Smaller Brain Size Associated With Unawareness of Illness in Patients With Schizophrenia
Abstract
OBJECTIVE: Although several neuropsychological studies have supported the notion of frontal and parietal lobe involvement in unawareness of illness in schizophrenia, neuroanatomic differences have not been examined.METHOD: Thirty patients with schizophrenia spectrum disorder were rated by means of a structured interview assessing awareness of illness and performance on clinical rating scales. With 13 healthy comparison subjects, they underwent neuropsychological assessment and a scan using three-dimensional, spoiled gradient recall acquisition volumetric magnetic resonance imaging.RESULTS: Patients who were relatively unaware of their illness had smaller brain and intracranial volumes (brain tissue plus CSF) than either aware patients or normal comparison subjects, who did not differ significantly from each other.CONCLUSIONS: These findings suggest that unawareness of illness is an important phenomenological feature with neurological correlates that is seen in at least one subgroup of patients with schizophrenia.
Many patients with schizophrenia demonstrate unawareness of their illness, including difficulty identifying their symptoms and recognizing that they have a mental disorder. This unawareness can have an impact on treatment compliance. It has been noted that unawareness of symptoms in neurological disorders (i.e., anosognosia) is similar in nature to unawareness in schizophrenia (1). Anosognosia has often been associated with lesions in the right parietal lobe and bilateral frontal lobes (e.g., reference 2).
Consistent with this model, there is evidence to suggest a relationship between unawareness of illness in schizophrenia and neuropsychological deficits of the frontal and parietal lobes. Several investigators have found unawareness to be inversely correlated with performance on a frontal lobe task, the Wisconsin Card Sorting Test (3–6), and measures associated with bilateral parietal lobe functioning, including right-left orientation and finger localization (5).
A study by Takai et al. (7) reported that lack of insight into having an illness, as defined by a single item on the Present State Examination, was correlated with increased ventricle-to-brain ratios. To our knowledge, no studies have investigated neuroanatomic correlates of unawareness of signs and symptoms by examining differences in structural neuroanatomy in patients with schizophrenia. We predicted that unawareness of symptoms would be inversely correlated with frontal and parietal lobe volumes.
Method
Subjects were 30 patients (27 inpatients and three outpatients) with diagnoses of schizophrenia spectrum disorder (24 with schizophrenia, five with schizoaffective disorder, and one with psychotic disorder not otherwise specified). After complete description of the study to the subjects, written informed consent was obtained. Comprehensive clinical assessment—including the Structured Clinical Interview for DSM-IV (8), the Brief Psychiatric Rating Scale (BPRS), the Schedule for the Assessment of Positive Symptoms (SAPS) (9), and the Schedule for the Assessment of Negative Symptoms (SANS) (10)—was completed with at least two authors present (L.A.F. and T.W.M.); consensus ratings were used.
The Scale to Assess Unawareness of Mental Disorders (11) is a semistructured interview and scale that assesses present and past awareness of illness and symptoms. There are general questions and items that assess awareness of specific symptoms, and participants are asked questions based on symptoms endorsed on the SANS and SAPS. Items are rated on a 5-point, Likert-type scale, with 1 indicating full awareness and 5 indicating complete unawareness of a symptom.
In addition, these subjects, along with 13 healthy comparison subjects, completed a neuropsychological examination and a structural magnetic resonance imaging (MRI) study by means of a 1.5 Tesla General Electric (Milwaukee, Wis.) magnet (parameters: spoiled grass sequence, TE=13 msec, TR=38 msec, flip angle=45°, number of excitations=1), which yielded a series of 124 contiguous, 1.5-mm coronal slices. Lobar region volumes (in cubed millimeters) were calculated by means of a standardized semiautomated procedure developed at the University of Iowa; detailed methods, including boundary definitions, have been previously reported (12).
Results
On the basis of their average scores for awareness of current episode symptoms on the Scale to Assess Unawareness of Mental Disorders, patients were divided into two groups: those who were aware of their symptoms (average score ≤3, N=12) and those who were unaware of their symptoms (average score >3, N=18). Groups did not differ in terms of age (aware patients: mean=36.4 years, SD=14.9; unaware patients: mean=33.9 years, SD=9.9) (t=0.55, df=28, p=0.59), full-scale IQ (aware patients: mean=96.0, SD=4.6; unaware patients: mean=93.0, SD=14.3) (t=0.55, df=28, p=0.59), gender composition (aware patients: nine men and three women; unaware patients: 13 men and five women) (χ2=0.03, df=1, p=0.87), or handedness (aware patients: 11 right-handed and one left-handed; unaware patients: 16 right-handed and two left-handed) (χ2=0.59, df=1, p=0.80). All left-handed subjects were men. There was a significant group difference for education; the aware patients were more educated than the unaware patients (mean=13.1 years, SD=2.3; mean=11.3 years, SD=2.8, respectively) (t=2.44, df=28, p=0.03). The patient groups were similar on clinical indices, including total SAPS scores (aware patients: mean=9.4, SD=2.9; unaware patients: mean=10.9, SD=2.8) (t=–1.38, df=28, p=0.18), total SANS scores (aware patients: mean=11.7, SD=3.6; unaware patients: mean=9.5, SD=4.1) (t=1.45, df=28, p=0.16), and BPRS scores (aware patients: mean=41.6, SD=12.0; unaware patients: mean=48.5, SD=7.9) (t=–1.90, df=28, p=0.12).
