Trauma and Dissociation in China
Abstract
Objective: In order to determine whether pathological dissociation occurs in China, the authors conducted a survey among psychiatric inpatients, outpatients, and the general population in Shanghai, China. There is virtually no popular or professional knowledge of dissociative identity disorder in China, and therefore professional and popular contamination cannot exist. Method: Chinese versions of the Dissociative Experiences Scale and the Dissociative Disorders Interview Schedule were administered to 423 inpatients, 304 outpatients, and 618 factory workers in Shanghai by Chinese psychiatrists working at the Shanghai Mental Health Center. Results: Dissociative disorders were diagnosed in 24 respondents by structured interview, and 15 respondents fell into the dissociative taxon on the Dissociative Experiences Scale. The outpatients reported the highest rates of childhood physical and/or sexual abuse and of pathological dissociation. Conclusions: Pathological dissociation can be detected readily among psychiatric outpatients in China but is much less common in the general population. Pathological dissociation is more frequent in more traumatized subsamples of the Chinese population. The findings are not consistent with the sociocognitive, contamination, or iatrogenic models of dissociative identity disorder.
The epidemiology of dissociative disorders has been studied in the general population in Canada (1) and Turkey (2) , among college students in Canada (3) and the United States (4) , in chemically-dependent populations in Canada and the United States (5 – 8) , and among general adult psychiatric inpatients in Canada (9 , 10) , the United States (11 – 14) , Turkey (15) , Switzerland (16) , Norway (17) , the Netherlands (18) , and Germany (19) . A series of dissociative identity disorder cases has been described in other countries, including Australia (20) and Puerto Rico (21) . These studies have established that dissociative disorders are not rare, but controversy persists concerning whether they occur naturally or are primarily a response to cultural influences and role demands made by therapists (22 – 27) .
China is a country in which there is little public or cultural awareness of dissociative identity disorder or other forms of chronic, complex, pathological dissociation. We are not familiar with any representation of the disorder on television, in film, in novels or plays, or in popular folklore. The trauma model of dissociation is not taught at medical schools in China, and dissociative disorders are very rarely diagnosed by mental health professionals. China, therefore, is virtually free of cultural or professional contamination concerning dissociative disorders. These assertions concerning the absence of information on dissociation in China are based on the collective experience of the first seven authors of this study, all of whom are Chinese psychiatrists living in Shanghai and working at the study site, Shanghai Mental Health Center.
There are two competing models of pathological dissociation: the trauma model (28 – 30) and the sociocognitive model (22 – 27) . The trauma model makes three predictions concerning pathological dissociation: 1) pathological dissociation should occur in any culture in which there is chronic childhood trauma; 2) within any given culture, pathological dissociation should be more frequent among more traumatized subgroups; and 3) pathological dissociation is a psychological reaction to trauma.
According to the sociocognitive model, complex pathological trauma is an artifact of contamination, and trauma is not a relevant etiological variable. The sociocognitive model predicts that 1) pathological dissociation should be absent in any culture free of contamination and role demands for it to occur, and 2) in cultures where pathological dissociation does occur, it is caused by contamination and iatrogenesis, not by trauma. The two models differ on their theories of etiology, and they make distinct predictions concerning epidemiology.
We predicted that a structured interview for dissociative disorders and a self-report measure for dissociation would detect complex pathological dissociation in China. That is, we tested the first predictions of the trauma and sociocognitive models of dissociation. The methodology of our study did not allow a direct test of the traumatic etiology of any dissociation we detected; however, we predicted that higher levels of dissociation would be reported by more traumatized subgroups in Shanghai.
Method
Subjects
This study was approved by the ethics committee and administrators at Shanghai Mental Health Center. The respondents consisted of three groups: inpatients at Shanghai Mental Health Center (N=423), outpatients at Shanghai Mental Health Center (N=304), and a nonclinical sample of workers at a clothing manufacturing factory (N=618). The inpatients were interviewed during Dec. 1998, and they were selected from 950 inpatients screened during that month. Inclusion criteria for the inpatients were that they had to be positive for one of three of the following items: one or more Schneiderian first-rank symptoms of schizophrenia, childhood physical abuse, or childhood sexual abuse.
The outpatients were interviewed during March and April 2000. Every fifth person coming in for an appointment was screened with the same three inclusion criteria used for the inpatients until a total of 304 respondents were collected. Each day, the Shanghai Mental Health Center has between 500 and 800 outpatient appointments scheduled. The factory workers were interviewed in August and Sept. 2000. The manufacturing company provided a list of all employees, and every fifth person on the list was approached for an interview. There were less than five refusals. All the workers had agreed to participate prior to their first meeting with the interviewers, and all were given a small gift as a token of thanks for their participation.
