The Psychosocial Treatment of Schizophrenia: An Update
Abstract
OBJECTIVE: The authors sought to update the randomized controlled trial literature of psychosocial treatments for schizophrenia. METHOD: Computerized literature searches were conducted to identify randomized controlled trials of various psychosocial interventions, with emphasis on studies published since a previous review of psychosocial treatments for schizophrenia in 1996. RESULTS: Family therapy and assertive community treatment have clear effects on the prevention of psychotic relapse and rehospitalization. However, these treatments have no consistent effects on other outcome measures (e.g., pervasive positive and negative symptoms, overall social functioning, and ability to obtain competitive employment). Social skills training improves social skills but has no clear effects on relapse prevention, psychopathology, or employment status. Supportive employment programs that use the place-and-train vocational model have important effects on obtaining competitive employment. Some studies have shown improvements in delusions and hallucinations following cognitive behavior therapy. Preliminary research indicates that personal therapy may improve social functioning. CONCLUSIONS: Relatively simple, long-term psychoeducational family therapy should be available to the majority of persons suffering from schizophrenia. Assertive community training programs ought to be offered to patients with frequent relapses and hospitalizations, especially if they have limited family support. Patients with schizophrenia can clearly improve their social competence with social skills training, which may translate into a more adaptive functioning in the community. For patients interested in working, rapid placement with ongoing support offers the best opportunity for maintaining a regular job in the community. Cognitive behavior therapy may benefit the large number of patients who continue to experience disabling psychotic symptoms despite optimal pharmacological treatment.
Antipsychotic medications have been repeatedly shown to be effective for the treatment of acute psychosis and the prevention of relapse for persons suffering from schizophrenia. Novel antipsychotics with fewer neuromotoric side effects are a clear therapeutic advancement. However, with the exception of clozapine for treatment-resistant psychosis, the newer agents have not been clearly shown to have clinical advantages in other domains of outcome, such as social adjustment and obtaining competitive employment (1). Thus, the majority of persons with schizophrenia, even those who benefit from medication, continue to have disabling residual symptoms and impaired social functioning and will most likely experience a relapse despite medication adherence. Hence, it is necessary to integrate empirically validated psychosocial treatments into the standard of care for this population.
In this article, we present an updated review of the various forms of psychosocial interventions that have been studied in methodologically sound clinical trials, with a special emphasis on studies published since the 1996 review by Penn and Mueser (2). Randomized controlled trials currently assess relevant outcomes in patients with schizophrenia beyond the traditional measures of psychopathology and rates of rehospitalization. Other domains of outcomes include cognitive performance, social skills and adjustment, overall quality of life, competitive employment, and comorbid substance abuse as well as less usual clinical measures such as negative, depressive, and deficit symptoms. As we describe different psychosocial interventions, we will define the primary targeted outcome measure addressed in each study. We will not address the important area of treatment research concerning schizophrenia and comorbid substance abuse (the reader is referred to the update by Drake and colleagues [3]).
Research into psychosocial treatment strategies exists at varying stages of development, some modalities having been studied more often and with better-designed randomized controlled trials. The majority of the randomized controlled trials reviewed assumed that optimal antipsychotic medication management was provided. From the available literature, whenever possible, we will address the following questions. What is the efficacy of the specific intervention for the primary outcome measure? For secondary outcomes? Is a particular kind of psychosocial intervention more efficacious for certain outcomes? (If so, what is the evidence for an “active ingredient”?). What evidence exists for effectiveness and transferability, i.e., effectiveness in more usual clinical settings? What data exist regarding cost-effectiveness?
Because family therapy is the most extensively studied psychosocial intervention, a reasonable attempt can be made to address most of these questions for this modality. For other forms of treatment, some of the questions may not be addressed because of limited data.
Method
We selected articles for review by conducting MEDLINE and PsychInfo computerized searches of the English language literature for the period 1966 to March 2000. For the MEDLINE searches, the following key words were used in conjunction with the terms “schizophrenia,” “randomized control trial,” and “human”: “psychotherapy,” “psychosocial rehabilitation,” “social adjustment,” “social support,” “cognitive therapy,” “family therapy,” and “social skills training.” From these searches, 155 separate references were found. For the PsychInfo searches, the following key words were used in conjunction with the terms “schizophrenia,” “empirical study,” “human,” and “journal articles”: “group psychotherapy,” “psychotherapy,” “family therapy,” “social adjustment,” “social skills,” and “cognitive therapy.” From these searches, 12 additional references not included in the initial MEDLINE search were identified. We primarily selected randomized controlled trials that used standardized rating instruments, but some pertinent less rigorously conducted studies were also included. We also checked the references in the articles obtained to ensure that other relevant articles that had not been identified with the initial searches were included, and we consulted some experts in the field in order to identify other recent studies.
Results
In total we identified 18 new studies since the review by Penn and Mueser (2): two for family therapy, two for case management, five for social skills training, three for supported employment programs, five for cognitive behavior therapy, and one for individual therapy (which also had a family therapy arm).
Family Therapy
Brown and Rutter (4) demonstrated, and Butzlaff and Hooley (5) have recently supported the concept, that schizophrenia patients who returned to families that were originally rated as being high in expressed emotion (an empirically derived index of criticism, overinvolvement, and hostility) were more likely to experience a relapse during the following year despite adequate pharmacotherapy. Although high expressed emotion environments are not specific to families of patients with schizophrenia (5), the expressed emotion literature provided the background for most of the initial randomized controlled trials of family therapy that attempted to reduce psychotic relapse.
Efficacy with regard to primary outcome
A large body of evidence has demonstrated the superiority of a variety of family therapy interventions that employ behavioral and psychoeducational techniques over customary outpatient care or individual therapy in terms of the primary outcome measures of psychotic relapse and rehospitalization (2). On average, relapse rates among schizophrenic patients whose treatment involves family therapy are approximately 24% as compared to about 64% among those who receive routine treatment (6). Additionally, the beneficial effects of long-term family interventions (i.e., greater than 9 months) appear to be quite durable and may be maintained for up to 2 years (6) or longer (7).
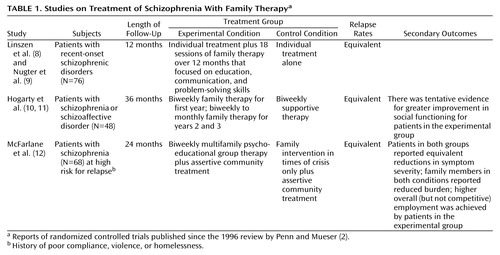
However, the few studies published since the 1996 review by Penn and Mueser (2) are remarkable for their lack of relapse prevention findings (Table 1). Linszen and colleagues (8, 9) studied adolescent patients early in their illness and found a very low (16%–20%) overall relapse rate at 1 year, with no advantage for the patients whose treatment included family therapy. It is worth noting that the comparison intervention involved a fairly intensive individual treatment approach rather than “standard” services. The personal therapy trial of Hogarty et al. (10) included a family therapy arm for patients residing with their families. Unlike the subjects in the previous study, these subjects were mostly chronic patients. Family therapy offered no advantage over supportive therapy in preventing relapse (the overall relapse rate was only 29% at 3 years). The supportive therapy group received biweekly sessions, minimum effective medication dosage, and case management—an enriched package of care compared to most community standards. These studies illustrate that if the base relapse rate is low (either because of the population selected or the use of a comprehensive control care program), the potential advantages of family therapy may not be realized.
