Alcohol Use and Anxiety: Diagnostic and Management Issues
“Ms. M” is a 40-year-old Caucasian female who presents with complaints of anxiety and sleep disturbance. She recently went through a difficult divorce after 14 years of marriage, and she has two children, ages 8 and 10. She was trained as a nurse and had stopped working when her first child was born, but she is now working as a school nurse. She reports feeling anxious about everything, including financial issues, the well-being of her children, and her competence at work. She has a great deal of difficulty falling asleep. Approximately 3 months ago, she began to drink wine at night to help her sleep. She has gradually increased her drinking and is currently drinking 2–3 glasses of wine (4 ounces each) per night on average, but on several nights within the past month she drank a 32-ounce bottle of wine by herself. Her father was an alcoholic, and she worries about her drinking. She reports binge drinking during adolescence and in college and recalls having one “blackout.” After she met her husband 18 years ago, her drinking decreased considerably because he drank alcohol only occasionally and disapproved of her drinking. They kept little alcohol in the house and she drank only socially. She says that since childhood she has felt extremely anxious in social settings and that drinking alcohol always helped to “take the edge off.” She has several close friends and is involved in her church community.
Evaluation and Diagnosis of Alcohol Use Disorders
Alcohol use disorders are among the most common psychiatric disorders, yet they are underdiagnosed and often go untreated. There are a number of reasons why a physician might fail to make a diagnosis of an alcohol use disorder. Denial is a core feature of the illness, so individuals with an alcohol problem often have limited insight into the impact their consumption has on their life and well-being. The social stigma attached to alcohol use disorders may also make it difficult for patients to fully disclose the extent and consequences of their alcohol use. This is particularly problematic for women, and women who have an alcohol problem are less likely than men to be diagnosed (1) .
Assessment of drug and alcohol use should be a routine part of psychiatric evaluation. Some standardized screening questionnaires (for example, the four-item CAGE screening test) focus on identification of alcohol dependence. The 10-item Alcohol Use Disorders Identification Test (AUDIT; 2) asks specific questions about alcohol consumption patterns (see Figure 1 ) and is likely to be more useful in detecting the spectrum of unhealthy drinking patterns (3) . The National Institute on Alcohol Abuse and Alcoholism has defined “at-risk drinking” as consuming more than seven drinks per week or three drinks per occasion for women and more than 14 drinks per week or four drinks per occasion for men (4) . In approaching the patient, using a nonjudgmental interview style and open-ended questions about specific quantities of alcohol use is likely to be the most successful way to gain information about alcohol use that might be considered unhealthy use. However, the threshold for “safe” alcohol consumption may be lower for patients who have psychiatric disorders that have a high risk of comorbidity with alcoholism, such as mood and anxiety disorders, and those who have a strong family history of alcohol use disorders, such as the patient in the case example.
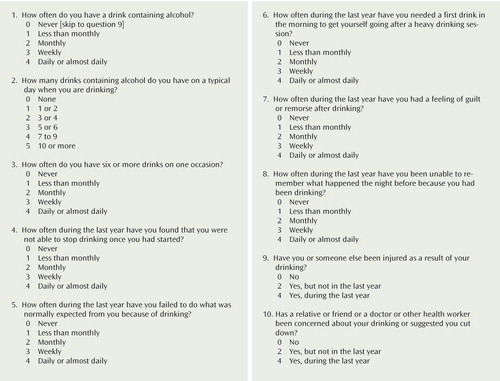
a A total score of 8 or higher on the AUDIT suggests a need for further evaluation. Specific questions or sets of questions serve as indicators of specific factors or risks. Questions 1–3 can be summed as a consumption subscore, questions 4–6 as a dependence subscore, and questions 7–10 as an alcohol-related problems subscore. For more information, see the World Health Organization’s guidelines for use of the AUDIT (2).
