Transmission of Response to Trauma? Second-Generation Holocaust Survivors’ Reaction to Cancer
Abstract
OBJECTIVE: Opinions differ about the effects of the Holocaust on the adult offspring of survivors. The authors studied cancer patients who were second-generation Holocaust survivors in an attempt to determine whether they react to their illness with the high distress found to be a characteristic of Holocaust survivors.METHOD: In a study population of women with breast cancer, 106 second-generation Holocaust survivors were compared to 102 women whose parents were not in the Holocaust. Background information was obtained by interviews. In addition, all patients completed three self-reports: the Mental Attitude to Cancer Scale, the Brief Symptom Inventory, and the Impact of Event Scale.RESULTS: The two groups had identical mean scores on the Mental Attitude to Cancer Scale. The offspring of Holocaust survivors had scores on the Brief Symptom Inventory and the Impact of Event Scale that were substantially and significantly higher and in the range of psychopathology. Within the group, married women and women whose mothers were still alive were even more distressed. Other independent variables shed little light on why the second-generation Holocaust survivors suffered from extreme distress.CONCLUSIONS: Second-generation Holocaust survivors are particularly vulnerable to psychological distress and, when faced with a trauma such as breast cancer, react with extreme psychological distress.
Familial nongenetic transmission or intergenerational transmission of psychiatric disorders has been defined as the “process through which, purposively or unintentionally, an earlier generation psychologically influences the parenting attitudes and the behavior of the next generation” (1). The occurrence of this phenomenon in Holocaust survivors and their offspring has received wide attention.
Reports in the literature concerning the psychological status of the second generation of Holocaust survivors are conflicting. Most of the clinical studies point to higher rates of psychopathology. Bergmann and Jucovy (2) concluded that in a world in which the horror of the Holocaust is the dominant psychic reality, it is not possible for a child of Holocaust survivors to grow up without becoming scarred and helpless. More controlled studies, however, have not supported that statement, leading Solkoff (3) to suggest that “the intergenerational effects of persecution are rooted in nothing more than unreliable data gathered from biased samples in poorly designed experiments.”
In a 3-year study of combat stress reaction casualties, Solomon et al. (4) found that soldiers who were the offspring of Holocaust survivors had a higher incidence of posttraumatic stress disorder (PTSD), more severe psychological syndromes, and a poorer recovery rate 2 and 3 years after the combat experience than soldiers who were not children of survivors.
For a number of years we have been studying the vulnerability to psychological distress of different patient populations diagnosed with cancer. One of the hypotheses confirmed from several of our studies was that people who had previously experienced situations that were severely life-threatening would cope less well and display more distress when confronted with a new life threat such as cancer. We interviewed cancer patients who had survived the Holocaust and compared them to a matched group of “nontraumatized” cancer patients and a group of healthy Holocaust survivors. The psychological distress of the cancer patients who had survived the Holocaust was substantially and very significantly higher than that of the nontraumatized cancer patients. The healthy Holocaust survivors showed a normal overall degree of psychological distress, but their profile, measured by the Brief Symptom Inventory, suggested that they would not be able to mobilize additional resources and were likely to react with extreme psychological distress when faced with a severe new threat (5, 6). Yehuda et al. (7) reported similar findings of extreme psychological distress after cancer diagnosis in their study of PTSD in Holocaust survivors, in whom the occurrence and severity of PTSD symptoms were related to current and lifetime stressors in addition to the focal trauma.
It seems reasonable to suggest that the offspring of Holocaust survivors might be as vulnerable as their parents and, similar to their parents, may function adequately in their daily activities but be unable to cope with the emotion of extreme stress or severe life-threatening situations. Accordingly, the hypothesis of the present study is that second-generation Holocaust survivors are vulnerable to psychological distress and, when confronted with a life-threatening illness such as cancer, will manifest more distress than patients who are not second-generation Holocaust survivors.
Method
Subjects
Patients were recruited from three medical centers: Hadassah in Jerusalem and Sheba and Beilinson in the Tel Aviv area. The records of all patients at these hospitals include sociodemographic data such as parents’ countries of origin and dates of immigration to Israel.
