Internet Support Groups for Depression: A 1-Year Prospective Cohort Study
Abstract
OBJECTIVE: This study described the characteristics of users of Internet-based depression support groups and assessed whether use predicts change in depression symptoms and social support. METHOD: Users (N=103) of these groups were recruited into the study cohort and followed prospectively. Demographic characteristics, support group use, depression care, score on the Medical Outcomes Study Social Support Survey, and score on the Center for Epidemiologic Studies Depression Scale (CES-D Scale) were assessed by Internet survey at baseline, 6 months, and 12 months. RESULTS: Users’ demographic characteristics included median age of 40 years, 78.6% women, and 56.3% unmarried. Most (86.4%) were currently depressed (CES-D Scale score >22). Over 50% of participants heavily used the support group (5 or more hours in 2 weeks), and 37.9% preferred online communication to face-to-face counseling. Social support scores were low, compared with those from other studies of primary care patients with depression. The overall follow-up rate was 81.6% at 6 or 12 months. During follow-up, 72.6% of responders still participated in the online group; 81.0% were still receiving face-to-face depression care. Heavy users of the Internet groups were more likely to have resolution of depression (CES-D Scale score ≤22) during follow-up than less frequent users, after adjustment for age, gender, employment, and baseline CES-D Scale score with logistic regression. Social support scores did not change during follow-up. CONCLUSIONS: Users had high depression severity scores, were socially isolated, and perceived considerable benefit from the group. Internet depression support groups warrant continued research regarding supplementation of face-to-face depression care.
In the early 1990s, Internet-based support groups—including newsgroups, message boards, and listservs—for specific medical conditions emerged (1, 2). An estimated 33 million Americans have used the Internet as a health resource (3). By 2000, Internet access had expanded to reach 41.5% of American households (4). Patient information and social support through local specialized computer networks have been successful in improving some intermediate patient outcomes in clinical trials involving Alzheimer’s caregivers (5, 6) and in patients living with AIDS (7) and cancer (8). In an AIDS trial, use of the computer-based communication system reduced self-reported isolation (7). In the earlier Alzheimer’s caregivers’ study (5), use of the system led to greater perceived confidence in the ability to care for family members.
Through the Internet, support groups can potentially reach a large number of individuals from a geographically diverse area. Internet-based peer support groups for depression have been founded by motivated individuals to provide information and support. However, the effect of the Internet on depression is controversial (9, 10). In a study of families, greater Internet use over a 2-year time period resulted in a decline in communication within the family and within the wider social circle (9). Because individuals in these families were not socially isolated or depressed at baseline, this study does not address the specific question of risks and benefits of Internet support for individuals with depression who may have limited social support. Despite nearly 10 years of patient participation in consumer-created, consumer-driven support groups, few quantitative studies have assessed the type and value of the support or the interface between these Internet resources and face-to-face care. More information concerning who uses these peer-led groups for depression treatment and the perceived value of these groups is needed.
We designed a prospective observational study of individuals who currently use Internet-based support groups. We used several research questions in this study related to the user’s social support, participation in depression health care services, and depression outcomes. First, we wanted to assess the interaction of Internet depression support group use and face-to-face depression care. We hypothesized that individuals might communicate information derived from the support group to their health care providers. Second, we hypothesized that users of Internet depression support groups may be potentially more socially isolated than other depressed individuals. Because prior studies have reported higher levels of Internet use associated with lower social support, we were concerned that higher levels of Internet-based depression support group use may be associated with worsening social isolation over time. Finally, because of the positive impact of computer-networked support in other conditions, our main hypothesis was that more frequent users of Internet-based depression support groups might have a greater resolution of their depressive symptoms than less frequent users.
Method
Design, Study Group, and Data Collection
We recruited individuals to participate in a prospective cohort study. After receiving approval of our consent protocol from the Johns Hopkins School of Medicine’s Joint Committee on Clinical Investigation, we contacted the “listmasters” (or leaders) of five support groups. Volunteer requests were posted on these depression support groups and also on the depression message boards at http://www.drkoop.com and http://www.delphiforums.com. After reading a description of the study through the e-mail volunteer request, participants were provided an electronic consent statement approved by the Joint Committee on Clinical Investigation. Because of concerns about privacy, the listmasters did not provide us with an exact count of the number of participants. Thus, we are unable to estimate the participation rate. Recruitment occurred over a 2-month period, and baseline questionnaires were sent at the end of the recruitment period. Thus, most participants had been involved in the group for at least 1 to 2 months before completing the baseline survey. Baseline and follow-up participant questionnaires, including information on potentially important covariates such as age, gender, marital status, education, and employment as well as scores on the Medical Outcomes Study Social Support Survey and the Center for Epidemiologic Studies Depression Scale (CES-D Scale), were distributed and returned through e-mail. To help us understand their experiences with depression care, support group users were asked to identify the number of years since their first diagnosis with depression; to describe the type, frequency, and quality of their face-to-face depression care; and to inform us if they had told their depression health care provider about participation in the Internet depression support group. Individuals who did not respond to the follow-up surveys were sent up to four e-mail reminders.