Patients with risky alcohol use patterns who do not meet criteria for alcohol dependence may not be motivated to participate in alcohol-related treatment or may not accept abstinence as a goal. The “brief intervention” approach to treating such patients refers to a spectrum of office-based interventions generally consisting of 10–15 minutes of counseling to provide feedback, advice, and goal setting in relation to alcohol use, with follow-up visits to assess changes (5) . These interventions, delivered in a variety of office-based settings, have efficacy in decreasing alcohol consumption in nondependent drinkers. Treatment goals that are focused on reducing alcohol consumption, although somewhat controversial, may be more palatable than abstinence-based treatments for some patients with unhealthy alcohol use. These “controlled drinking” models, including behavioral self-control training, moderation-oriented cue exposure, and guided self-change, have yielded substantial reductions in alcohol use, which are sustainable over time for some individuals (6) . It is not clear what characteristics best predict which individuals can successfully reduce drinking to an acceptable level, so controlled drinking strategies should be approached with caution.
Comorbidity of Anxiety and Alcohol Use Disorders
The relationship between anxiety, anxiety disorders, and alcohol use is complex and bidirectional. While tension-reduction hypotheses of alcohol use and misuse suggest that acute use of alcohol reduces anxiety, laboratory studies with human subjects have shown an inconsistent relationship between alcohol ingestion and anxiety, and alcohol withdrawal is clearly associated with increased anxiety. A number of epidemiologic studies have demonstrated high comorbidity between alcohol use and anxiety disorders, but these studies are not designed to shed light on causal connections (7 , 8) . In a classic review of the literature from epidemiologic, family, and field studies, Kushner and colleagues concluded that the relationship between alcohol problems and anxiety appears to be variable among the anxiety disorders (9) . For social phobia and agoraphobia, alcohol problems tend to begin after the onset of the anxiety disorder, and many patients report initiating alcohol use as an attempt to control anxiety. Generalized anxiety disorder and panic disorder tend to begin after or at the same time as problem drinking, and the symptoms of these disorders can be indistinguishable from symptoms of alcohol withdrawal. This suggests that there may be more difficulty in diagnosing these disorders in the face of active alcohol use and that alcohol use may exacerbate symptoms of anxiety or unmask a vulnerability to these disorders. In any case, a simple unidirectional causal relationship between alcohol use and anxiety in clinical settings is not likely to be established. Alcohol has the potential to interact with anxiety in an upward spiral, leading to increased severity of both the anxiety disorder and problem drinking (9) . Alcohol consumption may be motivated by short-term relief of anxiety, but it ultimately leads to increased anxiety as a result of hyperexcitability of the autonomic nervous system associated with alcohol withdrawal and the anxiety-inducing environmental disruptions caused by excessive alcohol use.
In diagnosing coexisting anxiety disorders, the gold standard has been to delay establishing a diagnosis until after a period of monitored abstinence. The length of that period may vary among psychiatric diagnoses. In general, disorders that have considerable symptom overlap in withdrawal states (e.g., dysthymia and generalized anxiety disorder) are likely to require longer periods of abstinence for accurate diagnosis. Disorders whose key symptoms are not mimicked by withdrawal states (e.g., obsessive-compulsive disorder and social phobia) can be diagnosed with greater confidence after shorter periods of abstinence. In Ms. M’s case, a diagnosis of social phobia might be made after the initial evaluation. Although Ms. M also describes symptoms consistent with generalized anxiety disorder, these symptoms could be a result of current stressors, and they may be exacerbated by alcohol consumption. It would be difficult to diagnose generalized anxiety disorder until after abstinence has been attained.
Stress and Alcohol Use
The relationship between stressful life events and substance use disorders is also complex. Animal studies have consistently demonstrated that a variety of stressors lead to increased self-administration of substances of abuse (10) . Corticotropin-releasing factor (CRF), one of the key hormones involved in the stress response, has been implicated in stress-induced self-administration in animals and has also been implicated in the pathophysiology of anxiety and affective disorders (11) . Stress stimuli that activate CRF circuits also potentiate mesolimbic dopaminergic reward pathways in laboratory animals, and thus stress may actually increase the reinforcing properties of substances of abuse (10) ; this process provides a neurobiologic explanation for the connection between substance use, relapse, and environmental stressors. Similarly, laboratory studies with human subjects have shown that emotional stress and negative affect states increase craving in substance-dependent individuals (12) . Evidence of altered neuroendocrine response to stress challenges in individuals with alcohol use disorders is consistent with clinical observations that individuals with substance use disorder have difficulty managing emotional distress states and may be vulnerable to relapse in the face of stressful situations (13) .
