Further Evidence of Relation Between Prenatal Famine and Major Affective Disorder
Abstract
OBJECTIVE: In a previous study, the authors demonstrated an association between prenatal famine in middle to late gestation and major affective disorders requiring hospitalization. In this study, they sought to examine the association by using newly identified cases from the Dutch birth cohort used previously to examine the gender specificity of the association and to assess whether this relation is present for both unipolar and bipolar affective disorders. METHOD: The authors compared the risk of major affective disorder requiring hospitalization in birth cohorts who were and were not exposed, in each trimester of gestation, to famine during the Dutch Hunger Winter of 1944–1945. These cases of major affective disorder requiring hospitalization were newly ascertained from a national psychiatric registry. A larger data set from this registry was used for analysis by gender and diagnostic subtype. RESULTS: For the newly ascertained cases, the risk of developing major affective disorder requiring hospitalization was increased for subjects with exposure to famine in the second trimester and was increased significantly for subjects with exposure in the third trimester, relative to unexposed subjects. For the cases from the entire period of ascertainment, the risk of developing affective disorder was significantly increased for those exposed to famine during the second and the third trimesters of gestation. The effects were demonstrated for men and women and for unipolar and bipolar affective disorders. CONCLUSIONS: These results provide support for the authors’ previous findings on the association between middle to late gestational famine and affective disorder.
In a previous investigation (1), we demonstrated an increased risk of developing major affective disorder requiring hospitalization after middle to late gestational exposure to prenatal famine. This finding suggested that prenatal nutritional deficiency, or the factors associated with such exposure, might play an etiologic role in at least some proportion of the cases of affective disorder. We wish to further examine the relation of exposure to a famine, the Dutch Hunger Winter of 1944–1945, to major affective disorder in adulthood.
The results of our previous study support a neurodevelopmental hypothesis of affective disorder. Other investigations have provided findings consistent with this hypothesis. Individuals destined to develop affective disorder tend to show evidence of developmental impairment in childhood, including low educational test scores, later attainment of motor milestones, and speech defects (2), and are likely to show ventriculomegaly and cortical sulcal prominence (3); and they also have higher rates of birth in the winter and spring (4). Specific risk factors, including prenatal influenza (5, 6) and obstetric complications (7, 8), have been associated with an increased risk of developing affective disorder. Taken with a more extensive literature supporting the neurodevelopmental hypothesis of schizophrenia, these studies suggest that early developmental insults may have a spectrum of effects on psychiatric well-being.
The tragic circumstances of the Dutch Hunger Winter created a unique opportunity to examine the relation between exposure to prenatal famine and psychiatric illnesses requiring hospitalization, including major affective disorder. Precipitated by a Nazi blockade in the last year of World War II, the famine commenced in October 1944 and gradually worsened over the subsequent months, until liberation in early May 1945. From February to April 1945, the famine reached its peak, with high mortality, low fertility, and increased adverse birth outcomes (9). The famine primarily affected the cities of the western Netherlands. The brief, well-circumscribed nature of the famine, combined with the availability of an excellent documentation of food rations and a comprehensive database on psychiatric outcomes, permitted an unprecedented examination of the relation of prenatal nutritional deficiency during precisely defined periods of gestation to a spectrum of broadly and narrowly defined psychiatric disorders. In our first major report on psychiatric disorders in this cohort (10), we demonstrated a twofold higher risk of developing schizophrenia in the birth group exposed to severe famine in early gestation, a finding that was confirmed and refined in a subsequent study (11, 12).
Motivated by our initial finding on schizophrenia, we undertook a study (1) aimed at relating prenatal exposure to the Dutch Hunger Winter with major affective disorder in adulthood. In that investigation, the cumulative incidence of major affective disorder (given in ICD-9 [13] as diagnostic code 296) was compared in groups exposed and not exposed to the famine during each period of gestation. We demonstrated a significant association between exposure to prenatal famine during the second trimester and major affective disorder in adulthood; a lesser, but still significant, association was found between exposure to famine in the third trimester and affective disorder. For men, the effect was greater than twofold; for women, the risk was not significantly higher.