Are some interventions more efficacious?
Considerable attention has focused on the reduction of expressed emotion levels as an active mediator for the efficacy of family therapy interventions. In studies that selected families with high levels of expressed emotion, patients who did not experience a relapse were more likely to reside in a family household in which the expressed emotion environment had changed from high to low during the treatment (13–16). However, the number of subjects/families reassessed was very small, and there were no reports of a clear correlation between relapse and reductions in expressed emotion levels. Because it is possible that a high level of expressed emotion may be a consequence of the relapse itself (or of patients being more severely ill), proving a causal role of expressed emotion for psychotic relapse requires a controlled study that includes interim expressed emotion assessments. Only Tarrier et al. (16) assessed expressed emotion levels at baseline, 4.5 months, and 9 months. Although they found that the level of expressed emotion changed from high to low in the relatives in the experimental treatment, similar changes occurred for the control condition. They concluded that “…this latter result would not be expected if expressed emotion is a stable dimension with a simple causal role in relapse” (16, p. 540).
Direct comparisons of two forms of family treatment (with one usually more intensive than the other) have failed to demonstrate differential efficacy for the experimental intervention (16–20). Because these studies did not include a no-treatment group, interpretations regarding the efficacy of the different forms of family therapy are problematic. However, the reported relapse rates at 2 years for these studies were low (under 36%) and comparable to the rates reported in previous comparison studies of active family intervention versus standard treatment (between 14% and 33% versus 40%–83%, respectively) (6). This suggests that in studies comparing two forms of family treatment, both interventions were efficacious.
McFarlane et al. (12) studied schizophrenia patients at high risk for relapse (Table 1). Half received biweekly multifamily group treatment, and half received family therapy only during times of crisis. There were no differences in relapse for the two treatment groups (27% at 2 years). Thus, research has failed to identify the relative superiority of any particular form of family therapy and suggests that treatment intensity (i.e., beyond moderate intensity with sustained availability) or format does not differentially effect outcome.
Efficacy with regard to secondary outcomes
Some studies have reported improvement in such factors as family burden, coping, and knowledge of schizophrenia (12, 21–23). However, these studies do not separate the effect that reduced relapse rates due to the family therapy intervention might have on these other outcome measures. The effect on social functioning independent of the effect on relapse has been assessed in two studies (11, 20) in which relapsed subjects reentered their original treatment group once stabilized. Social functioning was assessed between relapse episodes. Neither study found an advantage in social functioning for the experimental family treatment group (11 and Mueser, personal communication, 1999).
Effectiveness and transferability
Many randomized controlled trials have employed treatment manuals to guide the family therapy, which would facilitate implementation in alternate settings. The model of Falloon et al. (13) (behaviorally oriented problem-solving in the home) has been repeatedly transferred to other research settings (8, 9, 20, 24). Unfortunately, the evidence for effectiveness in a more typical nonresearch setting is very limited, primarily because family therapy has not become the standard of care in the community (25). Some studies from China show that a relatively simple psychoeducational approach can be implemented in the community with large numbers of patients and have an important effect on relapse (23, 26, 27). However, the control condition in these studies (usual care) failed to include scheduled medication management follow-up (clearly suboptimal care by Western standards). Therefore, it is not surprising that the family management groups (which encouraged family members to actively pursue medication follow-up) had substantially better outcomes (relapse rates of 15%–44% versus 31%–64%, respectively). These Chinese studies also suggest that cultural differences are not necessarily an impediment to successfully applying existing family therapy interventions to diverse cultural groups. However, Telles et al. (28) applied the model of Falloon et al. (13) to a group of Hispanic families and found no differences between behavioral family therapy and standard treatment. Thus, the impact of more complex models of family treatments to non-Caucasian cultures is unclear.
Cost-effectiveness
Although a large effect of family therapy on prevention of relapse and rehospitalizations could potentially result in important cost savings, only a few studies report cost-benefit analyses. In an analysis that compared home-based family treatment versus individual management over a 12-month period, Cardin et al. (29) reported that the total costs of family management were 19% less than those of individual treatment, with overall benefits favoring the family therapy intervention. Tarrier et al. (30) documented a favorable cost-benefit ratio for patients from high expressed emotion environments who received a 9-month family therapy intervention as compared to a control group from high expressed emotion environments who received routine treatment. Despite the extra costs associated with therapist time, the family therapy intervention resulted in a mean cost savings of 27% per patient. The study by Xiong et al. (26) reported significant cost savings associated with family therapy ($170 per patient per year, a large savings by contemporary Chinese standards). However, as stated before, a replication study that applies Western standards of community care is required.
Case Management
Patients with schizophrenia are often ill-prepared to find and maintain the multiple services they need in order to function in the community. Traditionally, case managers have functioned as brokers of services, being contacted by other professionals who have identified a new need for the patient and then referring the patient to the provider able to deliver these services. Unfortunately, many patients with schizophrenia lack the level of cognitive and social competence to consistently follow-through and get their needs met, which further increases their risk of relapsing.
A different approach to case management and service delivery is exemplified by the assertive community treatment program (31). Patients are assigned to one multidisciplinary team (case manager, nurse, etc.). The team has a fixed caseload and a high staff/patient ratio and delivers all services when and where needed by the patient, 24 hours a day, 7 days a week. Mueser et al. (32) reviewed the literature on assertive community treatment programs for patients with chronic mental illness, and two more randomized controlled trials have since been published (33, 34). There are now 32 studies of assertive community treatment programs with a true experimental design.
Efficacy with regard to primary outcome
The main goal of assertive community treatment programs is to prevent rehospitalization in patients at risk for relapse through provision of comprehensive integrated community services. The most consistent effects have been a reduction of time spent in the hospital (demonstrated in 14 of 24 studies; nine reported no differences) and an improvement in housing stability (demonstrated in nine of 13 studies; four reported no differences) (32–34). These effects are clinically meaningful and more robust among patients with high service utilization rates. It is of interest that the two most recent studies (33, 34) did not find an effect on rehospitalizations. Both studies included an intensive clinical case management approach as a control treatment and did not provide 24-hour coverage as a component of assertive community treatment. Also, Issakidis et al. (34) did not restrict subject inclusion to those who were high service utilizers (only one-third of their study group were high service utilizers). These characteristics may explain the negative findings.
Efficacy with regard to secondary outcomes
Only a minority of studies have found advantages in social adjustment (four of 16) or employment (three of nine, and these jobs represented mostly sheltered rather than competitive employment) (32–34). The disappointing effects on functioning are perhaps accounted for by the emphasis of assertive community treatment in directly assisting patients with their immediate needs, without a formal component of rehabilitation directed toward either social or vocational skills. If a reasonable goal for some patients is self-sufficiency, more systematic efforts aimed at rehabilitation may need to be incorporated into assertive community treatment.