Treatment Options
Psychotherapy
There are a number of efficacious psychotherapeutic approaches to the treatment of alcohol use disorders. In a multisite trial supported by the National Institute on Alcohol Abuse and Alcoholism, cognitive behavior therapy, 12-step facilitation, and brief motivational therapy were found to be equally efficacious in improving alcohol-related outcomes during 1-year follow-up (14) . The results did not support hypotheses concerning individual characteristics that might predict differential response to treatment. However, individuals with higher scores on the psychiatric subscales of the Addiction Severity Index had better outcomes when treated with cognitive behavior therapy as compared with the other interventions, which supports the use of cognitive behavior therapy in individuals with alcohol dependence and psychiatric comorbidity.
The importance of social support systems for individuals in recovery should not be underestimated. Alcoholics Anonymous (AA) and other 12-step programs are widely available and cost free, and they can be an important first step and an invaluable source of support, companionship, and strength. In the case presented, given Ms. M’s social anxiety, making the initial contact with an AA group may be difficult. It might be helpful for the clinician to provide “coaching” about AA attendance and for Ms. M to attend a first meeting with a known support person.
Another issue in this case is optimal psychotherapeutic treatment for anxiety disorders. For individuals with co-occurring substance use and psychiatric disorders, the timing of the treatment of one disorder relative to treatment of the other can be important. For Ms. M, nonspecific anxiety reduction techniques commonly used to promote relapse prevention in substance abuse treatment (e.g., relaxation therapy and progressive muscle relaxation) may be sufficient to reduce the patient’s generalized anxiety. The treatment of social phobia or other anxiety disorders for which exposure-based therapy is indicated is more problematic. Exposure-based therapies, which involve having individuals face feared stimuli and use new coping strategies, have demonstrated efficacy in the treatment of a number of anxiety disorders (15) . However, exposure-based therapy is anxiety provoking. In the treatment of posttraumatic stress disorder (PTSD), the use of exposure-based therapy during early recovery has been questioned because of the belief that provoking anxiety during early stages of recovery might lead to relapse. Preliminary studies show that individuals with co-occurring PTSD and substance use can benefit from exposure-based therapy in combination with relapse prevention skills training (16) . The most appropriate psychotherapeutic approach to co-occurring social phobia and substance dependence needs further exploration. While exposure to social situations is inevitable and can be therapeutic, it is important to ensure that the patient has a firm grasp of relapse prevention strategies, and in particular strategies that would be helpful in managing anxiety in social settings without drinking.
Pharmacotherapy
An important issue in Ms. M’s case is whether to use medications and, if so, which ones. In the treatment of social phobia, selective serotonin reuptake inhibitors (SSRIs) are the first-line treatment and have demonstrated efficacy in a number of placebo-controlled trials (15) . The effectiveness of SSRIs in co-occurring social phobia and alcohol dependence is not well studied. Two small randomized trials demonstrated a positive impact on anxiety outcomes but no impact on alcohol-related outcomes (17 , 18) . Although buspirone treatment of anxious alcohol-dependent subjects was associated in one study (19) with decreases in both anxiety and alcohol consumption, the study did not include individuals with social phobia.
The use of SSRIs in reducing alcohol consumption remains controversial. Despite consistent evidence that SSRI treatment reduces alcohol intake in animal models, results of clinical studies are inconsistent (20) . Much of this variability may be related to heterogeneity of the study populations. Recent work suggests that subtypes of alcoholism are differentially responsive to treatment with SSRIs. In several studies, alcohol-dependent individuals with a later onset and less severe dependence had a better response to SSRIs, whereas early onset and more severe dependence predicted poor response (21) .
Pharmacotherapeutic management of alcohol withdrawal may be an issue in this case, although the pattern and amount of alcohol consumption described may not be associated with physical withdrawal. Although symptoms of withdrawal can range from mild to life threatening, alcohol withdrawal is often mild and easily managed. Severe withdrawal is generally associated with high levels of alcohol use, although the relationship between the amount of consumption and withdrawal symptoms is highly variable. Benzodiazepines are currently the only medication class proven to treat withdrawal (22) , although there is accumulating evidence that some anticonvulsants can also be useful.