There was no significant correlation between unawareness of symptoms and education (Pearson’s r=–0.20, p=0.29). Pearson correlations indicated no significant correlations between unawareness of symptoms and either SAPS (r=0.02, p=0.90), SANS (r=–0.03, p=0.88), or BPRS (r=0.30, p=0.10) scores.
Thirteen healthy comparison subjects (no history of psychiatric or neurologic illness or injury) did not differ from the patient groups in terms of age (mean=32.8 years, SD=9.2) (t=–0.41, df=41, p=0.68), sex (12 men and one woman) (χ2=1.97, df=1, p=0.16), or handedness (12 right-handed and one left-handed) (<χ2=0.11, df=1, p=0.81), although they had a higher full-scale IQ, with a mean of 108.3 (SD=8.6) (t=3.64, df=41, p=0.0008). The left-handed comparison subject was also male. The comparison group also had slightly more education (mean=14.5 years, SD=1.8) (t=3.49, df=41, p=0.001) than the unaware patient group.
Analyses of variance (PROC GLM, SAS Systems, Inc., Cary, NC) indicated group differences for both brain size (F=9.11, df=2, 40, p=0.0006) and intracranial volume (F=6.50, df=2, 40, p=0.004). Separate planned comparisons with Bonferroni adjustment indicated that the unaware patient group demonstrated smaller brain size (mean=1219.3 mm3, SD=156.5) and intracranial volume (mean=1426.6 mm3, SD=188.5) than either the aware patient group (whole brain mean=1441.1 mm3, SD=255.3; intracranial volume: mean=1672.1 mm3, SD=293.2) or the normal comparison subjects (whole brain mean=1497.3 mm3, SD=175.8; intracranial volume: mean=1674.6 mm3, SD=185.1), although those two groups did not differ significantly from each other. For comparison of individual brain volumes, see Figure 1. Pearson’s correlations were also used to examine awareness as a continuous variable. Inverse correlations were significant for both brain size (r=–0.47, p=0.009) and intracranial volume (r=–0.44, p=0.02); greater unawareness was associated with smaller volumes.
Finally, differences in lobar volumes were examined for the two patient groups. Although significant lobar differences were noted between the aware and unaware patients groups for bilateral frontal, temporal, and parietal lobe tissue volumes, these differences did not remain significant after intracranial volume was entered as a covariate.
Discussion
Patients with schizophrenia who were unaware of their symptoms were found to have smaller brain size and intracranial volume than patients with schizophrenia who were aware of their symptoms. These differences were found despite nonsignificant differences in gender composition or intellectual ability, which have previously been found to be correlated with brain size (13, 14). Furthermore, there were no significant relationships found between unawareness of symptoms and positive symptoms, negative symptoms, illness severity, or education. Unawareness of symptoms appears to represent another important dimension of the heterogeneity seen in schizophrenia. Our findings are consistent with the hypothesis that unawareness of symptoms represents a distinct phenomenological feature rather than a simple reflection of suffix of psychopathology, symptom severity, or level of cognitive functioning.
We did not find lobar correlates of unawareness of symptoms in schizophrenia, as anticipated on the basis of previous neuropsychological findings. Although our results appear consistent with theories of anosognosia that attribute the deficit to diffuse brain dysfunction (15), localized involvement cannot be ruled out. An examination of frontal and parietal lobe subregion differences with a larger study group may help clarify this issue.
It will be important for future studies to investigate other correlates of unawareness in schizophrenia. Although there have been a number of investigations examining neuropsychological differences, to our knowledge, this is the only neuroanatomical study of correlates of unawareness of signs and symptoms of schizophrenia. Studies of neurodevelopmental factors, including obstetric complications, genetic and familial risk factors, and functional neuroimaging, would likely provide a comprehensive perspective of the etiology of unawareness in schizophrenia.