Are some interventions more efficacious?
In general, programs that more closely resemble the original assertive community treatment model tend to have a more reliable effect on rehospitalization (35). However, because assertive community treatment is so complex and there have been no studies that systematically assess the impact of each component, it is not known which components are essential. Hence, the effect on hospitalization could be due to improved medication compliance, continuity of caregivers, 24-hour coverage, site of service, intensity of services, or a combination of some of these elements.
Effectiveness and transferability
The original assertive community treatment program has been successfully transferred to many communities by other teams of clinical researchers. Also, assertive community treatment programs have been successfully implemented as part of routine clinical care and have been shown to be effective at reducing rehospitalizations (36).
Cost-effectiveness
In patients with high service utilization rates, assertive community treatment may result in some net savings, since expensive inpatient treatments are reduced by employing less costly community services (31, 37). Rosenheck and Neale (36) documented the cost savings associated with assertive community treatment compared to the cost of standard care at a Veterans Administration (VA) facility, but only for the sickest of the high inpatient service users who were treated at neuropsychiatric hospitals. However, a recently published analysis (38) of a previous study (33) that compared assertive community treatment with another high-quality case management system that did not use multidisciplinary teams with constant availability did not support the cost savings advantages of assertive community treatment.
Social Skills Training
Social skills are those “…specific response capabilities necessary for effective social performance” (39). Social skills training uses learning theory principles to improve social functioning by working with patients to remediate problems in activities of daily living, employment, leisure, and relationships. It is hoped that the improved skills (primary outcome) will generalize to better community functioning and have a downstream effect on relapse and psychopathology. Following the framework described by Bellack and Mueser (39), there are three forms of social skills training: the basic model, the social problem-solving model, and the cognitive remediation model.
In the basic model, complex social repertoires are broken down into simpler steps, subjected to corrective learning, practiced through role playing, and applied in natural settings. The social problem-solving model focuses on improving impairments in information processing that are assumed to be the cause of social skills deficits. The model targets domains needing changes including medication and symptom management, recreation, basic conversation, and self-care. Each domain is taught as part of a module, with the purpose of correcting deficits in receptive, processing, and sending skills. In the cognitive remediation model, the corrective learning process begins by targeting more fundamental cognitive impairments, like attention or planning. The assumption is that if the underlying cognitive impairment can be improved, this learning will be transferred to support more complex cognitive processes, and the traditional social skills models can be better learned and generalized in the community.
Efficacy with regard to the primary outcome
The basic model has been repeatedly demonstrated to have an effect on improving specific social skills, and this learning is maintained for up to 12 months (2). However, the outcomes measured in most of these studies closely resembled those assessed in the skills training setting, and there is little evidence that this learning translates into improved social competence in the community (40). In the most extensive study of the basic social skills training model, Hogarty et al. (41) failed to demonstrate a significant impact on social adjustment after 2 years of treatment, despite a very intensive intervention (1 hour weekly for 21 months plus medication compared to medication only). The lack of generalization in this study and others that used the basic model has been a significant limitation.
The social problem-solving model has also demonstrated an effect on skill enhancement (42–44). Two studies have examined the long-term impact of this model. Marder et al. (45) assigned schizophrenic outpatients to problem-solving group therapy or supportive group therapy for 2 years. Both groups received the same intensity, frequency, and overall length of intervention (90 minutes twice weekly for the first 6 months, then weekly). There was a small but statistically significant advantage for the problem-solving intervention in two out of six measures of social adjustment after 2 years. Thus, the experimental treatment had modest benefits.
Liberman et al. (46) compared the problem-solving group model to equally intensive occupational therapy. Subjects received the psychosocial interventions for 6 months (3 hours a day, four times a week) and were followed for 2 years. The experimental condition had a significant effect in three out of 10 independent living skills (more personal possessions, more skilled food preparation, and improved money management) that were maintained up to 18 months after completing the intervention. The authors posited that the effect on independent living skills suggests generalization of skills learned and attributed this effect to the fact that all subjects were assigned a case manager who actively encouraged them to apply the skills learned in the community.
Although initial studies of the cognitive remediation model demonstrated some improvement of elementary cognitive processes (47), studies that have evaluated more complex cognitive and social skills have provided mixed results. Hodel and Brenner (48) failed to find in a program that started with cognitive remediation before skills training (N=10) the predicted advantage on social adjustment over a program that followed the opposite order (N=11). Wykes et al. (49) found that 17 patients treated with an intensive cognitive remediation approach (1-hour daily sessions for up to 3 months) that targeted executive functioning deficits showed improvement on three of 12 cognitive measures as compared to 16 patients who received a comparison intervention (occupational therapy) matched for therapist contact and treatment duration. The cognitive remediation intervention did not result in any direct improvements in social functioning or symptoms.
A recent report by Spaulding et al. (50) from their large study (total N=90) comparing cognitive remediation plus the social problem-solving modules with equally intensive supportive therapy plus the modules presents a more hopeful outlook. Subjects were very ill, mostly with schizophrenia, and were referred for long-term hospital treatment because of inability to sustain community living. The experimental and control interventions were matched for intensity (3 hours per week for 6 months). The cognitive remediation group did better in two out of four measures of social competence and demonstrated better acquisition of skills for two out of four of the social problem-solving modules. This study suggests that the cognitive remediation approach can enhance response to more standard skills training in very ill, institutionalized patients.
Efficacy with regard to secondary outcomes
The study by Hogarty et al. (15, 41) is the only large social skills training study to find an effect on relapse prevention (46% for social skills training versus 30% for the control condition after 1 year), but there is an important caveat to this finding: the relapse prevention effect was lost in the second year, 3 months after the social skills training was reduced from weekly to biweekly. Thus, it is not clear whether the effect on relapse was due to the higher patient contact rather than a specific advantage of social skills training. Two studies that used the social problem-solving model (45, 46) and controlled for the nonspecific effects of patient contact failed to find an effect on relapse prevention, which suggests that some nonspecific aspects of social skills training (e.g., improved symptom monitoring) may reduce relapse rates. For other outcomes such as psychopathology and employment there have been no consistent effects reported for any of the social skills training modalities.
Effectiveness and transferability
The problem-solving model has been standardized into well-defined modules with printed manuals, making it easy to transfer to other settings. In a pre-post design, Wallace et al. (51) documented learning of skills in seven nonresearch settings as implemented by regular staff trained through a 2-day workshop. The study by Liberman (46) also documented the effectiveness of intervention implemented by paraprofessionals in a typical VA clinical setting.
Vocational Rehabilitation
Competitive employment (holding a regular community job as opposed to being employed in a program overseen by a rehabilitation agency) has been estimated at less than 20% for severely mentally ill persons and is probably lower for patients with schizophrenia (52). In an effort to keep patients as functional and autonomous as possible in the community, various programs have been implemented to help patients find jobs and maintain them. Supported employment programs, the most recent approach to enhancing outcomes beyond those associated with traditional vocational rehabilitation (like transitional or sheltered employment), aims to improve opportunities for competitive employment.