Use of the Support Group
At each assessment, users of the Internet depression support groups were asked to report the number of hours they spent interacting with the groups in the past 2 weeks. Individuals also rated the value of the support groups on a 5-point Likert scale and reported the types of support they received from the group. Finally, we asked participants which they would choose if they had to choose between daily interaction with others on the support groups or going for weekly face-to-face counseling sessions.
Outcomes
Our main outcome measure was resolution of depressive symptoms over time. The CES-D Scale (11), a 20-item survey assessing severity of depressive symptoms within the past week, was administered at each time point. The CES-D Scale is a well-validated instrument (11, 12). Computerized CES-D Scale screening is highly correlated with paper screening with the instrument (13). The CES-D Scale is useful as an anonymous screen because it does not include questions whose answers demand immediate action, such as suicidal ideation (13).
The most common cutoff for a positive CES-D Scale score is greater than 16, with sensitivity at this level ranging from 86% to 100% and specificity ranging from 53% to 84% in different samples (11, 14–16). A more stringent cutoff has been recommended because of concerns about the potentially high level of false positive rates (14, 17). These more stringent cutoffs have varied from a score of 20 to 27 (14, 17, 18). Instead of choosing a single arbitrary cutoff, we opted to create three cutoffs: definite resolution of depression (score of ≤16), likely resolution (score of 17–21), and possible resolution (score of 22–27).
Secondary outcomes included influence of use of Internet depression support groups on participation in face-to-face depression care. Also, at 1 year, individuals reported whether their experiences in the Internet depression support groups had influenced them to “ask my doctor a question” or to “make a change in medications.”
To measure changes in social support, the Medical Outcomes Study Social Support Survey (19), which assesses tangible, affective, and emotional support and positive social interactions, was administered at each time point. Items were rated on a 5-point Likert scale ranging from 1=none of the time to 5=all of the time. Original factor analysis of the survey indicated excellent reliability (Cronbach’s alpha ≥0.95) and strong internal validity (r=0.69–0.82) within each subscale (19).
Analysis
To test the hypothesis that higher level of participation in the Internet depression support groups at baseline predicted a higher rate of resolution of depression, we compared with chi-square tests the rate of resolution of depression among individuals with frequent use of the support group (5 or more hours per week) to those who less frequently used the support group. Logistic regression analysis was then used to adjust for possible confounding by age, gender, employment status, and baseline severity of depressive symptoms. Resolution of depression was defined as a CES-D Scale score ≤22 for the primary analysis. Other CES-D Scale score cutoffs were used in additional models to test the robustness of the findings. Separate models were also created to predict resolution of depression at 6 and 12 months.
We then compared item scores on the Medical Outcomes Study Social Support Survey with those from the Quality Improvement for Depression study (20), a study following 1,400 patients with major depression identified in primary care settings around the country. To explore the potential association of more frequent use of the Internet support group and worsening of social support over time, change in a summation score of the nine Medical Outcomes Study Social Support Survey items was used as the outcome in linear regression and adjusted for age, gender, marital status, and change in depression severity score.
Results
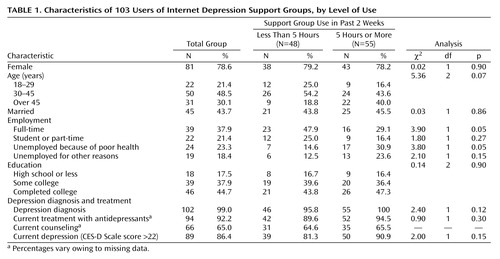
Overall, Internet depression support group users were mostly women with a median age of 40 years (Table 1). A high percentage of users (41.7%, N=43) were unemployed. The relatively high level of education in our cohort reflects the prevalent educational status among Internet users. Users were geographically dispersed, with participants representing 31 different states. Eighteen participants were from Canada, Australia, or Europe.