Despite these intriguing findings, several questions were left unanswered by this study. First, could the same or similar findings be demonstrated in a new group of patients with major affective disorder who were exposed to prenatal famine during the second and third trimesters? Second, did the lack of an association between prenatal famine and major affective disorder in women result from an insufficient number of cases? Third, did exposure to second- and third-trimester famine increase the risk of both unipolar and bipolar affective disorders, or was it specific to one or the other illness?
Fortunately, after publication of our earlier study (1), we obtained data from the Dutch national psychiatric registry covering additional periods of psychiatric hospitalization, which yielded a substantially greater number of cases. The data set from the earlier study included over 90% of all psychiatric hospitalizations in the Netherlands from 1978 to 1991. In the present study, the data set also included psychiatric hospitalizations from 1970 to 1977 and 1992 to 1996. These records of 13 additional years of psychiatric hospitalization included nearly as many cases of affective disorders as the data set of the earlier study. The additional cases enabled us to address each of the previous questions by permitting us to examine the association by using newly ascertained cases and to enhance our statistical power for further analyses by using cases identified over the entire period of ascertainment (1970–1996).
METHOD
The study was approved by the institutional review board of the New York State Psychiatric Institute and by the ethical committee of the Dutch psychiatric registry in accordance with the privacy laws of the Netherlands.
Definition of Birth Cohort
The birth cohort that constituted the focus of this study included subjects born from 1944 to 1946 in the six cities of western Holland with populations greater than 40,000. These cities were Amsterdam, The Hague, Haarlem, Leiden, Rotterdam, and Utrecht. The date of conception was inferred by assuming a full-term pregnancy. Cities in other regions of the Netherlands were not included in the present study because they did not experience severe famine and the number of cases was too few to permit a meaningful analysis.
Definition of Exposure
Exposure was defined as described by us in the previous study in Brown et al. (1), by using data on official food rations for the groups born in each of the 36 months from 1944 to 1946. The exposed birth groups were those who experienced severe food deprivation, defined as a mean intake of less than 1000 kcal/day over a trimester. As in our earlier study, we redefined the birth groups by trimester of exposure. The group exposed during the first trimester was born between August and December 1945, the group exposed during the second trimester was born between May and September 1945, and the group exposed during the third trimester was born between February and June 1945. Unexposed groups were defined as those with average daily rations that were 1000 kcal/day or more throughout gestation (born January 1944 to January 1945 or January 1946 to December 1946). Because the famine took place over an extended time interval, there is an overlap between successive trimesters of exposure. (Note that we are not using our refined definition of exposure [11]. That definition was specifically related to the hypothesis that prenatal famine is a risk factor for schizophrenia and is not appropriate in this study of affective disorder.)
Definition of Outcome
We first defined the population at risk for major affective disorder requiring hospitalization following the precedent of three earlier studies (1, 9, 10). The population consisted of men and women born in Holland from 1944 to 1946 who survived to at least age 18 years. The number at risk for each exposed birth group was therefore calculated by taking the number of live births and subtracting the number of deaths up to age 18.
The cases of major affective disorder requiring hospitalization (diagnostic code 296 in ICD-9) were ascertained by using the Dutch national psychiatric registry. The registry data consists of diagnoses recorded from psychiatric and university hospital inpatient admissions from 1970 to 1996. This diagnostic category is defined as “severe disturbances of mood (mania and/or depression) accompanied by mood-congruent psychotic symptoms.” In this diagnostic system, “psychosis” is more broadly defined than in DSM-III-R or DSM-IV, including significant neurovegetative features or other symptoms of “melancholia,” in addition to more classically described symptoms of psychosis such as delusions and hallucinations. Data for each case consisted of the most recent ICD-9 discharge diagnosis, place of birth, and week of birth.
For the first part of the study, we aimed to examine only newly ascertained cases of major affective disorder. In the previous study, cases were ascertained from the psychiatric registry from 1978 to 1991. Thus, for the present study, we first ascertained all cases of major affective disorder by using a recently acquired data set covering the years 1970 to 1996. Then, in order to ensure that only newly ascertained cases were examined, we excluded from this analysis all cases that were ascertained in our previous report.
