Multiple Recurrences of Major Depressive Disorder
Abstract
OBJECTIVE: The authors of this study examined multiple recurrences of unipolar major depressive disorder. METHOD: A total of 318 subjects with unipolar major depressive disorder were prospectively followed for 10 years within a multicenter naturalistic study. Survival analytic techniques were used to examine the probability of recurrence after recovery from the index episode. RESULTS: The mean number of episodes of major depression per year of follow-up was 0.21, and nearly two-thirds of the subjects suffered at least one recurrence. The number of lifetime episodes of major depression was significantly associated with the probability of recurrence, such that the risk of recurrence increased by 16% with each successive recurrence. The risk of recurrence progressively decreased as the duration of recovery increased. Within subjects, there was very little consistency in the time to recurrence. CONCLUSIONS: Major depressive disorder is a highly recurrent illness. The risk of the recurrence of major depressive disorder progressively increases with each successive episode and decreases as the duration of recovery increases.
Major depressive disorder is usually an episodic disease, with recurrent episodes occurring in at least 50% of the patients seeking treatment for major depression at tertiary care centers (1). Although patients usually suffer multiple episodes of major depression, most studies have examined only a single recurrence.
The National Institute of Mental Health (NIMH) Collaborative Program on the Psychobiology of Depression (2) is a prospective, naturalistic, longitudinal investigation that has helped describe the episodic course of illness in major depressive disorder. Early research from the NIMH collaborative depression study found that after recovery from an index episode of unipolar major depression, the cumulative probability of recurrence was nearly 30% after 6 months of follow-up and almost 40% after 12 months of follow-up (3). The time to recurrence was significantly shorter for those with a history of three or more episodes of major depression before intake than for subjects with fewer than three previous episodes.
Since that 1983 report, a large number of subjects from the NIMH collaborative depression study have suffered multiple recurrences. The present study focuses on the time to recurrence of major depressive disorder across multiple episodes that have been prospectively observed in their entirety. Based on studies of a single recurrence (3–5), it was predicted that as the duration of recovery increases, the risk of recurrence decreases. A second prediction was that each recurrence increases the probability of yet another recurrence.
METHOD
Subjects
From 1978 to 1981, individuals receiving inpatient or outpatient treatment for a mood disorder were recruited into the collaborative depression study at academic medical centers in Boston, Chicago, Iowa City (Iowa), New York, and St. Louis. Inclusion criteria included an age of 17 years or more, an IQ greater than 70, the ability to speak English, white race (genetic hypotheses were tested), and no signs of a mood or psychotic disorder secondary to a general medical condition. After receiving a complete description of the study, the subjects provided written informed consent.
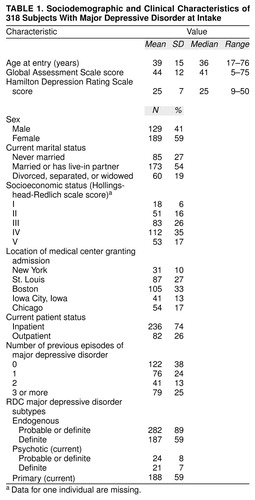
A total of 955 patients entered the collaborative depression study. Within this group, 431 were experiencing an episode of major depression but had no underlying minor depression of at least 2 years’ duration, no chronic intermittent depressive disorder, and no history of mania, hypomania, or schizoaffective disorder. Of these 431 subjects, 65 had a diagnosis change to either bipolar or schizoaffective disorder during the follow-up period and were excluded from the analyses in this article. Of the remaining 366 subjects, 318 eventually recovered from the intake episode of major depression during the 10-year follow-up and were at risk for a recurrence. The other 48 subjects did not recover during the follow-up. (Of these 48 subjects, 30 dropped out of the study before recovering from the intake episode, and 18 subjects remained in the study for the entire 10 years of follow-up and did not recover from their intake episode.) The study group for the analyses in this article thus consisted of 318 subjects. Table 1 lists their sociodemographic and clinical characteristics at intake.
Assessments
Current and past psychiatric histories were assessed with the Schedule for Affective Disorders and Schizophrenia (6). Diagnoses were made according to the Research Diagnostic Criteria (RDC) (7).
Follow-up assessments were completed every 6 months for the first 5 years of the study and annually thereafter by using the Longitudinal Interval Follow-Up Evaluation (8). This is a semistructured instrument that measures numerous clinical variables, including the severity of psychopathology on a weekly basis, as well as the type and dose of all prescribed medication. The severity of psychopathology is quantified on a 6-point scale called the psychiatric status rating, which is assigned to any present psychiatric disorder. At each interview, the rater assigned a psychiatric status rating for each week of the study, starting from the last interview. To accomplish this, the rater first identified chronological anchor points, such as holidays, to help the subject remember when significant clinical improvement or deterioration occurred. Whenever possible, corroborative data were obtained from medical records and informants.