The range of pharmacologic treatment options for relapse prevention in alcohol dependence is growing, but the utility of available agents in reducing nondependent problem drinking has not been established. Naltrexone, acamprosate, and disulfiram have all received approval from the Food and Drug Administration for relapse prevention in alcohol-dependent individuals (23) . Disulfiram (250 or 500 mg/day) is an aversive agent that causes a buildup of a toxic metabolite when alcohol is consumed. The opioid antagonist naltrexone (50 mg/day) is thought to reduce the self-reinforcing craving that occurs during active drinking by interfering with the neurotransmission of reward. Acamprosate (666 mg t.i.d.) appears to improve abstinence rates by reducing the craving that accompanies withdrawal (24) . A recent study demonstrated allelic variation of the μ-opioid receptor gene associated with differential response to naltrexone in alcohol-dependent individuals (25) . If replicated, this intriguing finding could help identify which individuals are most likely to respond to naltrexone treatment. Other predictors of medication response have not been identified. A depot formulation of naltrexone has demonstrated efficacy in decreasing alcohol consumption in alcohol-dependent individuals for periods of up to 1 month after a single injection (26) .
Because each of these agents has a different mechanism of action, theoretically they could be used concurrently to improve outcomes. However, a recent multisite investigation of naltrexone and acamprosate given individually and in combination did not demonstrate any benefit of combination therapy (27) . The use of these agents in co-occurring anxiety disorders, either in combination with SSRIs or alone, has not been systematically explored.
Summary and Recommendations
Ms. M presented with generalized anxiety, sleep disturbance, and concern about a pattern of increased alcohol consumption. Given the likelihood that her alcohol consumption was exacerbating her anxiety and sleep symptoms, her psychiatrist suggested eliminating the use of alcohol as the first step in treatment. Initially, Ms. M was not interested in working toward a goal of abstinence from alcohol, but after several failed attempts to cut down on alcohol use, she decided that abstinence was the best course of action. Pharmacologic options to support abstinence were discussed, and naltrexone (50 mg/day) was initiated. This resulted in a significant decrease in alcohol craving.
Ms. M’s anxiety in social situations continued to be problematic, making it difficult for her to engage the necessary social support for her recovery. In addition to cognitive behavior therapy targeting both alcohol relapse prevention and social anxiety, Ms. M was started on escitalopram (10 mg/day), and her social anxiety lessened. She joined a local AA group and was able to secure a sponsor who was also a nurse in recovery. The AA community has become an invaluable source of support and a significant part of her life.
1. Weisner C, Schmidt L: Gender disparities in treatment for alcohol problems. JAMA 1992; 268:1872–1876Google Scholar
2. Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG: AUDIT: The Alcohol Use Disorders Identification Test: Guidelines for Use in Primary Care, 2nd ed. Geneva, World Health Organization, Department of Mental Health and Substance Dependence, 2001Google Scholar
3. Fiellin DA, Reid MD, O’Connor PG: Screening for alcohol problems in primary care: a systematic review. Arch Intern Med 2000; 160:1977–1989Google Scholar
4. Saitz R: Clinical practice: unhealthy alcohol use. N Engl J Med 2005; 352:596–607Google Scholar
5. National Institute on Alcohol Abuse and Alcoholism: The Physicians’ Guide to Helping Patients With Alcohol Problems. NIH Publication No 95-3769. Rockville, Md, Department of Health and Human Services, 1995Google Scholar
6. Saladin ME, Santa Ana EJ: Controlled drinking: more than just a controversy. Curr Opin Psychiatry 2004; 17:175–187Google Scholar
7. Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, Pickering RP, Kaplan K: Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry 2004; 61:807–816Google Scholar