In the second part of the study, we aimed to conduct further analyses (by gender and diagnostic subtype) that required a larger number of cases. For this purpose, we included all cases of major affective disorder requiring hospitalization that were ascertained from 1970 to 1996, the entire period of case ascertainment in the psychiatric registry. Thus, these analyses included individuals hospitalized from 1978 to 1991, who were included in our previous article.
In an analysis by ICD-9 diagnostic subtype, unipolar affective disorder was defined as manic-depressive psychosis, depressed type (296.1). Bipolar affective disorder was defined as any of the following ICD-9 subtypes: manic-depressive psychosis, manic type (296.0); manic-depressive psychosis, circular type but currently manic (296.2); manic-depressive psychosis, circular type but currently depressed (296.3); and manic-depressive psychosis, circular type, mixed (296.4).
Data Analysis
For the birth groups exposed to famine in each trimester, we calculated the cumulative incidence of hospitalization for major affective disorder for each group by dividing the number of subjects in the psychiatric registry with ICD-9 discharge diagnosis 296 by the number surviving to age 18. Each individual was counted only once for these analyses; for example, in the case of a subject hospitalized in 1975 and again in 1993 for a 296 diagnosis, only the latter hospitalization was counted.
For each trimester, the relative risk was obtained by calculating the ratio of the cumulative incidence of major affective disorder in exposed versus unexposed birth groups; 95% confidence intervals (CI) were computed by using the Taylor series (14, pp. 74–75). The null hypothesis of no association between famine exposure during each period of gestation and diagnosis was tested by using the chi-square statistic (14, p. 163).
RESULTS
Analysis by Time of Ascertainment
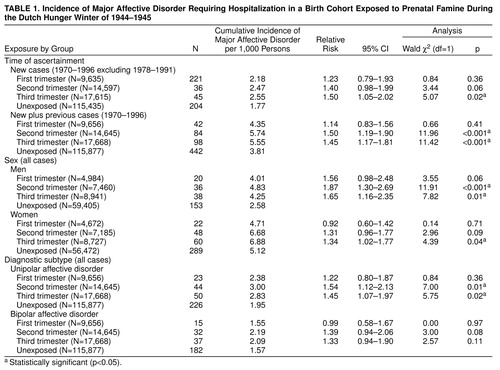
As previously discussed, we examined whether the findings of our previous study could be demonstrated by using the newly ascertained cases from the same famine-exposed Dutch birth groups. The results are summarized in table 1. The risk of major affective disorder requiring hospitalization (ICD-9 code 296) after prenatal famine was greater for exposure during the second and third trimesters than for unexposed subjects. There was no significant association between exposure to prenatal famine during the first trimester and major affective disorder requiring hospitalization. Although the second-trimester association fell short of significance, these findings are similar to those reported in our previous article (1).
We then examined the relation of prenatal famine to affective disorder, for cases from the entire period of ascertainment, including the cases examined in our previous article (1). The results are summarized in table 1. The risk of affective disorder requiring hospitalization was significantly greater after exposure to famine during the second and third trimesters. These results are similar in magnitude to those reported in our previous study (1).
Analysis by Sex
In these analyses, we examined the relation between prenatal famine during each trimester and major affective disorder separately for men and women, using cases from the entire period of ascertainment. The results are also summarized in table 1. For men, the relative risk of major affective disorder requiring hospitalization was significant following exposure to prenatal famine during the second and third trimesters. There was a nonsignificant increase in risk for first-trimester famine in men.
For women, the risk of major affective disorder was greater than normal, albeit nonsignificantly, following exposure to second-trimester famine and was significantly greater following third-trimester famine. There was no increased risk in women for exposure to first-trimester famine.