Received June 14, 1999; revision received Oct. 26, 1999; accepted Dec. 14, 1999. From the Brain Imaging Laboratory, Neuropsychiatry Section, Department of Psychiatry, Dartmouth Medical School; New Hampshire Hospital, Concord, NH; and the Mental Health Clinical Research Center, University of Iowa Hospitals and Clinics, Iowa City. Address reprint requests to Dr. Flashman, Department of Psychiatry, Dartmouth-Hitchcock Medical Center, One Medical Center Dr., Lebanon, NH 03756; [email protected] (e-mail). Supported by a Young Investigator Award from the National Alliance on Research on Schizophrenia and Depression, the New Hampshire Hospital, and the Ira DeCamp Foundation. The authors thank Robert Vidaver, Cheryl Brown, Molly Sparling, Annette Donnelly, Chad Moritz, and John Crampton for their help with data collection and analysis.
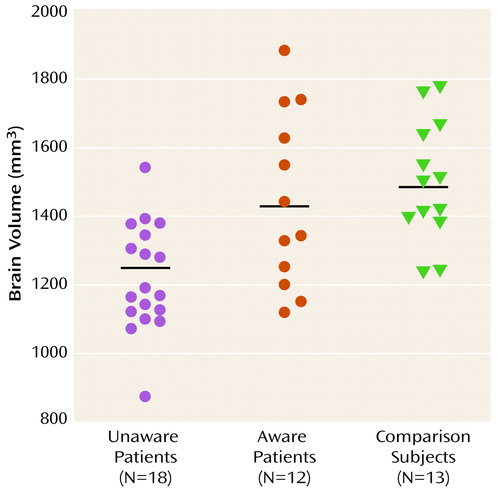
Figure 1. Individual Brain Volumes for Patients With Schizophrenia Who Were Unaware of Their Symptoms, Patients With Schizophrenia Who Were Aware of Their Symptoms, and Healthy Comparison Subjects
1. Amador XF, Strauss DH, Yale SA, Gorman JM: Awareness of illness in schizophrenia. Schizophr Bull 1991; 17:113–132Crossref, Medline, Google Scholar
2. Stuss DT, Benson DF: The Frontal Lobes. New York, Raven Press, 1986Google Scholar
3. Dickerson FB, Boronow JJ, Ringel N, Parente F: Lack of insight among outpatients with schizophrenia. Psychiatr Serv 1997; 48:195–199Link, Google Scholar
4. Lysaker PH, Bell MD, Bryson G, Kaplan E: Neurocognitive function and insight in schizophrenia: support for an association with impairments in executive function but not with impairments in global function. Acta Psychiatr Scand 1998; 97:297–301Crossref, Medline, Google Scholar
5. McEvoy JP, Hartman M, Gottlieb D, Godwin S, Apperson LJ, Wilson W: Common sense, insight, and neuropsychological test performance in schizophrenia patients. Schizophr Bull 1996; 22:635–641Crossref, Medline, Google Scholar
6. Young DA, Davila R, Scher H: Unawareness of illness and neuropsychological performance in chronic schizophrenia. Schizophr Res 1993; 10:117–124Crossref, Medline, Google Scholar
7. Takai A, Uematsu M, Ueki H, Sone K, Kaiya H: Insight and its related factors in chronic schizophrenic patients: a preliminary study. Eur J Psychiatry 1992; 6:159–170Google Scholar
8. Spitzer RL, Williams JBW, Gibbon M: Structured Clinical Interview for DSM-IV (SCID). New York, New York State Psychiatric Institute, Biometrics Research, 1995Google Scholar
9. Andreasen NC: Scale for the Assessment of Positive Symptoms (SAPS). Iowa City, University of Iowa, 1983Google Scholar
10. Andreasen NC: Modified Scale for the Assessment of Negative Symptoms (SANS). Iowa City, University of Iowa, 1984Google Scholar
11. Amador XF, Strauss DH, Yale SA, Flaum MM, Endicott J, Gorman JM: Assessment of insight in psychosis. Am J Psychiatry 1993; 150:873–879Link, Google Scholar
12. Andreasen NC, Rajarethinam R, Cizadlo T, Arndt S, Swayze VW II, Flashman LA, O’Leary DS, Ehrhardt JC, Yuh WTC: Automatic atlas-based volume estimation of human brain regions from MR images. J Comp Assist Tomogr 1996; 20:98–106Crossref, Medline, Google Scholar
13. Andreasen NC, Flaum M, Swayze V II, O’Leary DS, Alliger R, Cohen G, Ehrhardt J, Yuh WTC: Intelligence and brain structure in normal individuals. Am J Psychiatry 1993; 150:130–134Link, Google Scholar
14. Peters M: Sex differences in human brain size and the general meaning of differences in brain size. Can J Psychol 1991; 45:507–522Crossref, Medline, Google Scholar
15. McGlynn SM, Schacter DL: Unawareness of deficits in neuropsychological syndromes. J Clin Exp Neuropsychol 1989; 11:143–205Crossref, Medline, Google Scholar