8. Kessler RC, Nelson CB, McGonagle KA, Edlund MJ, Frank RG, Leaf PJ: The epidemiology of co-occurring addictive and mental disorders: implications for prevention and service utilization. Am J Orthopsychiatry 1996; 66:17–31Google Scholar
9. Kushner MG, Sher KJ, Beitman BD: The relation between alcohol problems and the anxiety disorders. Am J Psychiatry 1990; 147:685–695Google Scholar
10. Piazza PV, Le Moal M: Stress as a factor in addiction, in Principles of Addiction Medicine. Edited by Graham AW, Schultz TK. Chevy Chase, Md, American Society of Addiction Medicine, 1998, pp 83–93Google Scholar
11. Nemeroff CB: The corticotropin-releasing factor (CRF) hypothesis of depression: new findings and new directions. Mol Psychiatry 1996; 1:336–342Google Scholar
12. Sinha R, Talih M, Malison R, Cooney N, Anderson GM, Kreek MJ: Hypothalamic-pituitary-adrenal axis and sympatho-adreno-medullary responses during stress-induced and drug cue-induced cocaine craving states. Psychopharmacology (Berl) 2003; 170:62–72Google Scholar
13. Brady KT, Back SE, Waldrop AE, McRae AL, Anton RF, Upadhyaya HP, Saladin ME, Randall PK: Cold pressor task reactivity: predictors of alcohol use among alcohol-dependent individuals with and without comorbid posttraumatic stress disorder. Alcohol Clin Exp Res 2006; 30:938–946Google Scholar
14. Project MATCH Research Group: Project MATCH secondary a priori hypotheses. Addiction 1997; 92:1671–1698Google Scholar
15. Otto MW, Smits JAJ, Reese HE: Combined psychotherapy and pharmacotherapy for mood and anxiety disorders in adults: review and analysis. Clin Psychol Sci Pract 2005; 12:72–86Google Scholar
16. Brady KT, Dansky BS, Back SE, Foa EB, Carroll KM: Exposure therapy in the treatment of PTSD among cocaine-dependent individuals: preliminary findings. J Subst Abuse Treat 2001; 21:47–54Google Scholar
17. Randall CL, Johnson MR, Thevos AK, Sonne SC, Thomas SE, Willard SL, Brady KT, Davidson JR: Paroxetine for social anxiety and alcohol use in dual-diagnosed patients. Depress Anxiety 2001; 14:255–262Google Scholar
18. Schade A, Marquenie LA, van Balkom AJ, Koeter MW, de Beurs E, van den Brink W, van Dyck R: The effectiveness of anxiety treatment on alcohol-dependent patients with a comorbid phobic disorder: a randomized controlled trial. Alcohol Clin Exp Res 2005; 29:794–800Google Scholar
19. Kranzler HR, Burleson JA, Del Boca FK, Babor TF, Korner P, Brown J, Bohn MJ: Buspirone treatment of anxious alcoholics: a placebo-controlled trial. Arch Gen Psychiatry 1994; 51:720–731Google Scholar
20. Pettinati HM, Volpicelli JR, Luck G, Kranzler HR, Rukstalis MR, Cnaan A: Double-blind clinical trial of sertraline treatment for alcohol dependence. J Clin Psychopharmacol 2001; 21:143–153Google Scholar
21. Kranzler HR, Burleson JA, Brown J, Babor TF: Fluoxetine treatment seems to reduce the beneficial effects of cognitive-behavioral therapy in type B alcoholics. Alcohol Clin Exp Res 1996; 20:1534–1541Google Scholar
22. Mayo-Smith MF: Pharmacological management of alcohol withdrawal: a meta-analysis and evidence-based practice guideline. JAMA 1997; 278:144–151Google Scholar
23. Anton RF, Swift RM: Current pharmacotherapies of alcoholism: a US perspective. Am J Addict 2003; 12(suppl 1):S53–S68Google Scholar
24. Mariani JJ, Levin FR: Pharmacotherapy for alcohol-related disorders: what clinicians should know. Harv Rev Psychiatry 2004; 12:351–366Google Scholar
25. Oslin DW, Berrettini W, Kranzler HR, Pettinati H, Gelernter J, Volpicelli JR, O’Brien CP: A functional polymorphism of the mu-opioid receptor gene is associated with naltrexone response in alcohol-dependent patients. Neuropsychopharmacology 2003; 28:1546–1552Google Scholar
26. Garbutt JC, West SL, Carey TS, Lohr KN, Crews FT: Pharmacological treatment of alcohol dependence: a review of the evidence. JAMA 1999; 281:1318–1325Google Scholar
27. Anton RF, O’Malley SS, Ciraulo DA, Cisler RA, Couper D, Donovan DM, Gastfriend DR, Hosking JD, Johnson BA, LoCastro JS, Longabaugh R, Mason BJ, Mattson ME, Miller WR, Pettinati HM, Randall CL, Swift R, Weiss RD, Williams LD, Zweben A; COMBINE Study Research Group: Combined pharmacotherapies and behavioral interventions for alcohol dependence: the COMBINE study: a randomized controlled trial. JAMA 2006; 295:2003–2017Google Scholar