Analysis by Diagnostic Subtype
In these analyses, we examined the relation between exposure to prenatal famine during each trimester and major affective disorder by the two principal diagnostic subtypes, unipolar and bipolar affective disorders, again using cases from the entire period of ascertainment. The associations between exposure to prenatal famine during the second and third trimesters were evident for patients with unipolar and bipolar affective disorders, although these relations appeared to be stronger for patients with unipolar disorder than for bipolar disorder. These results are presented in table 1.
Separation of Effects of Prenatal Famine by Trimester
We conducted subsequent analyses in order to distinguish the effects of the individual trimesters on the risk of developing affective disorder. In men, we investigated whether the increased risk for affective disorder after first-trimester famine was due to the effect of second-trimester famine (because of the overlapping exposure times for these two trimesters). For this purpose, we divided the periods of exposure into “first trimester only” (born October to December 1945), “first plus second trimester” (born August to September 1945), and “second but not first trimester” (born May to July 1945). Among the men exposed during these three periods, the risk of developing major affective disorder was significantly increased only for the group exposed in the second but not first trimester (risk ratio=1.75, 95% CI=1.15–2.67; χ2=6.97, df=1, p=0.01); there was no significant increase in risk for those exposed in the first trimester only (risk ratio=1.25, 95% CI=0.64–2.45; χ2=0.44, df=1, p=0.51).
In women, we examined whether the second or third trimester was contributing to most or all of the observed effects. Therefore, we divided the periods of exposure into “second but not third trimester” and “third trimester only” categories. We found that exposure in each of these periods contributed nearly equally to the effect: “second but not third trimester,” risk ratio=1.33 (95% CI=0.89–1.99; χ2=1.98, df=1, p=0.16); “third trimester only,” risk ratio=1.26 (95% CI=0.90–1.76; χ2=1.80, df=1, p=0.18).
Moderate Famine Exposure
We next examined whether a dose-response relation existed between prenatal famine exposure and affective psychosis; in other words, was greater exposure to famine associated with a greater risk for affective psychosis? For this purpose, we examined the relation between prenatal famine and affective disorder by using birth cohorts exposed in utero to moderate famine (defined by Susser and Lin [10] as average rations of 1000–1500 kcal/day in a trimester) but not to severe famine at any time during gestation. The risk ratios were 0.92 (95% CI=0.63–1.35; χ2=0.17, df=1, p=0.68) for the first trimester, 1.11 (95% CI=0.82–1.51; χ2=0.47, df=1, p=0.49) for the second trimester, and 0.91 (95% CI=0.66–1.26; χ2=0.32, df=1, p=0.57) for the third trimester. Thus, our data are not compatible with a dose-response effect of prenatal famine exposure on the risk of developing affective disorder.
DISCUSSION
There are three major findings in the present study. First, in a group of newly ascertained cases from the same Dutch birth cohort, we have demonstrated findings similar to those reported in our earlier study of prenatal famine and affective disorder requiring hospitalization in adulthood (1). The results provide further support for the hypothesis that middle to late gestational nutritional deficiency—or its associated factors—plays a role in the etiology of major affective disorder. When we assume a causal relationship, the attributable risk percent allows us to estimate the proportion of cases of affective disorder in exposed subjects that is accounted for by prenatal malnutrition. For the birth groups exposed during the second and third trimesters, these values are 33.6% and 30.3%, respectively.
Second, using the larger data set afforded by the more recently ascertained cases, for the first time we have demonstrated an association between prenatal famine and major affective disorder in women. A significant effect was observed for exposure to famine during the third trimester, and a notable increase, albeit nonsignificant, was shown for exposure to famine in the second trimester. In regard to our previous study, it should be noted that the magnitudes of these effects were similar, which suggests that the negative finding for women in that study was due to inadequate statistical power. Although these new findings suggest that the relation between prenatal malnutrition and affective disorder may not be sex specific, these effects appear to be somewhat weaker in women than in men. Such differences might be explained in part by a greater vulnerability of men to prenatal insult (15) and by additional etiologic factors in women that may dilute the proportion of cases of affective disorder that are attributable to prenatal famine.