A total of 90.9% of more frequent users (N=50) reported current depression (CES-D Scale score >22), compared with 81.3% of less frequent users of the support group (N=39). All but two individuals had been diagnosed with depression by a health care professional. These two individuals both had CES-D Scale scores >22 and were thus included in the study group. Of the 103 participants, 96 were in treatment for depression at baseline. Most individuals had been treated with counseling (86.4%, N=89) or antidepressant medications (96.1%, N=99) in their lifetime. A total of 23.3% of the participants (N=24) were dissatisfied with their depression care.
Internet Support and Face-to-Face Care
In the previous 2 weeks, over one-half (53.4%) of the 103 Internet depression support group users (N=55) reported 5 or more hours of support group participation. Almost all users (95.1%, N=98) agreed that chatting on the Internet support groups helped their symptoms. Emotional support was the most popular reason to use the groups. Individuals also reported receiving information about medications (77.7%, N=80). When asked whether they preferred the Internet depression support groups to face-to-face counseling, 37.9% (N=39) said they preferred the group, 50.5% (N=52) preferred counseling, and 11.7% (N=12) reported no preference.
The overall follow-up rate was 81.6% (N=84) at 6 or 12 months, with 69.9% (N=72) at 6 months and 64.1% (N=66) at 12 months. Baseline characteristics, including demographic characteristics, depression severity, level of social support, and frequency of support group use, did not predict loss to follow-up. Of the 84 individuals with follow-up data available, 72.6% (N=61) were still participating in the Internet depression support groups at follow-up. Despite high use of the Internet depression support groups, most users did not abandon their face-to-face depression treatment over time, with 81.0% (N=68) still in routine depression care at the longest follow-up time (76.4% [55 of 72] at 6 months and 78.8% [52 of 66] at 1 year). Those without depression at baseline were more likely to have left face-to-face care (50.0%, six of 12) than those who had depression at baseline (13.9%, 10 of 72) (χ2=8.70, df=1, p=0.003). Among less frequent users of the support groups, 26% (N=10) abandoned face-to-face depression care during follow-up, compared with 13% (N=6) of the more frequent users (χ2=2.40, df=1, p=0.12).
At baseline, 71.8% of the users (N=74) reported that their depression care providers knew that they used the Internet depression support groups. At 1 year, participants were asked how the Internet depression support groups had influenced their face-to-face depression care. Of the 61 individuals who responded to this question, 62.3% (N=38) indicated that their experience in the Internet depression support groups had influenced them to “ask their health care provider a question,” and 26.2% (N=16) indicated the group had influenced them to “make a change in medications.”
Internet Support and Social Support
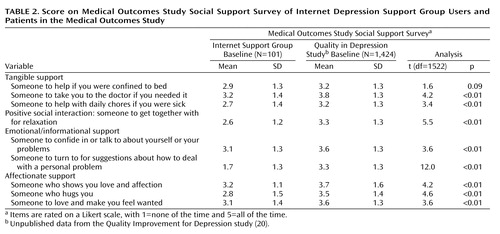
Uniformly, individuals in our cohort indicated lower levels of tangible, emotional, and affectionate support as well as positive social interactions compared with participants in the Quality Improvement for Depression study (Table 2). To aid the reader in interpreting the comparison between this group and the group in the Quality Improvement for Depression study we provide the following information. The 1,424 individuals in the Quality Improvement for Depression study sample were slightly older (mean age=44 years, SD=13) and less educated (22.0% [N=313] were college graduates); 47.0% (N=669) were married, and 62.0% (N=883) were unemployed (20). In addition, only 50.0% (N=712) of the Quality Improvement for Depression study sample had used antidepressants in the past 6 months. All of the subjects in the Quality Improvement for Depression study sample had a diagnosis of major depressive disorder, and only 28.0% (N=399) reported one episode of depression lasting less than 1 year (20). A relatively high percentage of the 103 online support group users reported “none at all” to the tangible support items on the Medical Outcomes Study Social Support Survey, including “someone to help if you were confined to bed” (18.4%, N=19), “someone to take you to the doctor if you needed it” (18.4%, N=19), and “someone to help with daily chores if you were sick” (25.2%, N=26).