The following patients were eligible for inclusion in the study: Jewish women with breast cancer (8 months–8 years after the initial diagnosis) who had resided in Israel for at least 10 years (to exclude the confounding variable of stress due to recent immigration) and were able to complete self-reports in Hebrew. After receiving approval for the study by the review boards of each hospital, we were able to select the patients by scanning the data to identify second-generation Holocaust survivors.
Holocaust survivors were defined as Jews who had been in a concentration camp, forced labor camp, or extermination camp in Europe during the World War II. Second-generation Holocaust survivors were individuals whose parents, either one or both, had survived the Holocaust. A group of breast cancer patients whose parents were not in the Holocaust served as a comparison group.
After their participation was approved by their physician, an experienced research coordinator contacted each patient by telephone to explain the purpose of the study. If the patient agreed to participate, a senior clinical psychologist went to her home, obtained the patient’s signed informed consent, conducted a semistructured interview, and administered the self-report questionnaires.
Measures
All patients completed three self-report questionnaires. The Brief Symptom Inventory (8) is a 53-item assessment tool used extensively to assess global psychological distress (determined by the individual’s score on the grand severity index). The measure has nine specific subscales (somatization, obsessive-compulsive, interpersonal sensitivity, depression, anxiety, hostility, phobic anxiety, paranoid ideation, and psychoticism). The raw scores are converted to T scores. The accepted cutoff point for psychopathology is a grand severity index score of 63 or scores of 63 on three of the subscales. Its internal reliability in the present study was excellent (Cronbach’s alpha=0.94).
The Impact of Event Scale (9) is a 15-item measure used extensively to assess the intrusiveness (seven items) and the avoidance (eight items) of an event, which in the present study was cancer. Its internal reliability was good in the present study (Cronbach’s alphas ranged from 0.82 to 0.85), except for an alpha of below 0.70 for the measure of avoidance in the comparison group. The cutoff point for psychopathology is not well defined, but a score of 20 and above on the Impact of Event Scale usually suggests psychological problems.
The Mental Adjustment to Cancer Scale (10) is a 41-item measure that assesses how patients cope with cancer by measuring fighting spirit, hopelessness/helplessness, anxious preoccupation, and fatalistic acceptance. Significant intercorrelations are usually found between the four subscales. The scale has no norms. In the present study, the internal reliability of two of the subscales (anxious preoccupation and fatalistic acceptance) fell below 0.70, but the two groups were very similar with respect to these items. For the other two scales (fighting spirit and hopelessness/helplessness), the internal reliabilities exceeded 0.70 for both groups.
Statistical Analysis
For continuous variables, the two groups were compared by using a t test with Bonferroni correction. Categorical variables were compared by applying a chi-square test. A stepwise multiple regression analysis was conducted for each of the three dependent outcome measures (the grand severity index score and scores on the intrusion and avoidance subscales of the Impact of Event Scale). The significance level for the F test was set at 0.10 for the inclusion of variables and 0.11 for their removal. Age, marital status, education, religiosity, mother/father being alive, time from diagnosis, Karnofsky performance scale score, and scores on the four Mental Attitude to Cancer Scale subscales were included as independent variables. Interaction terms (group by variable) were included for each of the four Mental Attitude to Cancer Scale subscales, marital status, and for having a mother who was still living.
Results
A total of 113 patients who were second-generation Holocaust survivors were approached, and 106 of them (93.8%) agreed to participate in the study. Of 114 patients in the comparison group, 102 (89.5%) agreed to participate.
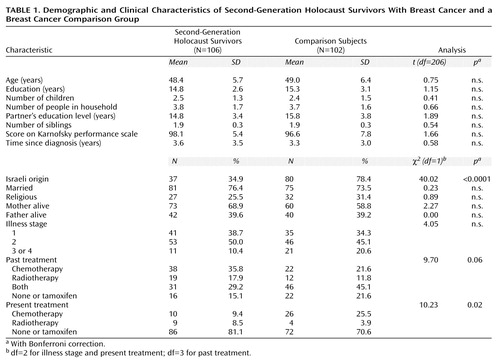
The two groups were similar in sociodemographic background (Table 1). For the majority of the second-generation group, both parents had been Holocaust survivors (nine subjects had only mothers who were survivors, and seven subjects had only fathers who were survivors). Most of the second-generation Holocaust survivors were not born in Israel, whereas the majority of the comparison group were first-generation Israelis (only 12 had parents who were born in Israel). The parents of both patient groups were immigrants from Europe, the major distinction of course being that only those of the second-generation group had been victims of the Holocaust. No other differences were found on any of the sociodemographic background variables. However, some differences between the two groups were found in their medical background, as the comparison group had lower scores on the Karnofsky performance scale and more patients in stage 3 and 4 of their illness, although there were no differences from time of diagnosis. Significantly more patients in the comparison group (26%) were in chemotherapy at the time of the study.