Third, our results suggest that exposure to famine during the second and third trimesters increases the risk of developing both unipolar and bipolar affective disorder. Although bipolar disorder has been demonstrated to be more familial/genetic with regard to etiology than unipolar affective disorder, the similarity in the effect sizes observed for these two disorders may perhaps be explained by our unique study group, which is clearly enriched for environmental etiologies. It should be further noted that these disorders may have been caused by different nutritional deficiencies or associated factors.
Potential Causal Mechanisms
There are two main causal mechanisms that should be considered. In the first, prenatal nutritional deficiency has a direct effect on the risk of developing major affective disorder. In the second, the effect of prenatal famine on the risk of affective disorder is mediated by another factor.
With regard to a direct effect of prenatal famine, it is difficult to attribute outcomes to any single dietary constituent because the diet was deficient in many micro- and macronutrients and both types of deficiency are important causes of neurodevelopmental disorder (16). As for micronutrients, prenatal folate deficiency causes neural tube defects, and prenatal iodine deficiency results in cretinism. As for general malnutrition, animal studies have shown that prenatal protein-calorie malnutrition markedly disrupts the development of brain structures, such as the hippocampus, and impairs the function of neurotransmitters, such as dopamine and serotonin (17).
Although there are no known nutritional deficits that occur exclusively in late gestation that have been linked to neurodevelopmental disorder (as in the relation between periconceptional folate deficiency and neural tube defects), a number of significant neurodevelopmental events occur during this time that may be relevant to the development of affective disorder. These events include the migration of neurons from the ventricular zone to the neocortex and neuronal differentiation (18, 19). Disturbances during these critical periods may have a variety of outcomes that could increase the vulnerability to psychiatric disorders, such as disrupted neuronal migration or impaired synaptic connections, evidence of which has been demonstrated in studies of schizophrenia (20, 21). In fact, some postmortem studies of affective disorder have also demonstrated ectopic neurons in the hippocampus (22), and neuroimaging studies of patients with affective disorder have shown ventriculomegaly and cortical sulcal prominence (3), which may be of neurodevelopmental origin.
With regard to the second potential mechanism, there are several scenarios involving factors that intervene between prenatal famine and affective disorder. In one example, severe famine increases maternal stress, which in turn has a neurotoxic effect on the development of the critical brain regions of causal relevance to affective disorder. The plausibility of this mechanism is supported by compelling data from animal studies indicating that marked stress early in development leads to long-term dysfunction of the hypothalamic-pituitary-adrenal axis similar to the abnormalities of the hormonal system found in major depression (23).
Relation to Previous Studies of Neurodevelopmental Factors and Affective Disorder
These findings complement an emerging literature that suggests that affective disorder may also have a neurodevelopmental etiology. For example, van Os et al. demonstrated lower educational test scores, later attainment of motor milestones, and speech defects (2) among children destined to develop affective disorder. In addition, higher rates of birth during the winter and spring months have been demonstrated in patients with bipolar disorder, a finding that may be explained by viral epidemics later in gestation (4).
Relation to Previous Findings Regarding Prenatal Famine and Schizophrenia
We now consider a new interpretation of our previous findings on the Dutch Hunger Winter and schizophrenia/schizophrenia spectrum disorder in light of the results in the present study. Briefly, these studies demonstrated a clear peak in the risk of schizophrenia and of schizoid/schizotypal personality disorder in the birth cohort exposed to severe famine during early gestation. These effects were greater than twofold and statistically significant (10–12). Taking these findings together with the findings of the present study, one may speculate, as did Crow (24) in regard to genetic etiologies, that there is a continuum of psychiatric disorders, from affective disorder to schizophrenia, and that, furthermore, the severity and type of disorders along this continuum are related to the gestational timing of prenatal famine. In this paradigm, early gestational famine gives rise to schizophrenia, whereas later gestational famine gives rise to affective disorder. Of course, this interpretation could be an oversimplification, since, as just mentioned, prenatal famine encompasses diverse nutritional and nonnutritional factors; thus, these two disorders could each be caused by different etiologic factors related to prenatal famine. Nonetheless, it is our view that this approach to a synthesis of findings provides an intriguing heuristic model for future studies of prenatal environmental risk factors for psychiatric disorders.
