The Psychiatric Symptoms of Rheumatic Fever
Abstract
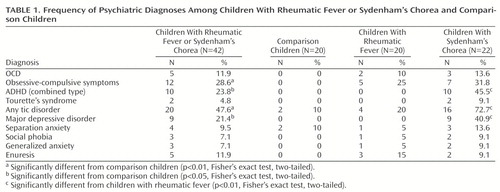
OBJECTIVE: This study examined the frequency and age at onset of psychiatric disorders among children with rheumatic fever, Sydenham’s chorea, or both and a comparison group. METHOD: Twenty children with rheumatic fever, 22 with Sydenham’s chorea, and 20 comparison children were assessed by means of a semistructured interview and rating scales for tic disorders and obsessive-compulsive disorder. RESULTS: Obsessive-compulsive symptoms were more frequent in both the Sydenham’s chorea and rheumatic fever groups than in the comparison group. The Sydenham’s chorea group had a higher frequency of major depressive disorder, tic disorders, and attention deficit hyperactivity disorder (ADHD) than both the comparison and rheumatic fever groups. ADHD symptoms were associated with a higher risk of developing Sydenham’s chorea. CONCLUSIONS: Both the rheumatic fever and Sydenham’s chorea groups were associated with a higher risk of developing neuropsychiatric disorders than the comparison group. ADHD appears to be a risk factor for Sydenham’s chorea in children with rheumatic fever.
Rheumatic fever is an autoimmune disorder that occurs after infection by specific strains of β-hemolytic streptococci. Sydenham’s chorea, the late central nervous system expression of rheumatic fever, has been associated with higher rates of psychiatric disorders, such as obsessive-compulsive disorder (OCD), tic disorders, major depressive disorder, and attention deficit hyperactivity disorder (ADHD), than those found in comparison patients (1–3).
In the present study, we systematically assessed the presence and the age at onset of neuropsychiatric symptoms in patients with rheumatic fever, with and without Sydenham’s chorea, and a matched comparison group to determine the frequency and onset of psychiatric disorders.
Method
All consecutively admitted patients with acute rheumatic fever and Sydenham’s chorea from two academic hospitals in São Paulo, Brazil, were assessed over an 18-month period (4). The exclusion criteria were age less than 5 years or more than 16 years or the presence of other neurological disorders. A comparison group of children was matched for age and gender with the rheumatic fever group and included children who were either seen in the outpatient clinic or hospitalized for nonautoimmune medical disorders. Written informed consent was obtained from all patients and their parents.
Rheumatic fever diagnoses were made according to the modified Jones criteria (5) by a pediatrician (M.H.K.). A child neurologist (M.J.M-D.) performed a complete neurological evaluation to rule out other forms of chorea in the patients with Sydenham’s chorea. None of the children in either group had previously been referred for a psychiatric evaluation. A child psychiatrist (M.T.M.) interviewed all probands and their parents. Best-estimate psychiatric diagnoses were made according to the DSM-IV criteria after administration of the Schedule for Affective Disorders and Schizophrenia for School-Age Children—Epidemiologic Version (6), which includes questions regarding age at onset of psychiatric symptoms. Although an effort was made to maintain blindness in this study, it proved impossible regarding subjects in the group with Sydenham’s chorea because of their overt symptom profiles.
The Yale-Brown Obsessive Compulsive Scale (7) and the Yale Global Tic Severity Scale (8) were used to determine symptom severity. In order to differentiate choreiform movements from tics, we emphasized the presence of vocal tics in making a diagnosis of tic disorders. When motor tics could not be distinguished from choreic movements, a diagnosis of tic disorders was not made.
Comparisons of categorical variables among groups were performed by means of Pearson’s chi-square analysis and Fisher’s exact test for two-by-two tables. Comparisons of continuous variables were carried out by means of ANOVA (Student’s t test for the comparison of two groups). The ages at onset were compared by means of paired-samples t tests. Significance values of p<0.05 were used in all analyses. Stepwise backward logistic regressions were also performed to establish the risk for the development of Sydenham’s chorea, given the presence of other comorbid conditions.