We were concerned that face-to-face social support might continue to decay, especially among frequent users. With a summed scale of items from the Medical Outcomes Study Social Support Survey with a range of 9–45, the mean scores at baseline (score=26), 6 months (score=28), and 1 year (score=27) were unchanged. Using a t test of means, we found that Medical Outcomes Study Social Support Survey scores decreased by 2.5 (95% CI=–7.5 to 2.0) among more frequent users, compared with an increase of 1.3 (95% CI=–1.0 to 3.6) among less frequent users (t=1.4, df=72, p=0.15). In multivariate linear regression, change in social support scores did not differ over time between more frequent users of the Internet depression support groups and less frequent users, after adjustment for age, gender, marital status, and change in depression severity (B=–2.9; 95% CI=–8.01 to 2.20; t=–1.14, df=1, p=0.30). At 1 year, individuals reported that they received a mean of 26% to 50% of their social support through the Internet.
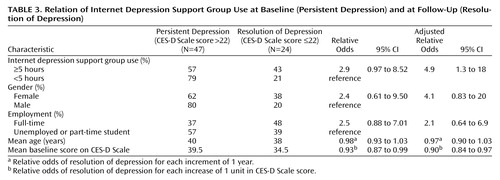
Internet Support and Depression Resolution
Among individuals with depression at baseline (CES-D Scale score >22) and follow-up data available (N=71), depression resolved (CES-D Scale score ≤22) in 33.8% of the subjects (N=24) at the longest follow-up time available. Depression resolved in 42.9% (18 of 42) of frequent users of the support groups at baseline (5 or more hours in the past 2 weeks), compared with 20.7% (6 of 29) of less frequent users (χ2=3.78, df=1, p=0.05). In multivariate analysis with logistic regression, more frequent users were again more likely to have resolution of depression than less frequent users (relative odds=4.9, 95% CI=1.3–18.0; likelihood ratio test χ2=6.53, df=1, p<0.03), after adjustment for age, gender, and baseline CES-D Scale scores (Table 3). We performed a subset analysis to examine the effect of the online support groups among individuals who were in counseling at baseline (N=67) compared with those who were not. Although our power was limited, we found no significant interaction between counseling and online support group use on the resolution of depression.
For the whole study group, 18.4% (N=19) and 46.6% (N=48) had resolution of their depression with a conservative cutoff (CES-D Scale score ≤16) and a more liberal cutoff (CES-D Scale score ≤27), respectively. With these alternate cutoffs, the association between resolution of depression and more frequent participation in online groups was no longer significant. The relative odds of depression resolution in comparisons of more frequent users to less frequent users were seen at 6 months (relative odds=2.7, 95% CI=0.7–10.0; z=1.53, df=1, p=0.13) and 12 months (relative odds=2.5, 95% CI=0.6–10.0; z=1.40, df=1, p=0.17), although power to find a relationship was again limited.
Discussion
We were successful in identifying 103 individuals participating in several online forums for depression peer support. Individuals participating in our study were chronically depressed and socially isolated. Almost all participants felt that interacting with these groups helped their symptoms, and over one-third preferred interacting on the Internet support group to face-to-face counseling. A potential concern is that individuals might neglect their face-to-face depression care in favor of the online environment. However, only seven of the support group users who still had depression (as measured by a CES-D Scale score >22) reported no longer being in treatment for depression during follow-up. It is surprising that most individuals told their health care providers about their online experiences. Some reported during follow-up that the online discussions had influenced them to become more active in their depression health care by asking their health care provider a question or helping to make a change in medications. Thus, although individuals in this cohort frequently used online support, they did not seem to leave their face-to-face care but used their online experiences to supplement face-to-face depression care.
Our hypothesis that individuals who chose to participate in online support groups may be a select group with low social support was confirmed. Individuals participating in online support groups had less social support than primary care patients with major depression (in the Quality Improvement for Depression study). These differences in social support are most likely mediated by other differences between these groups, including the prevalence of severe, chronic depression among Internet support group users. Among the comparison Quality Improvement for Depression study sample, individuals reported lower rates of use of antidepressant medications, were less chronically depressed, and were more likely to be married and employed. The significance of the social isolation impairment in the online users is best understood by the high percentage (18% to 25%) of individuals who reported no tangible social support. Although previous studies of Internet users have suggested an increase in social isolation over time, social support did not decline over time in our cohort (9). Unfortunately, the narrowed social support structure of these individuals also did not expand with time, even though their depressive symptoms improved.