Limitations
Most of our study’s limitations are provided in previous publications (10–12). Briefly, they include 1) the use of chart diagnoses rather than direct assessments using research diagnostic criteria, which may contribute to diagnostic misclassification; 2) the use of group rather than individual data, although exposure was pervasive in the population; 3) the lack of information on particular nutrients in the diet; 4) the assumption of full-term pregnancy in estimating the time of exposure on the basis of the time of birth, although the vast majority of births occurred at full term; and 5) the lack of adjustment for potential confounders, such as social class and familial liability to affective disorders. In regard to social class, however, the exposed birth cohorts were weighted toward the upper social classes, which tend to reduce the estimated relative risks, rather than create spurious associations. In regard to family liability, the selective fertility of women genetically predisposed to major affective disorder might be invoked to explain our findings. However, we do not believe that our findings can be explained by selective fertility because decreased fertility occurred only in those exposed to famine early in gestation (9). Finally, it should be acknowledged that, generally speaking, all of the odds ratios were relatively small, which suggests that prenatal nutrition plays only a contributory role in the etiology of affective disorder in our cohort.
CONCLUSIONS
These findings provide further evidence that prenatal malnutrition in middle to late gestation, or its associated factors, may play a role in the etiology of major affective disorder. We have demonstrated the effects for men and women and for unipolar and bipolar affective disorders. This study adds to a growing body of literature indicating a neurodevelopmental basis for the development of major affective disorder. Future studies should be conducted to confirm the association between prenatal famine and affective disorder by using direct diagnostic interviews to examine the neurodevelopmental basis of this relation and to explore potential interactions with genetic vulnerability.
Received Dec. 8, 1998; revision received May 25, 1999; ac- cepted June 17, 1999. From the Department of Psychiatry, College of Physicians and Surgeons, Columbia University, New York; and the New York State Psychiatric Institute. Address reprint requests to Dr. Brown, New York State Psychiatric Institute, 1051 Riverside Dr., Unit 2, New York, NY 10032; [email protected] (e-mail). Supported by NIMH grant MH-01206 (Dr. Brown), a New York State Psychiatric Institute Research Support Grant (Dr. Brown), and the Theodore and Vada Stanley Foundation (Dr. van Os). The authors thank Pieter Bosch and Constance van Rooijen of the Dutch Psychiatric Registry for their help.
 |
1. Brown AS, Susser ES, Lin SP, Neugebauer R, Gorman JM: Increased risk of affective disorder in males after second trimester prenatal exposure to the Dutch Hunger Winter of 1944–1945. Br J Psychiatry 1995; 166:601–606Crossref, Medline, Google Scholar
2. van Os J, Jones P, Lewis G, Wadsworth M, Murray R: Developmental precursors of affective illness in a general population birth cohort. Arch Gen Psychiatry 1997; 54:625–631Crossref, Medline, Google Scholar
3. Elkis H, Friedman L, Wise A, Meltzer H: Meta-analysis of studies of ventricular enlargement and cortical sulcal prominence in mood disorder: comparisons with controls or patients with schizophrenia. Arch Gen Psychiatry 1995; 52:735–746Crossref, Medline, Google Scholar
4. Torrey E, Rawlings R, Ennis J, Merrill D, Flores D: Birth seasonality in bipolar disorder, schizophrenia, schizoaffective disorder and stillbirths. Schizophr Res 1996; 21:141–149Crossref, Medline, Google Scholar
5. Machon R, Mednick S, Huttunen M: Adult major affective disorder after prenatal exposure to an influenza epidemic. Arch Gen Psychiatry 1997; 54:322–328Crossref, Medline, Google Scholar