The analyses reported in this article are based on the psychiatric status ratings for the 318 subjects with unipolar major depression at intake who subsequently recovered. The analyses encompass data for up to 520 weeks of follow-up. Recovery was defined as at least 8 consecutive weeks with either no symptoms of major depressive disorder or only one or two symptoms at a mild level of severity. Recurrence was defined as the reappearance of RDC major depressive disorder meeting the full criteria for at least 2 consecutive weeks, beginning with the first of these 2 weeks. Recurrence occurred only after the individual had first recovered from his or her preceding mood episode. Episodes of RDC minor depression and chronic intermittent depression were not included in these analyses.
Treatment
This was an observational study in that treatment was not randomly assigned by design and not controlled by anyone connected with the study. However, somatic treatment was quantified with the Longitudinal Interval Follow-Up Evaluation for each week of the study. To rate the intensity of such treatment, equivalent dose ranges were established for different classes of antidepressant somatic therapy (including lithium carbonate and electroconvulsive therapy). These dose ranges were then summarized on a 5-point scale to generate a composite antidepressant score (9) for each week of the study. Each point on the scale specified a range of daily doses of imipramine or its equivalent. A composite antidepressant score of zero indicated that no antidepressant somatic treatment was provided, a composite antidepressant score of 1 indicated a daily dose of 1 mg to 99 mg of imipramine or its equivalent, a composite antidepressant score of 2 indicated a daily dose of 100 mg to 199 mg of imipramine or its equivalent, a composite antidepressant score of 3 indicated a daily dose of 200 mg to 299 mg of imipramine or its equivalent, and a composite antidepressant score of 4 indicated a daily dose of 300 mg or more of imipramine or its equivalent.
Statistical Analyses
Time to recurrence (i.e., duration of recovery) was examined by using survival analytic techniques (10). These analytic techniques account for varying lengths of follow-up and estimate the changing probability of recurrence at different times over the course of follow-up (11).
The survival time (the time to recurrence) began after the completion of an 8-week recovery period. The event that ended each recovery was recurrence or (for censored cases) end of the follow-up period (10 years), withdrawal from the study, or death. The cumulative probability of recurrence was estimated with the Kaplan-Meier product limit (12). Separate analyses were conducted for the first five recurrences that began in the period encompassing baseline through year 10 (only 12 [4%] of 318 subjects experienced more than five recurrences during the follow-up period). The 6-month, interval-specific probabilities of recurrence, which are similar to hazard functions, were also calculated.
To evaluate the influence of successive episodes on the probability of recurrence over time, a mixed-effects, grouped-time survival analysis (13) was used to examine all prospectively observed recovery periods in one model. The fixed effect was a time-varying covariate: number of lifetime episodes of major depression. These constituted both the episodes of major depressive disorder before the index episode (ranging from 0 to 3 or more) and all prospectively observed episodes. The random intercept term accounted for the clustering of episodes within each subject. In this grouped-time model, the recovery durations were grouped as follows: monthly for 6 months, quarterly for the remainder of year 1 through year 4, annually for years 5 through 7, and biannually for years 8 through 10. The mixed model was also used to calculate an intraclass correlation coefficient (ICC), which estimates the within-subject consistency of the duration of recovery (14). The mixed model was analyzed by using MIXGSUR software (15). All analyses were conducted with a two-tailed alpha level of 0.05.
RESULTS
The study group comprised 318 subjects who had recovered from their intake episode of unipolar major depression during the first 10 years of follow-up are included. Data for 34 subjects (11%) who died during follow-up are included. Of the 318 subjects, 263 (83%) were followed for at least 5 years, and 208 (65%) were followed for the entire 10-year period. The mean length of follow-up was 419 weeks (SD=159), and the median length of follow-up was 520 weeks. A total of 481 recurrences were observed during the 10-year follow-up. The mean number of episodes of major depressive disorder per year of follow-up was 0.21 (SD=0.24).