Overall, a small number (33.8%) of individuals with depression at baseline resolved their depressive symptoms during follow-up. Individuals with depression at baseline who were more frequent users of the support groups were more likely to have resolution of their depression based on a cutoff score of 22. Using more conservative and more stringent cutoffs, we did not find a statistically significant association of resolution of depression with time spent on the online groups. In the context of previous success with controlled trials of networked computer support groups in cancer, AIDS, and Alzheimer’s disease, the relation of more frequent use of the depression support groups and more frequent resolution of depression suggests that these support groups may provide some therapeutic effect (5–7). Because our study was observational, a causal relationship cannot be determined. Although these results are interesting, randomized controlled trials should be performed to further define the benefit of Internet-based support groups for depression. In addition, we were not able to assess the beneficial effect of online support among those currently in counseling compared with those who were not in counseling. A hypothesis to test in future studies is whether individuals who are not currently in formal counseling have a greater benefit from online support group participation.
Potential advantages to online support for depression include accessibility by individuals from a wide geographic area who may not have easy access to groups in their community. Only one-third of our Internet support group users reported ever participating in a face-to-face support group. Individuals with embarrassing or stigmatizing conditions may also find the relative anonymity of the Internet gives them freedom to discuss their concerns more openly. Participants were asked to add personal anecdotes. Here is one example that pertains to the potential value of online anonymity:
I find online message boards to be a very supportive community in the absence of a “real” community support group. I am more likely to interact with the online community than I am with people face to face. This allows me to be honest and open about what is really going on with me. There are a lot of shame and self-esteem issues involved in depression, and the anonymity of the online message board is very effective in relieving some of the anxiety associated with “group therapy” or even individual therapy. I am not stating that it is a replacement for professional assistance, but it has been very supportive and helped motivate me to be more active in my own recovery program.
This study of Internet support groups for depression represents the first attempt to test the feasibility of recruiting and maintaining a prospective cohort completely through the Internet. The privacy that is valued among these online support groups presented challenges to our research design. Because the group moderators were unwilling to supply exact numbers of participants and because the number of people participating in a group varies from day to day, we were unable to quantify the level of participation bias. Our group may not be representative of all support group users—a limitation of this study. Individuals who are more active in the support groups were more likely to read our volunteer request. Thus, our group was potentially biased toward more frequent users. In addition, if frequent users are more likely to be socially isolated, our group may be skewed toward those with less social support. Despite adjustment, in observational studies there is always the possibility of residual confounding by factors, including age, gender, or severity of depression. Our results might have been affected by loss to follow-up. However, loss to follow-up was not associated with primary exposure, frequency of support group use, or severity of baseline depression symptoms. Because we did not collect other personal identifiers, such as telephone numbers and addresses, we were only able to collect self-reported data, and a small number of participants were lost because of changes in e-mail addresses.
In conclusion, individuals who participate in Internet depression support groups often report moderate to severe depression, with low levels of social support. Participants reported deriving considerable support from their online interactions, placed a high value on the support groups, and seemed to incorporate information from the online support groups into their relationship with their health professional. At the beginning of our study, these individuals reported significant social isolation, and this, unfortunately, did not improve over time. Lack of social support might mean a greater risk of recurrence of depressive symptoms. We found no evidence that more frequent users became more depressed at follow-up. More frequent use was associated with an increase in resolution of depression (CES-D Scale score ≤22), although this finding was not robust across multiple CES-D Scale score thresholds. Health providers caring for individuals with depression should explore their patients’ use of online support, both to understand the information individuals are receiving and to monitor the effect of these interactions on their depressive symptoms. Despite their potential, these online communities may also be improved by integration into face-to-face care with participation by health professionals or more training for the lay health workers leading these groups. Internet depression support groups offer an interesting alternative outlet for individuals with depression to increase their knowledge, self-help skills, and medical communication skills consistent with an active coping style that has been shown to predict resolution of depression (21). In future research, one might hypothesize that Internet-based peer support groups may be more helpful as an outlet for individuals who are not currently in counseling and are taking medications alone than for individuals already in professional counseling. However, before Internet-based depression support groups can be recommended, larger prospective studies and clinical trials should be performed to assess their impact on depression symptoms and social support.
 |
 |
 |
Presented in part at Partnerships for Networked Health Communication, Washington, D.C., Jan. 24–28, 2000. Received April 3, 2001; revisions received Sept. 21, 2001, and July 11, 2002; accepted July 24, 2002. From the Departments of Medicine, Epidemiology, Health Policy, and Management, School of Hygiene and Public Health, Johns Hopkins University School of Medicine, Baltimore. Address reprint requests to Dr. Ford, 2024 East Monument St., Suite 2-500, Baltimore, MD 21205-2223; [email protected] (e-mail). Supported by Association for Health Services Research training grant ZT32PE10025. Dr. Ford gave permission for the use of unpublished data from the Quality Improvement for Depression study.