Table 1 presents the results from the three self-report questionnaires of the second-generation Holocaust survivors with breast cancer and the breast cancer comparison group. No differences were found between the two groups on scores on the Mental Adjustment to Cancer Scale, which assesses coping with cancer and suggests that the second-generation Holocaust survivors were coping with the breast cancer diagnosis as well as the comparison group.
However, extreme differences were found on the two self-report questionnaires that assess psychological condition. The second-generation Holocaust survivors had extremely high scores on both the intrusion and avoidance subscales of the Impact of Event Scale. The differences between the two groups were even more extreme on the Brief Symptom Inventory. The comparison group had a grand severity index score of 54, which suggests mild psychological distress, and only one subscale score that exceeded 55 (somatization). One would expect such scores from breast cancer patients who are in fairly good medical condition. The second-generation Holocaust survivors, however, scored substantially higher, and the difference was statistically significant for all the dimensions. The second-generation Holocaust survivors had a grand severity index score of 66 and scored above 63 on five of the nine dimensions (somatization, depression, anxiety, hostility, and psychoticism). These scores are considered to be in the range of psychopathology.
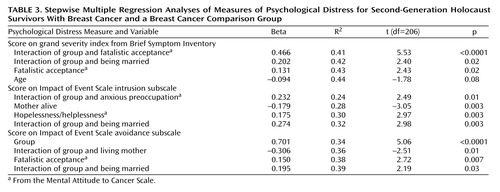
The differences between the two groups were highlighted when three stepwise multiple regressions were carried out, with scores on the grand severity index and the intrusion and avoidance subscales of the Impact of Event Scale as dependent variables (Table 3). Age, marital status, education, religiosity, mother/father alive, time from diagnosis, score on the Karnofsky performance scale, the four Mental Attitude to Cancer Scale dimensions, and interaction terms (group by the four Mental Attitude to Cancer Scale dimensions, group by mother alive, and group by marital status) were included as independent variables. For each of the multiple regression analyses, Karnofsky score, father being alive, education, religiosity, and fighting spirit did not enter any of the equations.
Grand Severity Index Score
The remaining independent variables explained 44% of the variability in score on the grand severity index (Table 3). Fatalistic acceptance was significantly related to grand severity index score: the higher the fatalistic acceptance level, the higher the grand severity index score. However, since the group-by-fatalistic acceptance interaction was shown to be significant, the relationship between grand severity index score and level of fatalistic acceptance was studied for each group. For the comparison group, the higher the fatalistic acceptance level, the higher the grand severity index score, but no relationship was found between the two variables in the second-generation Holocaust survivors. In addition, the group-by-married interaction was found to be significant. In the second-generation Holocaust survivors, higher grand severity index scores were observed in married women than in unmarried women, whereas in the comparison group, there was no relationship between being married and score on the grand severity index.
Intrusion
The studied variables explained 32% of the variance in scores on the intrusion subscale of the Impact of Event Scale (Table 3). Having a mother who was still alive was shown to be a significant variable related to intrusion: lower levels of intrusion were observed when the mother was not alive. Married women in the breast cancer group of second-generation Holocaust survivors showed higher intrusion levels, whereas married women in the breast cancer comparison group did not. This interaction between group and being married was significant. Another significant interaction was found for group by anxious preoccupation: in the comparison group, the higher the anxious preoccupation, the higher the intrusion level; whereas in the second-generation group, there was no correlation between the two variables. Hopelessness/helplessness was significantly related to intrusion as well: the higher the level of hopelessness/helplessness, the higher the intrusion subscale score.