6. Cannon M, Cotter D, Coffey V, Sham P, Takei N, Larkin C, Murray R, O’Callaghan E: Prenatal exposure to the 1957 influenza epidemic and adult schizophrenia: a follow-up study. Br J Psychiatry 1996; 168:368–371Crossref, Medline, Google Scholar
7. Sacker A, Done D, Crow T, Golding J: Antecedents of schizophrenia and affective illness: obstetric complications. Br J Psychiatry 1995; 166:734–741Crossref, Medline, Google Scholar
8. Done D, Johnstone E, Frith C, Golding J, Shepherd PM, Crow TJ: Complications of pregnancy and delivery in relation to psychosis in adult life: data from the British Perinatal Mortality Survey sample. Br Med J 1991; 302:1576–1580Google Scholar
9. Stein Z, Susser M, Saenger G, Marolla F: Famine and Human Development: The Dutch Hunger Winter of 1944–45. New York, Oxford University Press, 1975Google Scholar
10. Susser ES, Lin SP: Schizophrenia after prenatal exposure to the Dutch Hunger Winter of 1944–1945. Arch Gen Psychiatry 1992; 49:983–988Crossref, Medline, Google Scholar
11. Susser E, Neugebauer R, Hoek H, Brown AS, Lin S, Labovitz D, Gorman JM: Schizophrenia after prenatal famine: further evidence. Arch Gen Psychiatry 1996; 53:25–31Crossref, Medline, Google Scholar
12. Susser E, Hoek HW, Brown A: Neurodevelopmental disorder after prenatal famine: the story of the Dutch Famine Study. Am J Epidemiol 1998; 147:213–216Crossref, Medline, Google Scholar
13. World Health Organization: Mental Disorders: Glossary and Guide to Their Classification in Accordance With the Ninth Revision of the International Classification of Diseases. Geneva, WHO, 1978Google Scholar
14. Fleiss J: Statistical Methods for Rates and Proportions, 2nd ed. New York, John Wiley & Sons, 1981Google Scholar
15. Kline J, Stein Z, Susser M: Conception to Birth: Epidemiology of Prenatal Development: Monographs in Epidemiology and Biostatistics, vol 1. New York, Oxford University Press, 1989Google Scholar
16. Brown AS, Susser ES, Butler PD, Richardson-Andrews R, Kaufmann CA, Gorman JM: Neurobiological plausibility of prenatal nutritional deprivation as a risk factor for schizophrenia. J Nerv Ment Dis 1996; 184:71–85Crossref, Medline, Google Scholar
17. Butler PD, Susser ES, Brown AS, Kaufmann CA, Gorman JM: Prenatal nutritional deprivation as a risk factor in schizophrenia: preclinical evidence. Neuropsychopharmacology 1994; 11:227–235Crossref, Medline, Google Scholar
18. Rakic P: Defects of neuronal migration and the pathogenesis of cortical malformations. Prog Brain Res 1988; 73:15–37Crossref, Medline, Google Scholar
19. Nowakowski RS: Prenatal development of the brain, in Prenatal Exposures in Schizophrenia. Edited by Susser ES, Brown AS, Gorman JM. Washington, DC, American Psychiatric Press, 1999, pp 61–85Google Scholar
20. Akbarian S, Bunney W, Potkin S, Wigal S, Hagman J, Sandman C, Jones E: Altered distribution of nicotinamide-adenine dinucleotide phosphate-diaphorase cells in frontal lobe of schizophrenics implies disturbances of cortical development. Arch Gen Psychiatry 1993; 50:169–177Crossref, Medline, Google Scholar
21. Jakob J, Beckman H: Prenatal developmental disturbances in the limbic allocortex in schizophrenics. J Neural Transm 1986; 65:303–326Crossref, Medline, Google Scholar
22. Beckman H, Jakob J: Prenatal disturbances of nerve cell migration in the entorhinal region: a common vulnerability factor in functional psychoses? J Neural Transm Gen Sect 1991; 84:155–164Google Scholar
23. Heim C, Owens M, Plotsky P, Nemeroff C: Persistent changes in corticotropin-releasing factor systems due to early life stress: relationship to the pathophysiology of major depression and posttraumatic stress disorder. Psychopharmacol Bull 1997; 33:185–192Medline, Google Scholar
24. Crow TJ: The continuum of psychosis and its implication for the structure of the gene. Br J Psychiatry 1986; 149:419–429Crossref, Medline, Google Scholar