The implementation of supported employment programs differs along a number of dimensions. However, several common components across models may be identified, including a goal of permanent competitive employment, minimal screening for employability, avoidance of preoccupational training, individualized placement (i.e., not enclaves or mobile work crews), time-unlimited support, and consideration of client preferences (53).
Efficacy with regard to the primary outcome
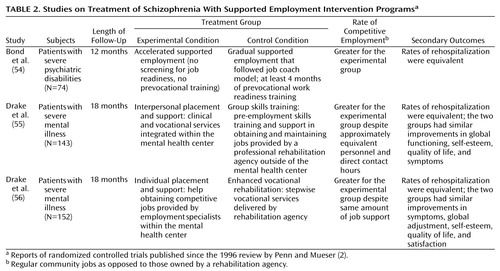
We identified three randomized controlled trials for supported employment programs (54–56) that had competitive employment as the primary targeted outcome (Table 2). The results were consistent in demonstrating significant advantages for supported employment programs over control interventions. The unweighted mean among patients in supported employment programs for obtaining competitive employment was 65% (range=56%–78%), whereas the corresponding rate for patients in the control conditions was 26% (range=9%–40%). Thus, in contrast to traditional vocational-rehabilitation approaches, these results provide encouraging evidence for the efficacy of supported employment programs in terms of increasing rates of competitive employment.
These positive results must be interpreted in light of the small number of trials that have been conducted and a number of methodological limitations (described in detail by Bond et al. [53]). Retention is a particularly important issue to consider, since dropout rates over 40% are not uncommon (53). Although supported employment programs appear to be efficacious in helping patients attain entry-level positions, there are no data to evaluate whether supported employment programs confer longer-term benefits for patients who may be capable of progressing beyond these positions. For patients who have poor work histories and limited premorbid skills (perhaps the majority of persons with schizophrenia), attainment of entry-level positions may be a reasonable outcome.
Efficacy with regard to secondary outcomes
Supportive employment programs do not appear to result in benefits for nonvocational outcomes (Table 2). For example, despite the belief that employment may produce such secondary benefits as improved self-esteem, improved quality of life, and reductions of symptoms and relapses, the studies reviewed provide little to no evidence to support these assumptions. However, it is possible that employment per se, apart from the vocational rehabilitation strategy implemented, could lead to improvement in other outcomes (57).
Are some interventions more efficacious?
Drake et al. (56) compared two types of supported employment interventions, one with early placement plus integration of vocational and mental health services (interpersonal placement and support) and the other with initial training and later placement (and no integration of services). The interpersonal placement and support group achieved higher rates of competitive employment, but it is not clear whether the effect was due to early placement or integration of services.
Effectiveness and transferability
The efficacy of interpersonal placement and support, which was originally demonstrated in two small cities in New Hampshire (55), was subsequently replicated in a Washington, D.C., patient group with a very different ethnic composition (83% African American) (56). These results provide some evidence that supported employment programs are transferable to urban settings and to diverse ethnic and socioeconomic populations. Additionally, Drake et al. (56) documented the effectiveness of supported employment programs compared to standard vocational services available in the Washington, D.C., area. The availability of a treatment manual for interpersonal placement and support (58) should facilitate research into the transferability of this treatment modality.
Cognitive Behavior Therapy
Over the past decade, there has been a growing interest in applying cognitive behavior therapy techniques to persons with schizophrenia, particularly those who continue to experience psychotic symptoms despite optimal pharmacological treatment. The principal aims of cognitive behavior therapy for medication-resistant psychosis are to reduce the intensity of delusions and hallucinations (and the related distress) and promote active participation of the individual in reducing the risk of relapse and levels of social disability. Interventions focus on rationally exploring the subjective nature of the psychotic symptoms, challenging the evidence for these, and subjecting such beliefs and experiences to reality testing.
Efficacy with regard to the primary outcome
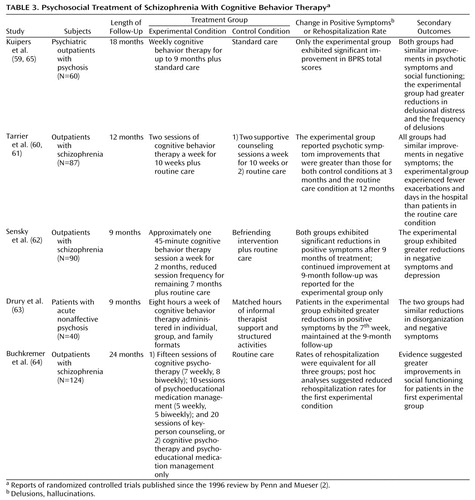
We identified five randomized controlled trials of cognitive behavior therapy for the treatment of psychotic symptoms as compared to standard or control treatment in patients with chronic psychoses (Table 3). For four of these studies, a reduction in delusions and hallucinations was the primary targeted outcome; one trial targeted reduced rehospitalization rates.
Three studies examined the effects of cognitive behavior therapy on medication-resistant psychotic symptoms in schizophrenic outpatients and included follow-ups of up to 1 year posttreatment. Kuipers et al. (59) found that patients receiving cognitive behavior therapy demonstrated a significant reduction in overall symptoms as compared to standard treatment alone but did not find a specific reduction in psychotic symptoms.
Tarrier et al. (60) found a reduction of delusions and hallucinations with cognitive behavior therapy compared to supportive counseling (of equal intensity) and routine care alone. The effects were clinically meaningful: 11 out of 33 of the patients treated with cognitive behavior therapy had reductions in delusions and hallucinations of at least 50% (compared to four out of 26 subjects who received supportive counseling). A particular effort was made in this study to ensure that symptoms were rated blindly. The advantage for cognitive behavior therapy was maintained at 12-month follow-up (61). A methodologically rigorous study by Sensky et al. (62) found that patients treated with cognitive behavior therapy or a befriending intervention (of equal intensity) plus routine care both experienced a reduction of psychotic symptoms following 9 months of treatment. At the end of treatment, there were no advantages for cognitive behavior therapy. However, at 9-month follow-up the treatment gains were sustained in the cognitive behavior therapy group but were not in the comparison condition. These studies suggest that the therapeutic benefit of cognitive behavior therapy is not simply attributable to nonspecific benefits of a psychological intervention.
In acutely psychotic inpatients, Drury et al. (63) found that cognitive behavior therapy adjunctive to antipsychotic medication resulted in a significantly faster and more complete recovery from the psychotic episode. At 9-month follow-up, 95% of the patients in the cognitive behavior therapy group reported no or only minor hallucinations or delusions as compared to 44% of patients in the control condition. A limitation of this study was that the raters of psychopathology also provided the experimental treatment.
Buchkremer et al. (64) compared four programs of care (two that included cognitive behavior therapy) to routine care. The interventions were delivered over 8 months and were assessed after 1 and 2 years of follow-up. The predicted reduction in rehospitalizations with cognitive behavior therapy was not found, but the group that received the most intensive intervention (cognitive behavior therapy plus individual and family psychoeducational psychotherapy) showed a trend toward fewer hospitalizations. In addition, cognitive behavior therapy failed to demonstrate an effect on psychotic symptoms.