Avoidance
The studied variables explained 39% of the variance in scores on the avoidance subscale of the Impact of Event Scale (Table 3). A significant group difference was found as the avoidance levels were higher for the second-generation Holocaust survivors. The interaction of group and being married was significant: higher levels of avoidance were observed in the second-generation Holocaust survivors who were married, whereas no such relationship was found for the comparison group. The group-by-mother alive interaction was also significant. For the second-generation group, lower levels of avoidance were observed when the mother was not alive; whereas in the comparison group, no relationship between the two variables was found. Finally, fatalistic acceptance was directly related to avoidance: the higher the level of fatalistic acceptance, the higher the avoidance subscale score.
Discussion
More than 200 women diagnosed with breast cancer participated in this study. About half of them were the offspring of Holocaust survivors and the rest comprised the comparison group. There was a low refusal rate, and participation in both groups was about 90%, which suggests that the two groups may be considered representative of women diagnosed with breast cancer. Thus, the premise of Solkoff (3) that the “major flaw is sampling” seems to have been avoided. Furthermore, the mean scores for the comparison group on the Brief Symptom Inventory and on the Impact of Event Scale were very similar to those obtained in earlier studies of women with breast cancer (11).
The two groups had similar background characteristics: the mean age was 48–49 years, they had 15 years of education on average, about 75% were married, and the mean number of children was 2.4–2.5. Also similar was the socioeconomic status of the two groups, as reflected by professions and the number of people living at home. They also shared similar backgrounds in terms of siblings and whether their parents were alive. However, they differed with regard to place of birth: most of the second-generation Holocaust survivors were born outside Israel, whereas the majority of the comparison group were born in Israel. The parents of patients in both groups were mostly immigrants. Parents of the second-generation Holocaust survivors were, by definition, immigrants from Europe, as were nearly 90% of the parents of the comparison group patients. Solkoff (12) maintains that the “immigrant status is as important as the Holocaust experience in determining differences in psychological adjustment among offspring.” That potential source of error was avoided in this study, and the differences observed between the groups cannot therefore be attributed to differences in the immigrant status of their parents.
The two groups were also similar with respect to their medical condition, although the second-generation Holocaust survivors were in somewhat better medical condition.
The ability of the patients to cope with cancer, as assessed by the Mental Attitude to Cancer Scale, was practically identical for the two groups. The scores obtained on the fighting spirit subscale were somewhat lower than those reported by Greer and Watson in one of their studies (13) and somewhat higher than those reported in another (14). On the other subscales, the mean scores of our patients were very close to the scores of the patients in those two studies. Compared to an earlier study of 40 older female cancer patients in Israel (15), patients in the present study had subscale scores that were somewhat higher for fighting spirit and somewhat lower for helplessness/hopelessness and fatalistic acceptance. As judged by their responses on the Mental Attitude to Cancer Scale, therefore, the two groups in our study appeared to react and cope with their disease much like other patients with breast cancer.
The groups differed drastically, however, on the two measures of psychological distress. Patients in the comparison group appeared to be only mildly distressed, as measured by both the Brief Symptom Inventory and the Impact of Event Scale. The second-generation Holocaust survivors were extremely distressed, with scores in the range of psychopathology on both measures. Thus, the basic hypothesis of our study, that the second-generation Holocaust survivors react emotionally with extreme distress to a threatening event such as cancer, was confirmed.
Similar findings were obtained by Yehuda et al. (16), who studied a group of physically healthy second-generation Holocaust survivors and a comparison group. Among the second-generation Holocaust survivors, there was a significantly higher prevalence of current and lifetime PTSD and other psychiatric diagnoses than in the comparison group, although they had not experienced a specific traumatic event. The survivor group also appeared to have experienced a greater degree of cumulative lifetime stress. The authors concluded that the offspring of Holocaust survivors either actually experience more ordinary life stresses in their daily lives or are more likely to characterize these experiences as major emotional problems or crises. This latter possibility might explain why the second-generation Holocaust survivors in the present study were more distressed than the comparison group, i.e., they may have experienced their cancer as a major crisis. This suggestion, however, is not supported by the results obtained on the Mental Attitude to Cancer Scale.