Survival Analyses of Time to Recurrence
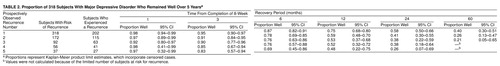
The survival analyses for the first five prospectively observed recurrent episodes of major depressive disorder are shown in table 2. The analyses are presented as the proportion of subjects who had not yet had a recurrence (i.e., remained well) at various points in the follow-up period. The time periods start after the completion of an 8-week recovery period. (Subjects were at risk for recurrence only after they had recovered—i.e., completed the 8-week recovery period.) There were 318 subjects who recovered from their intake episodes. Of these, 202 suffered a recurrence. The remainder were treated as censored cases at the end of their follow-up. The cumulative probability of recurrence at 1 year was 25%; at 2 years, 42%; and at 5 years, 60%. (The proportions in table 2 represent Kaplan-Meier product limit estimates, which incorporate censored cases.)
Of the 202 subjects who suffered a recurrence, 172 recovered and were at risk for a second recurrence. A total of 115 subjects eventually had a second recurrence. The cumulative probability of recurrence at 1 year was 41%; at 2 years, 59%; and at 5 years, 74%.
With each succeeding recurrence, the cumulative probability of recurrence generally increased at each time point (moving down each column in table 2). However, the overlapping confidence intervals at each time point suggest that the differences were not statistically significant.
Median Time to Recurrence
For the entire study group, the median time to recurrence for the first prospectively observed recurrence was 150 weeks, and the 95% confidence interval (CI) was 116–204 weeks. For the second recurrence, the time was 83 weeks (95% CI=60–108); for the third recurrence, 77 weeks (95% CI=44–104); for the fourth recurrence, 68 weeks (95% CI=32–112); and for the fifth recurrence, 57 weeks (95% CI=28–88). The 95% CIs indicate that the median time to recurrence for the first prospective recurrence was significantly longer than the time to recurrence for subsequent recurrences. For subsequent episodes, the median times to recurrence did not differ significantly (because of overlapping CIs).
Interval-Specific Probability of Recurrence
Analyses were also conducted to calculate the semiannual interval-specific probability of recurrence—that is, the probability that a patient who was still well at the start of a 6-month interval would experience a recurrence during those 6 months. Across the five recurrences, the mean probability of recurrence during the first 6 months after recovery was 20% (SD=6) (weighted by number of subjects). This indicates that, on average, of the subjects at risk for recurrence, 20% had a recurrence in the first 6 months after the onset of recovery from the preceding depressive episode.
In subsequent 6-month intervals, the rate of recurrence decreased. Across all five recurrences, the weighted mean for the probability of recurrence in the second 6 months (months 7–12) after the onset of recovery from the preceding mood episode was 19% (SD=7); in the third 6 months (months 13–18), the weighted mean was 15% (SD=6); in the fourth 6 months (months 19–24), the weighted mean was 13% (SD=3); in the fifth 6 months (months 25–30), the weighted mean was 11% (SD=3); and in the sixth 6 months (months 31–36) after the onset of recovery from the preceding mood episode, the weighted mean for the probability of recurrence was 9% (SD=6). The mean average interval-specific probabilities of recurrence were not compared statistically because the groups of subjects overlapped.
Probability of Recurrence
Mixed-effects, grouped-time survival analysis was used to examine recurrence during all prospectively observed recovery periods. The number of lifetime episodes of major depressive disorder was significantly associated with recurrence during the 10-year follow-up period (odds ratio=1.16, 95% CI=1.03–1.31; z=2.33, p=0.02). Thus, for each successive episode of major depression, the risk of recurrence increased by 16%. The ICC from the mixed model was 0.20, which indicates that there was very little consistency in the time to recurrence within subjects.
Treatment
The highest level of pharmacotherapy received during any of the 4 weeks immediately preceding the onset of the five prospectively observed recurrences was examined. The low level of maintenance treatment was striking. During the 4 weeks immediately before the onset of the first three prospectively observed recurrences, 47%–50% of all subjects received no pharmacotherapy. During the 4 weeks immediately before the onset of the fourth and fifth prospectively observed recurrences, one-third of the subjects received no pharmacotherapy. During any of the 4-week periods immediately preceding the onset of the five prospectively observed recurrences, only 33% to 45% of the subjects received at least 100 mg/day of imipramine or its equivalent, and only 18% to 30% received at least 200 mg/day of imipramine or its equivalent.
By using the composite antidepressant score previously described, the mean level of treatment for the 4 weeks immediately preceding the recurrence was calculated for each of the five recurrences. For the first recurrence, the mean was 1.1 (SD=1.3); for the second, the mean was 1.1 (SD=1.3); for the third, the mean was 1.2 (SD=1.3); for the fourth, the mean was 1.4 (SD=1.3); and for the fifth recurrence, the mean was 1.6 (SD=1.5). (As noted earlier, a composite antidepressant score of 1 indicated a dose of 1–99 mg/day of imipramine or its equivalent, and a composite antidepressant score of 2 indicated a dose of 100–199 mg/day of imipramine or its equivalent.)