Overall, the few available randomized controlled trials provide some preliminary evidence for the efficacy of cognitive behavior therapy in reducing delusions and hallucinations in medication-resistant patients and for its use as a complement to pharmacotherapy in acute psychosis.
Efficacy with regard to secondary outcomes
Cognitive behavior therapy failed to improve social functioning (59, 65) or relapse rates (60), both of which have been targeted outcomes in medication-resistant patients. Studies that have reported negative symptom effects have generally not found significant improvements associated with cognitive behavior therapy (60, 63, 64). However, the recent study by Sensky et al. (62) reported improvements in negative and depressive symptoms that were sustained up to 9 months following completion of treatment. A brief cognitive behavior therapy intervention based on motivational interviewing techniques that targeted compliance with antipsychotic medication showed significant improvements in compliance and patient attitudes toward drug treatment and insight into their illness as compared to standard treatment (66). However, the effects of this intervention were not translated into improvements in social functioning or symptoms.
Are some interventions more efficacious?
Only one study has compared two forms of cognitive behavior therapy for medication-resistant psychotic symptoms. Tarrier et al. (67) found that coping strategy enhancement or problem-solving interventions both led to targeted reductions in psychotic symptoms, with no between-group differences. The lack of a no-treatment group limits conclusions that may be drawn regarding “active ingredients.”
Cost-effectiveness
Kuipers et al. (65) reported some evidence that the monthly cost per patient was not higher for the cognitive behavior therapy group (£ 958) than for the standard treatment (£ 1,139) during an 18-month follow-up period. Because of the small study group size, this difference did not reach statistical significance.
Individual Therapy
Before the 1960s, individual psychoanalytically oriented therapy was considered by many the optimal treatment for schizophrenia. Following the negative findings in the landmark studies of May et al. (68) and Gunderson et al. (69), psychoanalytically oriented individual psychotherapy for most patients with schizophrenia has been practically eliminated in the United States. Only recently has a different form of intensive individual treatment been examined.
Hogarty et al. (10, 11) compared individual personal therapy for schizophrenia to family therapy, combined treatment, and supportive therapy in a 3-year trial. Personal therapy was conducted weekly (for 30 to 45 minutes) following an incremental approach individualized for the patients’ stage of recovery: the initial phase focused on the relationship between stress and symptoms; the intermediate phase emphasized learning to use relaxation and cognitive reframing techniques when stressed; the advanced phase (which generally started 18 months into treatment) focused on seeking social and vocational initiatives in the community and applying what was learned in personal therapy.
For the primary outcome measure of relapse prevention, personal therapy was no different than the other conditions. However, the personal therapy group was clearly favored in a composite measure of social adjustment (with an effect size that was over twice as large as that seen with non-personal-therapy), with the greatest differential improvement occurring in the last 2 years. Adjustment data were derived from various sources: patient interview, therapist assessments, and relatives’ perception, which argues for its validity. Limitations were that 40% of the patients assigned to personal therapy did not move on to the advanced phase of the treatment, and adjustment ratings were not blind to treatment conditions.
Conclusions
Summary of Findings
Over the last 4 years, research on psychosocial treatments for schizophrenia has continued to develop. We reviewed randomized controlled trials with a special emphasis on those published since the last update by Penn and Mueser (2). For the more extensively studied interventions (family therapy and assertive community treatment), the recent studies have had largely negative findings (8–10, 12, 33, 34). In our view, this does not so much put in doubt the large body of research supporting the efficacy of these treatments but rather is consistent with the level of evolution of research into these modalities. These findings reflect more sophisticated studies of either special populations (e.g., patients very early in their illness [8, 9]) or inclusion of enriched packages of care as control conditions (10, 12, 33, 34). In contrast, studies of two relatively new modalities, supported employment programs (54, 56) and cognitive behavior therapy (59–64), have shown mostly positive findings. Also, the few social skills training studies of interventions designed to increase generalization of skills (the social problem-solving [45, 46] and cognitive remediation models [50]) have reported promising results.
On the whole, the literature is consistent in that the various interventions have been largely successful for the primary outcome measures they were designed to target (i.e., family therapy and assertive community treatment for prevention of psychotic relapse and rehospitalization, social skills training for learning specific social behaviors, supported employment programs for obtaining competitive employment, and cognitive behavior therapy for reducing delusions and hallucinations). However, these effects tend to be domain specific and do not result in improvements in other clinically important secondary outcomes. For some interventions, this lack of an effect on other measures is not a serious limitation. With supported employment programs, attainment of competitive employment is clearly worthwhile, regardless of a limited effect on social adjustment or psychopathology. Likewise, with cognitive behavior therapy, reduction in the distress associated with psychotic symptoms is a highly desirable outcome, especially when other available treatments have failed. However, for the social skills training modalities, even if learning of skills is robust in most patients and can be maintained over time with relatively few resources, demonstrating some degree of generalizability and improved community functioning is crucial. Direct demonstration of use of learned skills in the community is a daunting methodological challenge yet to be accomplished.
The identification of “active ingredients” for different interventions has had very limited success. Beyond the general advantage of sustained over brief interventions in terms of primary outcomes, little is known regarding the specificity of the various treatments. Even for family interventions, the construct of “expressed emotion” has not been clearly shown to underlie the efficacy for relapse prevention. Also, when two forms of family interventions are compared, the literature is consistent that no advantages are evident. Similarly, recent studies of assertive community treatment suggest that “more is not necessarily better” and that for many patients, even those with high relapse rates, high-quality clinical case management with adequate service availability is equally effective. Because the effects of these interventions are mainly on relapse prevention, in populations of patients in which the base rate of relapse is already low (such as medication compliant persons early in their illness), there may be no advantage of adding family therapy, as the most recent studies suggest. With novel antipsychotic medications becoming the standard of care, compliance will hopefully improve, and relapse rates may be lowered; this could result in the amelioration of the effects of family treatment and assertive community treatment programs on relapse.
Transferability of efficacious treatments to more usual clinical settings has been documented for only a minority of interventions (like assertive community treatment and perhaps the social skills training problem-solving model). Cost-effectiveness has been documented for assertive community treatment when compared to usual community care but not when compared to another high-resource model of clinical case management.
Future Research
For the newer interventions such as supported employment programs, cognitive behavior therapy, cognitive remediation, and personal therapy, replication of the initial positive findings is necessary in large samples, in different settings, and by investigators not directly involved in the development of these treatment modalities. For family interventions and assertive community treatment, future research should concentrate on 1) identifying the minimal intensity of services that will maintain the relapse-preventing effects and 2) examining whether some subgroups of patients may benefit in particular. In the services research arena, it is necessary to demonstrate whether assertive community treatment programs effective in the community result in cost savings. Likewise, studies are needed of the cost-effectiveness of sustained psychoeducational family interventions added to adequate standard care.
Since effective interventions tend to be domain specific, it is important to investigate when to apply particular treatments. Because the majority of patients will relapse, sustain deficits in social competence, and fail to attain competitive employment (and many will experience persistent psychosis), research is needed to guide the optimum sequencing and combination of specific services to be delivered. For example, should social skills training precede, follow, or be implemented concurrently with cognitive behavior therapy in patients with persistent psychosis and limited social skills? And for what subgroups of patients and at what stage of the illness should a particular intervention be implemented?