Results
There were no significant between-group differences in demographic characteristics when the data were stratified by referral source. The mean ages of the rheumatic fever, Sydenham’s chorea, and comparison groups were 10.7 years (SD=2.7), 10.6 years (SD=2.8), and 10.7 years (SD=2.7), respectively (age: F=0.02, df=2, 59, n.s.; sex: χ2=3.18, df=2, n.s.).
The rates of psychiatric disorders are shown in Table 1. Both the Sydenham’s chorea and rheumatic fever groups had higher rates of obsessive-compulsive symptoms, tic disorders, ADHD, and major depressive disorder than the comparison subjects (Table 1). Compared to the rheumatic fever group, the Sydenham’s chorea group showed no difference in the rate of obsessive-compulsive symptoms, but the group with Sydenham’s chorea was at greater risk for ADHD, tic disorders, and major depressive disorder. The onsets of major depressive disorder, obsessive-compulsive symptoms, and tic disorders were contemporaneous or subsequent to the onset of rheumatic fever in 89% (8 of 9), 42% (5 of 12), and 55% (11 of 20) of the cases, respectively. But in 90% (9 of 10) of the cases of ADHD, age at onset was significantly earlier than for rheumatic fever (rheumatic fever or Sydenham’s chorea: mean=10.6 years, SD=2.7, versus ADHD: mean=6.7 years, SD=2.2) (t=5.40, df=9, p<0.01, Student’s t test).
The presence or absence of ADHD symptoms was a predictor for the risk of developing Sydenham’s chorea in this study group. Specifically, if a child with rheumatic fever had an antecedent history of ADHD, combined type, he or she had a markedly higher risk of developing Sydenham’s chorea (95%) than did rheumatic fever patients without such a history (36%) (symptoms of inattention: B=1.40, Wald’s χ2=2.32, df=1, p=0.13; symptoms of hyperactivity or impulsive behavior: B=2.20, Wald’s χ2=3.71, df=1, p=0.05).
Discussion
Similar to earlier reports, this study found major depressive disorder, tic disorders, and ADHD to be more frequent in patients with Sydenham’s chorea than in patients with rheumatic fever (1, 2). Although the frequency for obsessive-compulsive symptoms was higher in the rheumatic fever and Sydenham’s chorea groups than in the comparison group, we found obsessive-compulsive symptoms to be present equally in both the rheumatic fever and Sydenham’s chorea groups. On the basis of the results of earlier studies (1, 2), this finding was unexpected. This difference may be explained by the small group sizes, the cross-sectional design, and the differences in assessment methods, including the fact that the individual responsible for the best-estimate diagnoses was aware of the subjects’ initial group assignments. The present study also differed from previous investigations by its ascertainment of patients in the acute phase of their illness (4) and in their first episode of rheumatic fever or Sydenham’s chorea. Subsequently, we monitored each of the children with rheumatic fever and diagnosed with either obsessive-compulsive symptoms or OCD. Thus far, over the ensuing 12–24 months, none of these children has developed Sydenham’s chorea.
In this study, a systematic comparison of age at onset for different neuropsychiatric disorders allowed us to determine the temporal relationship among the different syndromes. For a number of individuals, there was a simultaneous beginning of the rheumatic or choreic symptoms, the tic disorders, and the psychiatric symptoms of major depressive disorder and OCD. This finding is consistent with an autoimmune process being associated with both movement and neuropsychiatric disorders (i.e., mental disorders due to a general medical condition) (DSM-IV) (1, 2, 9). However, a substantial number of individuals reported the onset of ADHD, tic disorders, and obsessive-compulsive symptoms before the occurrence of rheumatic fever. Although, the significance of these findings is unclear, they suggest that in some cases, ADHD, tic disorders, and obsessive-compulsive symptoms may reflect a vulnerability to developing rheumatic fever and Sydenham’s chorea. Future longitudinal studies are necessary to evaluate whether these psychiatric symptoms represent the early expression of an autoimmune process triggered by streptococcus infections (9) or evidence of an increased central nervous system vulnerability to rheumatic fever and Sydenham’s chorea due to some other cause.