Thus, among the second-generation Holocaust survivors we found a discrepancy between the “normal” reaction to having cancer (as reflected by the Mental Attitude to Cancer Scale findings) and the extreme psychological distress reflected on both the Brief Symptom Inventory and the Impact of Event Scale. In previous studies, we found a similar discrepancy in cancer patients who were first-generation Holocaust survivors. The functional adjustment of those patients to cancer was as good as that of the comparison group, but their psychological distress was significantly greater (5). It could be suggested that people for whom emotions act as an internal stimulus who recall unresolved threats may perceive any additional emotional threat as intrusive. They may also experience their emotions as overwhelming and disorganizing forces that should be avoided and controlled. In this situation, their emotions do not facilitate adaptation and mastery but rather reflect greater distress and a strengthening of their avoidance mechanism (17).
Mandler (18) suggested that high emotion can either be adaptive—in which case an appropriate behavior must be learned—or it will lead to greater distress in situations in which people become convinced that they cannot influence the outcome. Emotionally, this conviction is experienced with high anxiety, accompanied by a state of helplessness that is unrelieved by any kind of coping behavior.
The two groups in the present study differed not only in their levels of psychological distress but also in the factors found to contribute to distress. Among the second-generation Holocaust survivors, those whose mothers were alive reported significantly higher levels of intrusion (from the Impact of Event Scale) than did those whose mothers were dead. Two studies have suggested that Holocaust survivor parents do indeed contribute to the distress of their offspring. Yehuda et al. (16) studied a small group of Holocaust survivors and their adult offspring and found that symptoms of distress in the offspring may be related to the presence and severity of symptoms in the parents. After traumatic events, they are more likely to develop PTSD if their parents had PTSD. Thus, a high incidence of PTSD in mothers who survived the Holocaust might explain the high intrusion and avoidance symptoms found in the second-generation offspring. In the second study, Schwartz et al. (19) studied a large community sample. They did not find higher rates of current psychopathology in second-generation subjects, but they did find significantly higher rates of past disorders in that group. In both studies, the authors concluded that living with a depressed, intrusive parent is a stressful situation that causes affective and anxiety disorders in the children. It could be suggested that after being diagnosed with breast cancer, a woman who normally would turn to her mother would prefer avoidance if her mother is a Holocaust survivor so as not to cause her more anxiety and psychological distress.
There was no sound explanation for the unexpected finding among second-generation Holocaust survivors that, in contrast to the findings of most studies on marriage and social support, the married women were more distressed than were the unmarried women. Nor could we find information on marriage as a source of distress rather than of support in healthy second-generation Holocaust survivors. We can only speculate that the emotional pressures of conforming to married life impose more of a stressful burden than a mutual sharing of support. Perhaps the women in our study perceived their own marriage as yet another emotional encumbrance that required them to exhibit a facade of additional strength and control.
These findings and their interpretation are in line with the basic finding of high psychological distress among patients who are second-generation Holocaust survivors and raise the question: what is transmitted from the first-generation survivors to their offspring? The findings of Yehuda et al. (16) reinforce the fact that vulnerability to PTSD is transmitted to the offspring. The fact that the traumatized parents were exposed over a long period to uncontrollable and extreme situations (17, 20) could result in the transmission of an intrusive-avoidant coping style to their children to such a degree that it became an integral part of their personality. Our data showed significantly high levels of intrusion and avoidance in the second-generation Holocaust survivors.
Ford and Neale (21) point out that if the belief in internal lack of control produced by helplessness persists for a long time, it will lead to an underestimation of control in a highly uncontrollable situation, such as cancer.
These are intriguing ideas that should be further investigated by studying sick and healthy second-generation Holocaust survivors and their parents. Nevertheless, it does seem clear from the present study that second-generation Holocaust survivors are particularly vulnerable to psychological distress and should be regarded as a population at risk. Although this study was limited to second-generation Holocaust survivors, we would like to suggest that the findings should not be restricted to this specific population and that the offspring of any severely traumatized parents (e.g., victims of war and forced immigration) should be regarded as especially vulnerable and at high psychological risk.
 |
 |
Received March 1, 1999; revision received Aug. 13, 1999; accepted Nov. 18, 1999. From the Department of Clinical Oncology and Radiotherapy, Sharett Institute of Oncology, Hadassah University Hospital; the Institute of Oncology, Beilinson Hospital, Petach Tikvah, Israel; and the Department of Oncology, Tel Hashomer Medical Center, Tel Aviv, Israel. Address reprint requests to Dr. Baider, Department of Clinical Oncology and Radiotherapy, Sharett Institute of Oncology, Hadassah University Hospital, Jerusalem 91120, Israel. Supported through a research grant (980035-C) from the Israel Cancer Association.