For the supported employment approach, future studies should address the issue of the extent of ongoing support required to maintain efficacy and changes in the social security disability system such as retention of benefits despite competitive employment that might foster these vocational gains.
Finally, because of the continued development of newer and hopefully better antipsychotic agents, the interactions between different psychosocial and pharmacological modalities should be investigated. We are aware of only two (20, 45) randomized trials that controlled the psychosocial as well as the pharmacological intervention (neither involved novel antipsychotic agents). One study (45) found an interaction between psychosocial and pharmacological treatments, which suggested that the problem-solving social skills training approach may provide protection against relapse among patients suboptimally medicated. The other study (20) found no interaction between two forms of family treatment and three antipsychotic medication dose regimens.
Clinical Recommendations
What implications can be drawn for the use of the psychosocial interventions described in this review, for the standard of care for persons suffering from schizophrenia? For frequent relapsers who reside with family, a relatively simple but sustained psychoeducational family approach should be offered (for example, monthly visits in a single or multifamily group setting). Additionally, for the majority of patients, the family should be viewed as a natural ally that can provide crucial early information regarding relapse, substance abuse, community functioning, and compliance. For patients with high service utilization rates, assertive community treatment programs should be considered, especially if family involvement is not available. With the large majority of schizophrenia patients living in the community and hospital stays becoming progressively shorter as a result of managed care, a comprehensive system of delivery of services based on assertive community treatment principles will continue to be necessary for a large proportion of patients.
Once stable community living is achieved, a systematic rehabilitation effort for the majority of persons with schizophrenia is necessary. Beyond allowing patients to make use of previously learned social skills once the psychotic process is sufficiently controlled, there is no compelling evidence that medications (even the novel drugs) offer additional benefits in terms of social competence (1). Specific strategies to teach social skills are available. Of these, the social problem-solving model not only has resulted in the acquisition of skills but also is the approach with some evidence that suggests generalization of skills to community functioning and of effectiveness in more routine clinical settings. The requirement of social skills training for clinicians specifically trained in these techniques presently limits their use, but the availability of printed manuals with well-defined modules targeting different areas of social functioning is a fundamental step towards disseminating these interventions.
Patients who wish to work should be referred to a vocational rehabilitation agency with resources for supported employment. No other psychosocial or pharmacological treatment has been shown to promote competitive employment. However, for many patients a traditional sheltered form of employment or no employment will remain the best option. Because presently there is no evidence to identify these patients in advance, the majority of persons suffering from schizophrenia should be offered the supported employment approach when available.
A large number of patients will continue to experience disturbing delusions and hallucinations despite the best available medications. Persistent symptoms after an adequate trial with one antipsychotic agent generally predict little response to other medications. Superiority for previously resistant psychotic symptoms has been demonstrated only for clozapine (1), but a recent meta-analysis of efficacy for this agent suggests that the effects, although important, are smaller than originally found (70). Therefore, the results from cognitive behavior therapy interventions are particularly encouraging. Currently, these strategies are in their infancy, there are few clinicians with the expertise to implement them, and it is not clear that even in the best hands these strategies will result in clinically meaningful sustained effects. Nevertheless, cognitive behavior therapy has become established for the treatment of depressive and anxiety disorders and may prove to be a valuable resource for clinicians helping persons with chronic psychotic disorders as well.
 |
 |
 |
Received Feb. 1, 2000; revision received May 26, 2000; accepted June 5, 2000. From the Departments of Psychiatry and Psychology, University of New Mexico School of Medicine. Address reprint requests to Dr. Bustillo, Department of Psychiatry, University of New Mexico School of Medicine, 2400 Tucker NE, Albuquerque, NM 87131; [email protected] (e-mail).
1. Bustillo JR, Lauriello J, Keith SJ: Schizophrenia: improving outcome. Harv Rev Psychiatry 1999; 6:229–240Crossref, Medline, Google Scholar
2. Penn DL, Mueser KT: Research update on the psychosocial treatment of schizophrenia. Am J Psychiatry 1996; 153:607–617Link, Google Scholar
3. Drake RE, Mercer-McFadden C, Mueser KT, McHugo GJ, Bond GR, Kosten TR, Ziedonis DM: A review of integrated mental health and substance abuse treatment for patients with dual disorders. Schizophr Bull 1998; 24:589–608Crossref, Medline, Google Scholar
4. Brown GW, Rutter M: The measurement of family activities and relationships: a methodological study. Human Relations Suppl 1966; 2:10–15Google Scholar
5. Butzlaff RL, Hooley JM: Expressed emotion and psychiatric relapse: a meta-analysis. Arch Gen Psychiatry 1998; 55:547–552Crossref, Medline, Google Scholar
6. Mueser KT, Glynn SM: Family intervention for schizophrenia, in Best Practice: Developing and Promoting Empirically Supported Interventions. Edited by Dobson KS, Craig KD. Newbury Park, Calif, Sage Publications, 1998, pp 157–186Google Scholar
7. Tarrier N, Barrowclough C, Porceddu K, Fitzpatrick E: The Salford Family Intervention Project: relapse rates of schizophrenia at five and eight years. Br J Psychiatry 1994; 165:829–832Crossref, Medline, Google Scholar
8. Linszen D, Dingemans P, Van Der Does JW, Nugter A, Scholte P, Lenior R, Goldstein MJ: Treatment, expressed emotion and relapse in recent onset schizophrenic disorders. Psychol Med 1996; 26:333–342Crossref, Medline, Google Scholar
9. Nugter A, Dingemans P, Van der Does JW, Linszen D, Gersons B: Family treatment, expressed emotion and relapse in recent onset schizophrenia. Psychiatry Res 1997; 72:23–31Crossref, Medline, Google Scholar