 |
Presented in part at the Congress of the International Association for Child and Adolescent Psychiatry and Allied Professions, Stockholm, August 2–7, 1998. Received Nov. 23, 1998; revisions received Dec. 15, 1999, and June 1, 2000; accepted July 5, 2000. From the Departments of Psychiatry and Pediatrics, Medical School, University of São Paulo, São Paulo, Brazil; and the Child Study Center, School of Medicine, Yale University. Address reprint requests to Dr. Mercadante, Child Study Center, Yale University, 230 South Frontage Rd., P.O. Box 207900, New Haven, CT 06520-7900; [email protected] (e-mail). Supported in part by grants from the Fundação de Amparo à Pesquisa do Estado de São Paulo (5012-7, 5013-3, 11991-0, and 7525-0) and the Conselho Nacional de Desenvolvimento Científico e Tecnológico (521369) to Drs. Miguel and Mercadante and from NIMH (MH-01527 and MH-49351) to Drs. Lombroso and Leckman. The authors thank Drs. José Alberto del Porto, Orlando Barreto, Vanda Bastos, Eunice Mitiko Ocuda, and Silvana Brasilia Sachetti for reviewing this manuscript.
1. Swedo SE, Rapoport JL, Cheslow DL, Leonard HL, Ayoub EM, Hosier DM, Wald ER: High prevalence of obsessive-compulsive symptoms in patients with Sydenham’s chorea. Am J Psychiatry 1989; 146:246–249Link, Google Scholar
2. Asbahr FR, Negrão AB, Gentil V, Zanetta DM, da Paz JÁ, Marques-Dias MJ, Kiss MH: Obsessive-compulsive and related symptoms in children and adolescents with rheumatic fever with and without chorea: a prospective 6-month study. Am J Psychiatry 1998; 155:1122–1124Google Scholar
3. Mercadante MT, Campos MC, Marques-Dias MJ, Miguel EC, Leckman J: Vocal tics in Sydenham’s chorea. J Am Acad Child Adolesc Psychiatry 1997; 36:305–306Crossref, Medline, Google Scholar
4. Taranta A, Markowitz M: A Febre Reumática. Lancaster, UK, Kluwer Academic, 1989Google Scholar
5. American Heart Association: Jones criteria (revised) for guidance in the diagnosis of rheumatic fever. Circulation 1984; 69:204Google Scholar
6. Orvaschel H, Puig-Antich J: Schedule for Affective Disorders and Schizophrenia for School-Age Children—Epidemiologic Version (K-SADS-E), 4th revision. Pittsburgh, Western Psychiatric Institute and Clinic, 1987Google Scholar
7. Goodman WK, Price LH, Rasmussen SA, Mazure C, Delgado P, Heninger GR, Charney DS: The Yale-Brown Obsessive Compulsive Scale, II: validity. Arch Gen Psychiatry 1989; 46:1012–1016Google Scholar
8. Leckman JF, Riddle MA, Hardin MT, Ort SI, Swartz KL, Stevenson J, Cohen J: The Yale Global Tic Severity Scale: initial testing of a clinician-rated scale of tic severity. J Am Acad Child Adolesc Psychiatry 1989; 28:566–573Crossref, Medline, Google Scholar
9. Swedo SE, Leonard HL, Kiessling LS: Speculations on antineuronal antibody-mediated neuropsychiatric disorders of childhood. Pediatrics 1994; 93:323–326Medline, Google Scholar