DISCUSSION
The length of prospective observation distinguishes the present study from previous investigations. By means of the current study and its 10 years of follow-up, we were in a better position to retain and assess the individuals whose course of illness was marked by a long interval from one recurrent episode to the next. This reduced the likelihood that the length of the observation period would condition or bias the results.
The probability of recurrence decreased for each successive 6-month interval after recovery, as shown by the mean average interval-specific probability of recurrence. In addition, the results within each row of table 2 show that for each recurrence, the rate of risk of recurrence fell as time elapsed. Both of these findings indicate that as the duration of recovery increases, the risk of recurrence decreases or decays (first prediction). Previous observational (3, 4) and treatment (16–19) studies have also found that the probability of a single recurrence of major depression declines over time. Similarly, in a study of subjects from the collaborative depression study with bipolar I disorder, the risk of recurrence decreased as the duration of recovery increased (20).
The findings from the mixed-effects model suggest that the probability of recurrence of major depression is significantly influenced by the number of lifetime episodes experienced before any recovery period or well interval. This confirms the second prediction that the probability of recurrence increases with each succeeding episode. With each successive recurrence, the risk of a subsequent recurrence increases by 16%. Thus, a patient with five lifetime episodes of major depressive disorder is more than twice as likely to suffer a recurrence than is a patient with one lifetime episode.
For the subjects with two or more prospectively observed episodes, the consistency in time to recurrence was low, as quantified by the ICC. This indicates that the time to recurrence is highly variable for any particular individual and accords with Kraepelin’s observation (21) that these patients experience a “sequence of attacks…between which pauses are interpolated of extraordinarily fluctuating duration” (p. 188).
One limitation of this study is that the cohort at risk for each succeeding prospective recurrence became progressively smaller. This was in part due to the subjects who did not recover and remained ill during follow-up and were therefore not at risk for recurrence. Also, the subjects who recovered and did not have a recurrence were not at risk for additional episodes. Thus, patients with relatively long intervals of illness or wellness were disproportionately excluded from successive analyses. As a result, the analyses underestimate the rates of recurrence over the lifetime of the patients. Even longer follow-up intervals would be required to more fully incorporate these subjects into the analyses and more accurately describe the course of illness for the entire study group.
Another limitation is that the analyses were restricted to episodes of major depression. Episodes of minor depression or intermittent depression were not included, with the net effect of underreporting the extent of psychopathology suffered by the study group.
This was an observational study, and treatment was not randomly assigned. As a result, treatment varied, and this may have influenced the findings. It is possible that some subjects recovered and discontinued treatment in the belief that they no longer required it and, by so doing, may have placed themselves at an increased risk for recurrence. It is also possible that the recurrence of major depressive disorder in patients receiving treatment may have left some of these patients feeling discouraged about treatment in general, with the result that they never pursued treatment again and were thus at increased risk for subsequent recurrence. Many of the subjects in the present study received little or no maintenance pharmacotherapy. This is unfortunate, given the findings from treatment studies (17–19) that indicate that maintenance therapy is efficacious in preventing recurrences.
Our findings can be summarized as follows. 1) After recovery from the index episode of unipolar major depression, the subjects suffered an average of two recurrences during 10 years of follow-up. 2) As the duration of recovery increased, the probability of recurrence decreased. 3) The probability of recurrence was significantly influenced by the lifetime number of episodes, such that the risk of recurrence increased by 16% with each successive recurrence. 4) The within-subject time to recurrence varied considerably from one recurrence to the next. 5) Many subjects received little or no maintenance treatment before recurrences.