10. Hogarty GE, Kornblith SJ, Greenwald D, DiBarry AL, Cooley S, Ulrich RF, Carter M, Flesher S: Three-year trials of personal therapy among patients living with or independent of family, I: description of study and effects on relapse rates. Am J Psychiatry 1997; 154:1504–1513Google Scholar
11. Hogarty GE, Greenwald D, Ulrich RF, Kornblith SJ, DiBarry AL, Cooley S, Carter M, Flesher S: Three-year trials of personal therapy among schizophrenic patients living with or independent of family, II: effects on adjustment of patients. Am J Psychiatry 1997; 154:1514–1524Google Scholar
12. McFarlane WR, Dushay RA, Stastny P, Deakins SM, Link B: A comparison of two levels of family-aided assertive community treatment. Psychiatr Serv 1996; 47:744–750Link, Google Scholar
13. Falloon IR, Boyd JL, McGill CW, Razani J, Moss HB, Gilderman AN: Family management in the prevention of exacerbations of schizophrenia: a controlled study. N Engl J Med 1982; 306:437–440Crossref, Google Scholar
14. Leff J, Kuipers L, Berkowitz R, Berlein-Vries R, Sturgeon D: A controlled trial of social intervention in the families of schizophrenic patients. Br J Psychiatry 1982; 141:121–134Crossref, Medline, Google Scholar
15. Hogarty GE, Anderson CM, Reiss DJ, Kornblith SJ, Greenwald DP, Javna CD, Madonia MJ: Family psychoeducation, social skills training, and maintenance chemotherapy in the aftercare treatment of schizophrenia, I: one-year effects of a controlled study on relapse and expressed emotion. Arch Gen Psychiatry 1986; 43:633–642Crossref, Medline, Google Scholar
16. Tarrier N, Barrowclough C, Vaughn C, Bamrah JS, Porceddu K, Watts S, Freeman H: The community management of schizophrenia: a controlled trial of a behavioural intervention with families to reduce relapse. Br J Psychiatry 1988; 153:532–542Crossref, Medline, Google Scholar
17. Zastowny TR, Lehman AF, Cole RE, Kane C: Family management of schizophrenia: a comparison of behavioral and supportive family treatment. Psychiatr Q 1992; 63:159–186Crossref, Medline, Google Scholar
18. Leff J, Berkowitz R, Shavit N, Strachan A, Glass I, Vaughn C: A trial of family therapy versus a relatives group for schizophrenia. Br J Psychiatry 1989; 154:58–66Crossref, Medline, Google Scholar
19. McFarlane WR, Lukens E, Link B, Dushay R, Deakins SA, Newmark M, Dunne EJ, Horen B, Toran J: Multiple-family groups and psychoeducation in the treatment of schizophrenia. Arch Gen Psychiatry 1995; 52:679–687Crossref, Medline, Google Scholar
20. Schooler NR, Keith SJ, Severe JB, Matthews SM, Bellack AS, Glick ID, Hargreaves WA, Kane JM, Ninan PT, Frances A, Jacobs M, Lieberman JA, Mance R, Simpson GM, Woerner MG: Relapse and rehospitalization during maintenance treatment of schizophrenia: the effects of dose reduction and family treatment. Arch Gen Psychiatry 1997; 54:453–463Crossref, Medline, Google Scholar
21. Falloon IRH, McGill CW, Boyd JL, Pederson J: Family management in the prevention of morbidity of schizophrenia: social outcome of a two-year longitudinal study. Psychol Med 1987; 17:59–66Crossref, Medline, Google Scholar
22. Barrowclough C, Tarrier N: Social functioning in schizophrenic patients, I: the effects of expressed emotion and family intervention. Soc Psychiatry Psychiatr Epidemiol 1990; 25:125–129Crossref, Medline, Google Scholar
23. Zhang M, Yan H: Effectiveness of psychoeducation of relatives of schizophrenic patients: a prospective cohort study in five cities of China. Int J Ment Health 1993; 22:47–59Crossref, Google Scholar
24. Randolf ET, Eth S, Glynn SM, Paz GG, Leong GB, Shaner AL, Strachan A, Van Vort W, Escobar JI, Liberman RP: Behavioural family management in schizophrenia: outcome of a clinic-based intervention. Br J Psychiatry 1994; 164:501–506Crossref, Medline, Google Scholar
25. Lehman AF, Steinwachs DM (Survey Coinvestigators of the PORT Project): Patterns of usual care for schizophrenia: initial results from the Schizophrenia Patient Outcomes Research Team (PORT) client survey. Schizophr Bull 1998; 27:11–19Crossref, Google Scholar
26. Xiong W, Phillips MR, Xiong H, Wang R, Dai Q, Kleinman J, Kleinman A: Family-based intervention for schizophrenic patients in China: a randomised controlled trial. Br J Psychiatry 1994; 165:239–247Crossref, Medline, Google Scholar
27. Zhang M, Wang M, Li J, Phillips MR: Randomised-control trial of family intervention for 78 first-episode male schizophrenic patients: an 18-month study in Suzhou, Jiangsu. Br J Psychiatry Suppl 1994; 165:96–102Crossref, Google Scholar
28. Telles C, Karno M, Mintz J, Paz G, Arias M, Tucker D, Lopez S: Immigrant families coping with schizophrenia: behavioral family intervention v case management with a low-income Spanish-speaking population. Br J Psychiatry 1995; 167:473–479Crossref, Medline, Google Scholar
29. Cardin VA, McGill CW, Falloon IRH: An economic analysis: costs, benefits, and effectiveness, in Family Management of Schizophrenia. Edited by IRH Falloon. Baltimore, Johns Hopkins University Press, 1986, pp 115–123Google Scholar
30. Tarrier N, Lowson K, Barrowclough C: Some aspects of family interventions in schizophrenia, II: financial considerations. Br J Psychiatry 1991; 159:481–484Crossref, Medline, Google Scholar
31. Stein LI, Test MA: Alternative to mental hospital treatment, I: conceptual model, treatment program and clinical evaluation. Arch Gen Psychiatry 1980; 37:392–397Crossref, Medline, Google Scholar
32. Mueser KT, Bond GR, Drake RE, Resnick SG: Models of community care for severe mental illness: a review of research on case management. Schizophr Bull 1998; 24:37–74Crossref, Medline, Google Scholar
33. Holloway F, Carson J: Intensive case management for the severely mentally ill: controlled trial. Br J Psychiatry 1998; 172:19–22Crossref, Medline, Google Scholar
34. Issakidis C, Sanderson K, Teesson M, Johnston S, Buhrich N: Intensive case management in Australia: a randomized controlled trial. Acta Psychiatr Scand 1999; 99:360–367Crossref, Medline, Google Scholar
35. Teague GB, Bond GR, Drake RE: Program fidelity in assertive community treatment: development and use of a measure. Am J Orthopsychiatry 1998; 68:216–232Crossref, Medline, Google Scholar
36. Rosenheck RA, Neale MS: Cost-effectiveness of intensive psychiatric community care for high users of inpatient services. Arch Gen Psychiatry 1998; 55:459–466Crossref, Medline, Google Scholar
37. Latimer E: Economic impacts of assertive community treatment: a review of the literature. Can J Psychiatry 1999; 44:443–454Crossref, Medline, Google Scholar
38. Johnston S, Salkeld G, Sanderson K, Issakidis C, Teesson M, Buhrich N: Intensive case management: a cost-effectiveness analysis. Aust NZ J Psychiatry 1998; 32:551–559Medline, Google Scholar
39. Bellack A, Mueser K: Psychosocial treatment of schizophrenia. Schizophr Bull 1993; 19:317–336Crossref, Medline, Google Scholar