1. Van Ijzendoorn MH: Intergenerational transmission of parenting: a review of studies in non-clinical populations. Dev Rev 1992; 12:76–99Crossref, Google Scholar
2. Bergmann MS, Jucovy ME (eds): Generations of the Holocaust. New York, Basic Books, 1982Google Scholar
3. Solkoff N: Children of survivors of the Nazi Holocaust: a critical review of the literature. Am J Orthopsychiatry 1981; 51:29–42Crossref, Medline, Google Scholar
4. Solomon Z, Kotler M, Mikulincer M: Combat-related posttraumatic stress disorder among second-generation Holocaust survivors: preliminary findings. Am J Psychiatry 1988; 145:865–868Link, Google Scholar
5. Baider L, Peretz T, Kaplan DeNour A: Effect of the Holocaust on coping with cancer. Soc Sci Med 1992; 34:11–16Crossref, Medline, Google Scholar
6. Peretz T, Baider L, Ever-Hadani P, Kaplan DeNour A: Psychological distress in female cancer patients with Holocaust experience. Gen Hosp Psychiatry 1994; 16:413–418Crossref, Medline, Google Scholar
7. Yehuda R, Kahana B, Schmeidler J, Southwick SM, Wilson S, Giller EL: Impact of cumulative lifetime trauma and recent stress on current posttraumatic stress disorder symptoms in Holocaust survivors. Am J Psychiatry 1995; 152:1815–1818Google Scholar
8. Derogatis LR, Spencer P: The Brief Symptom Inventory (BSI): Administration, Scoring and Procedures Manual. Baltimore, Clinical Psychometric Research, 1982Google Scholar
9. Horowitz MJ, Wilner N, Alvarez W: Impact of Event Scale: a measure of subjective stress. Psychosom Med 1979; 41:209–218Crossref, Medline, Google Scholar
10. Watson M, Greer S, Young J, Inayat Q, Burgess C, Robertson B: Development of a questionnaire measure of adjustment to cancer: the MAC scale. Psychol Med 1988; 18:203–209Crossref, Medline, Google Scholar
11. Baider L, Kaplan DeNour A: Psychological distress and intrusive thoughts in cancer patients. J Nerv Ment Dis 1997; 185:346–348Crossref, Medline, Google Scholar
12. Solkoff N: Children of survivors of the Nazi Holocaust: a critical review of the literature. Am J Orthopsychiatry 1992; 62:342–358Crossref, Medline, Google Scholar
13. Greer S, Watson M: Mental adjustment to cancer: its measurement and prognostic importance. Cancer Surv 1987; 6:439–453Medline, Google Scholar
14. Greer S, Moorey S, Watson M: Patients’ adjustment to cancer: the Mental Adjustment to Cancer (MAC) scale vs clinical ratings. J Psychosom Res 1989; 33:373–377Crossref, Medline, Google Scholar
15. Baider L, Walach N, Perry S, Kaplan DeNour A: Cancer in married couples: higher or lesser distress? J Psychosom Res 1998; 45:1–11Google Scholar
16. Yehuda R, Schmeidler J, Giller EL Jr, Siever LJ, Binder-Brynes K: Relationship between posttraumatic stress disorder characteristics of Holocaust survivors and their adult offspring. Am J Psychiatry 1998; 155:841–843Link, Google Scholar
17. Mikulincer M: Human Learned Helplessness: A Coping Perspective. New York, Plenum, 1994Google Scholar
18. Mandler G: The generation of emotion: a psychological theory, in Emotions: Theory, Research and Experience, vol 1. Edited by Plutchik R, Kellerman H. New York, Academic Press, 1980, pp 219–236Google Scholar
19. Schwartz S, Dohrenwend BP, Levav I: Nongenetic familial transmission of psychiatric disorders? evidence from children of Holocaust survivors. J Health Soc Behav 1994; 35:385–402Crossref, Medline, Google Scholar
20. Garber J, Seligman M (eds): Human Helplessness: Theory and Applications. New York, Academic Press, 1980Google Scholar
21. Ford CE, Neale JM: Learned helplessness and judgements of control. J Pers Soc Psychol 1985; 49:1330–1336Google Scholar