Received Nov. 30, 1998; revised April 22, 1999; accepted July 18, 1999. From the Mood Disorders Program, Department of Psychiatry, Rhode Island Hospital; the Department of Psychiatry and Human Behavior, Brown University, Providence, R.I.; the Department of Psychiatry, Cornell University, New York; the Department of Health Policy and Research, Stanford University, Stanford, Calif.; the Department of Psychiatry, University of Iowa College of Medicine, Iowa City, Iowa; the Integrative Neuroscience of Schizophrenia, Mood, and Other Brain Disorders Program, NIMH, Bethesda, Md.; and the Department of Research and Training, New York State Psychiatric Institute, New York . Address reprint requests to Dr. Solomon, Mood Disorders Program, Department of Psychiatry, Rhode Island Hospital, 593 Eddy St., Providence, RI 02903-4970; [email protected] (e-mail)
 |
 |
1. American Psychiatric Association: Practice Guideline for Major Depressive Disorder in Adults. Am J Psychiatry 1993; 150(April suppl)Google Scholar
2. Katz MM, Secunda SK, Hirschfeld RMA, Koslow SH: NIMH clinical research branch collaborative program on the psychobiology of depression. Arch Gen Psychiatry 1979; 36:765–771Crossref, Medline, Google Scholar
3. Keller MB, Lavori PW, Lewis CE, Klerman GL: Predictors of relapse in major depressive disorder. JAMA 1983; 250:3299–3304Google Scholar
4. Lavori PW, Keller MB, Klerman GL: Relapse in affective disorders. J Psychiatr Res 1984; 18:13–25Crossref, Medline, Google Scholar
5. Belsher G, Costello CG: Relapse after recovery from unipolar depression: a critical review. Psychol Bull 1988; 104:84–96Crossref, Medline, Google Scholar
6. Endicott J, Spitzer RL: A diagnostic interview: the Schedule for Affective Disorders and Schizophrenia. Arch Gen Psychiatry 1978; 35:837–844Crossref, Medline, Google Scholar
7. Spitzer RL, Endicott J, Robins E: Research Diagnostic Criteria: rationale and reliability. Arch Gen Psychiatry 1978; 35:773–782Crossref, Medline, Google Scholar
8. Keller MB, Lavori PW, Friedman B, Nielsen E, Endicott J, McDonald-Scott P, Andreasen NC: The Longitudinal Interval Follow-Up Evaluation: a comprehensive method for assessing outcome in prospective longitudinal studies. Arch Gen Psychiatry 1987; 44:540–548Crossref, Medline, Google Scholar
9. Keller MB: Undertreatment of major depression. Psychopharmacol Bull 1988; 24:75–80Medline, Google Scholar
10. Kalbfleish JD, Prentice RL: The Statistical Analysis of Failure Time Data. New York, John Wiley & Sons, 1980Google Scholar
11. Leon AC, Friedman RA, Sweeney JA, Brown RP, Mann JJ: Statistical issues in the identification of risk factors for suicidal behavior: the application of survival analysis. Psychiatry Res 1990; 31:99–108Crossref, Medline, Google Scholar
12. Kaplan EL, Meier P: Nonparametric estimation from incomplete observations. J Am Statistical Assoc 1958; 53:457–481Crossref, Google Scholar
13. Hedeker D, Siddiqui O, Hu FB: Random-Effects Regression Analysis of Correlated Grouped-Time Survival Data: Technical Report. Chicago, University of Illinois at Chicago, Division of Epidemiology and Biostatistics, 1998Google Scholar
14. Siddiqui O, Hedeker D, Flay BR: Intraclass correlation estimates in a school-based smoking prevention study. Am J Epidemiol 1996; 144:425–433Crossref, Medline, Google Scholar
15. Hedeker D: MIXGSUR: A Computer Program for Mixed-Effects Grouped-Time Survival Analysis: Technical Report. Chicago, University of Illinois at Chicago, Division of Epidemiology and Biostatistics, 1998Google Scholar
16. Prien RF, Kupfer DJ, Mansky PA, Small JG, Tuason VB, Voss CB, Johnson WE: Drug therapy in the prevention of recurrences in unipolar and bipolar affective disorders. Arch Gen Psychiatry 1984; 41:1096–1104Google Scholar
17. Glen AIM, Johnson AL, Shepherd M: Continuation therapy with lithium and amitriptyline in unipolar depressive illness: a randomized, double-blind, controlled trial. Psychol Med 1984; 14:37–50Crossref, Medline, Google Scholar
18. Frank E, Kupfer DJ, Perel JM, Cornes C, Jarrett DB, Mallinger AG, Thase ME, McEachran AB, Grochocinski VJ: Three-year outcomes for maintenance therapies in recurrent depression. Arch Gen Psychiatry 1990; 47:1093–1099Google Scholar
19. Robinson DS, Lerfald SC, Bennett B, Laux D, Devereaux E, Kayser A, Corcella J, Albright D: Continuation and maintenance treatment of major depression with the monoamine oxidase inhibitor phenelzine. Psychopharmacol Bull 1991; 27:31–39Medline, Google Scholar
20. Coryell W, Endicott J, Maser JD, Mueller T, Lavori P, Keller M: The likelihood of recurrence in bipolar affective disorder. J Affect Disord 1995; 33:201–206Crossref, Medline, Google Scholar
21. Kraepelin E: Manic-Depressive Insanity and Paranoia. Translated by Barclay RM, edited by Robertson GM. Edinburgh, E & S Livingstone, 1921Google Scholar