40. Dilk MN, Bond GR: Meta-analytic evaluation of skills training research for individuals with severe mental illness. J Consult Clin Psychol 1996; 6:1337–1346Google Scholar
41. Hogarty G, Anderson C, Reiss D, Kornblith S, Greenwald D, Ulrich R, Carter M: Family psychoeducation, social skills training and maintenance chemotherapy in the aftercare treatment of schizophrenia, II: two-year effects of a controlled study on relapse and adjustment. Arch Gen Psychiatry 1991; 48:340–347Crossref, Medline, Google Scholar
42. Wallace CJ, Liberman RP: Social skills training for patients with schizophrenia: a controlled clinical trial. Psychiatry Res 1985; 15:239–247Crossref, Medline, Google Scholar
43. Brown MA, Munford AM: Life skills training for chronic schizophrenics. J Nerv Ment Dis 1983; 171:466–470Crossref, Medline, Google Scholar
44. Eckman TA, Wirshing WC, Marder SR, Liberman RP, Johnston-Cronk K, Zimmerman K, Mintz J: Technique for training schizophrenic patients in illness self-management: a controlled trial. Am J Psychiatry 1992; 149:1549–1555Google Scholar
45. Marder SR, Wirshing WC, Mintz J, McKenzie J, Johnston K, Eckman TA, Lebell M, Zimmerman K, Liberman R: Two-year outcome of social skills training and group psychotherapy for outpatients with schizophrenia. Am J Psychiatry 1996; 153:1585–1592Google Scholar
46. Liberman RP, Wallace CJ, Blackwell G, Kopelowicz A, Vaccaro JV, Mintz J: Skills training versus psychosocial occupational therapy for persons with persistent schizophrenia. Am J Psychiatry 1998; 155:1087–1091Google Scholar
47. Brenner H, Hodel B, Roder V, Corrigan P: Treatment of cognitive dysfunctions and behavioral deficits in schizophrenia. Schizophr Bull 1992; 18:21–26Crossref, Medline, Google Scholar
48. Hodel B, Brenner HD: Cognitive therapy with schizophrenic patients: conceptual basis, present state, future directions. Acta Psychiatr Scand Suppl 1994; 90:108–115Crossref, Google Scholar
49. Wykes T, Reeder C, Corner J, Williams C, Everitt B: The effects of neurocognitive remediation on executive processing in patients with schizophrenia. Schizophr Bull 1999; 25:291–307Crossref, Medline, Google Scholar
50. Spaulding WD, Reed D, Sullivan M, Richardson C, Weiler M: The effects of cognitive treatment in psychiatric rehabilitation. Schizophr Bull 1999; 25:291–307Crossref, Medline, Google Scholar
51. Wallace CJ, Liberman RP, MacKain SJ, Blackwell, G, Eckman TA: Effectiveness and replicability of modules for teaching social and instrumental skills to the severely mentally ill. Am J Psychiatry 1992; 149:654–658Link, Google Scholar
52. Lehman A: Vocational rehabilitation in schizophrenia. Schizophr Bull 1995; 21:645–656Crossref, Medline, Google Scholar
53. Bond GR, Drake RE, Mueser KT, Becker DR: An update on supported employment for people with severe mental illness. Psychiatr Serv 1997; 48:335–346Link, Google Scholar
54. Bond GR, Dietzen LL, McGrew JH, Miller LD: Accelerating entry into supported employment for persons with severe psychiatric disabilities. Rehab Psychol 1995; 40:91–111Crossref, Google Scholar
55. Drake RE, McHugo GJ, Becker DR, Anthony WA, Clark RE: The New Hampshire study of supported employment for people with severe mental illness. J Consult Clin Psychol 1996; 64:391–399Crossref, Medline, Google Scholar
56. Drake RE, McHugo GJ, Bebout RR, Becker DR, Harris M, Bond GR, Quimby E: A randomized clinical trial of supported employment for inner-city patients with severe mental disorders. Arch Gen Psychiatry 1999; 56:627–633Crossref, Medline, Google Scholar
57. Bell MD, Lysaker PH, Milstein RM: Clinical benefits of paid work activity in schizophrenia. Schizophr Bull 1996; 22:51–67Crossref, Medline, Google Scholar
58. Becker DR, Drake RE: A Working Life: The Individual Placement and Support (IPS) Program. Concord, New Hampshire-Dartmouth Psychiatric Research Center, 1993Google Scholar
59. Kuipers E, Garety P, Fowler D, Dunn G, Bebbington P, Freeman D, Hadley C: London-East Anglia randomised controlled trial of cognitive-behavioural therapy for psychosis, I: effects of treatment phase. Br J Psychiatry 1997; 171:319–327Crossref, Medline, Google Scholar
60. Tarrier N, Yusupoff L, Kinney C, McCarthy E, Gledhill A, Haddock G, Morris J: Randomised controlled trial of intensive cognitive behaviour therapy for patients with chronic schizophrenia. Br Med J 1998; 317:303–307Crossref, Medline, Google Scholar
61. Tarrier N, Wittkowski A, Kinney C, McCarthy E, Morris J, Humphreys L: Durability of the effects of cognitive-behavioural therapy in the treatment of schizophrenia:12-month follow-up. Br J Psychiatry 1999; 174:500–504Google Scholar
62. Sensky T, Turkington D, Kingdon D, Scott JL, Scot J, Siddle R, O’Carroll M, Barnes TRE: A randomized controlled trial of cognitive-behavioral therapy for persistent symptoms in schizophrenia resistant to medication. Arch Gen Psychiatry 2000; 57:165–172Crossref, Medline, Google Scholar
63. Drury V, Birchwood M, Cochrana R, MacMillan F: Cognitive therapy and recovery from acute psychosis: a controlled trial, I: impact on psychotic symptoms. Br J Psychiatry 1996; 169:593–601Crossref, Medline, Google Scholar
64. Buchkremer G, Klingberg S, Holle R, Schulze Monking H, Hornung WP: Psychoeducational psychotherapy for schizophrenic patients and their key relatives or care-givers: results of a 2-year follow-up. Acta Psychiatr Scand 1997; 96:483–491Crossref, Medline, Google Scholar
65. Kuipers E, Fowler D, Garety P, Chisholm D, Freeman D, Dunn G, Bebbington P, Hadley C: London-East Anglia randomised controlled trial of cognitive-behavioural therapy for psychosis, III: follow-up and economic evaluation at 18 months. Br J Psychiatry 1998; 173:61–68Crossref, Medline, Google Scholar
66. Kemp R, Hayward P, Applewhaite G, Everitt B, David A: Compliance therapy in psychotic patients: randomised controlled trial. Br Med J 1996; 312:345–349Crossref, Medline, Google Scholar
67. Tarrier N, Beckett R, Harwood S, Baker A, Yusupoff L, Ugarteburu I: A trial of two cognitive-behavioural methods of treating drug-resistant psychotic symptoms in schizophrenic patients, I: outcome. Br J Psychiatry 1993; 162:524–532Crossref, Medline, Google Scholar
68. May PRA, Tuma AH, Dixon WJ, Yale C, Thiele DA, Kraude WH: Schizophrenia: a follow-up study of the results of five forms of treatment. Arch Gen Psychiatry 1981; 38:776–784Crossref, Medline, Google Scholar
69. Gunderson JG, Frank AF, Katz HM, Vannicelli ML, Frosch JP, Knapp PH: Effects of psychotherapy in schizophrenia, II: comparative outcome of two forms of treatment. Schizophr Bull 1984; 10:564–598Crossref, Medline, Google Scholar
70. Wahlbeck K, Cheine M, Essali A, Adams C: Evidence of clozapine’s effectiveness in schizophrenia: a systematic review and meta-analysis of randomized trials. Am J Psychiatry 1999; 156:990–999Abstract, Google Scholar