1. Ferguson T: Health Online. New York, Addison-Wesley, 1996Google Scholar
2. Ferguson T: Health online and the empowered medical consumer. J Quality Improvement 1997; 23:251-257Crossref, Medline, Google Scholar
3. Miller TE, Reents S: The Health Care Industry in Transition: The Online Mandate to Change. New York, Cyber Dialogue, 1998Google Scholar
4. National Telecommunications and Information Administration: Falling Through the Net: Toward Digital Inclusion. Washington, DC, US Department of Commerce, 2000Google Scholar
5. Gallienne RL, Moore SM, Brennan PF: Alzheimer’s caregivers: psychosocial support via computer networks. J Gerontol Nurs 1993; 19:15-22Crossref, Medline, Google Scholar
6. Brennan PF, Moore SM, Smyth K: The effects of a special computer network on caregivers of persons with Alzheimer’s disease. Nurs Res 1995; 44:166-172Crossref, Medline, Google Scholar
7. Brennan PF, Ripich S, Moore SM: The use of home-based computers to support persons living with AIDS/ARC. J Community Health Nurs 1991; 8:3-14Crossref, Medline, Google Scholar
8. Gustafson DH, McTavish F, Hawkins R, Pingree S, Arora N, Mendenhall J, Simmons GE: Computer support for elderly women with breast cancer (letter). JAMA 1998; 280:1305Crossref, Medline, Google Scholar
9. Kraut R, Patterson M, Lundmark V, Kiesler S, Mukopadhyay T, Scherlis S: Internet paradox: a social technology that reduces social involvement and psychological well-being. Am Psychol 1998; 53:1017-1031Crossref, Medline, Google Scholar
10. Roberts N: Out of the doldrums on the net: surfing the Internet to break depression. New Statesman 1996; 127:24Google Scholar
11. Radloff LS: The CES-D Scale: a self-report depression scale for research in the general population. J Applied Psychol Measurement 1977; 1:385-401Crossref, Google Scholar
12. Schulberg HC, Saul M, McClelland M, Christy W, Frank R: Assessing depression in primary medical and psychiatric practices. Arch Gen Psychiatry 1985; 42:1164-1170Crossref, Medline, Google Scholar
13. Ogles BM, France CR, Lunnen KM, Bell MT, Goldfarb M: Computerized depression screening and awareness. Community Ment Health J 1998; 34:27-38Crossref, Medline, Google Scholar
14. McDowell I, Newell C: Depression, in Anonymous Measuring Health: A Guide to Rating Scales and Questionnaires. New York, Oxford University Press, 1996, pp 238-286Google Scholar
15. Parikh RM, Eden DT, Price TR, Robinson RG: The sensitivity and specificity of the Center for Epidemiologic Studies Depression Scale in screening for post-stroke depression. Int J Psychiatry Med 1988; 18:169-181Crossref, Medline, Google Scholar
16. Beekman AT, Deeg DJ, Van Limbeek J, Braam AW, De Vries MZ, Van Tilburg W: Criterion validity of the Center for Epidemiologic Studies Depression scale (CES-D): results from a community-based sample of older subjects in The Netherlands. Psychol Med 1997; 27:231-235Crossref, Medline, Google Scholar
17. Zich JM, Attkisson CC, Greenfield TK: Screening for depression in primary care clinics: the CES-D and the BDI. Int J Psychiatry Med 1990; 20:259-277Crossref, Medline, Google Scholar
18. Clark VA, Aneshensel CS, Frerichs RR, Morgan TM: Analysis of effects of sex and age in response to items on the CES-D Scale. Psychiatry Res 1981; 5:171-181Crossref, Medline, Google Scholar
19. Sherbourne CD, Stewart A: The MOS Social Support Survey. Soc Sci Med 1991; 32:705-714Crossref, Medline, Google Scholar
20. Rost KM, Duan N, Rubenstein LV, Ford DE, Sherbourne CD, Meredith LS, Wells KB: The Quality Improvement for Depression collaboration: general strategies for a coordinated study of quality improvement in depression care. Gen Hosp Psychiatry 2001; 23:239-253Crossref, Medline, Google Scholar
21. Sherbourne CD, Hays RD, Wells KB: Personal and psychosocial risk factors for physical and mental health outcomes and course of depression among depressed patients. J Consult Clin Psychol 1995; 63:345-355Crossref, Medline, Google Scholar