Procedure
All interviews were conducted by a team of 12 psychiatrists. Rater training sessions were held prior to the beginning of data collection. The training consisted of a group discussion of the two measures and the meaning of all scale items and a session in which one person administered the structured interview while all the psychiatrists scored it independently. Further discussion was then undertaken to ensure that scoring decisions were consistent, but no statistical analysis of interrater reliability was conducted.
All subjects completed Chinese versions of the Dissociative Experiences Scale (29 , 31–35) and the Dissociative Disorders Interview Schedule (28 , 36–38) . The Dissociative Experiences Scale is a 28-item self-report measure used in over 250 published studies (39) . It has excellent reliability and concurrent validity with other measures of dissociation (38) . An eight-item subscale of the Dissociative Experiences Scale yields a conclusion of whether an individual is inside or outside of the dissociative taxon (34 , 35) . Members of the dissociative taxon report pathological experiences not endorsed by nontaxon members. These include experiences such as not recognizing oneself in a mirror and not recognizing family members. General population norms for the Dissociative Experiences Scale on a sample of 1,055 respondents in Winnipeg, Canada are also available (33) .
The Dissociative Disorders Interview Schedule is a structured diagnostic interview that determines DSM-IV diagnoses of somatization disorder, major depressive disorder, borderline personality disorder, and the five dissociative disorders. In addition, it asks questions about substance abuse, secondary features of dissociative identity disorder, extrasensory/paranormal experiences, and childhood physical and sexual abuse. The Dissociative Disorders Interview Schedule has established reliability and concurrent validity when compared to a clinical interview, the Structured Clinical Interview for DSM-IV Dissociative Disorders (40 – 44) , and the Dissociative Experiences Scale-T (34 , 35) . When respondents in a survey of general adult psychiatric inpatients were categorized as having no dissociative disorder, dissociative identity disorder, or dissociative disorder not otherwise specified, the Dissociative Disorders Interview Schedule has rates of agreement (using Cohen’s kappa) of 0.71 with clinician ratings, 0.74 with the Structured Clinical Interview for DSM-IV Dissociative Disorders, and 0.81 with the Dissociative Experiences Scale-T taxon membership. Interviewers in this study were blind to the results of all other measures.
Results
Demographics
There were significant differences among the inpatients, outpatients, and factory workers in terms of age (36.1 years [SD=8.9], 40.7 years [SD=7.0], and 41.7 years [SD=5.9], respectively; F=80.797, p<0.00001), percentage of women (44%, 41%, and 52%; F=6.329, p<0.002), number of children (mean= 0.3 [SD=0.5], 0.4 [SD=0.5], and 1.0 [SD=0.4]; F=351.199, p<0.00001), and percentage who were married (28%, 37%, and 92%; F=417.076, p<0.00001).
Childhood Trauma History
There were significant differences among the inpatients, outpatients, and factory workers in terms of the rate of childhood physical abuse (5.4% [N=23], 13.1% [N=40], and 0.1% [N=1], respectively; F=40.504, p<0.00001). While the groups did not differ in rate of childhood sexual abuse (2.8% [N=12], 3.0% [N=9], and 0.0% [N=0]), when the two forms of trauma were combined, a significant difference among the groups was found (7.8% [N=33], 14.5% [N=44], and 0.1% [N=1]; F=42.959, p<0.00001).
Diagnoses
There were no cases of somatization disorder. There were significant differences among the inpatients, outpatients, and factory workers in prevalence of the following disorders queried in the Dissociative Disorders Interview Schedule: substance abuse (2.8% [N=12], 2.0% [N=6], and 8.3% [N=51], respectively; F=11.76, p<0.00001), dissociative amnesia (0.2% [N=1], 1.3% [N=4], and 0.2% [N=1]; F=3.37, p<0.04), dissociative fugue (0.0%, 1.3% [N=4], and 0.0%; F=6.92, p<0.001), and a dissociative disorder of some type (1.7% [N=7], 5.0% [N=15], and 0.3% [N=2]; F=12.59, p<0.00001). Other disorders diagnosed among the inpatients, outpatients, and factory workers were major depressive episode (6.4% [N=27], 7.6% [N=23], and 2.6% [N=16]), borderline personality disorder (1.7% [N=7], 1.3% [N=4], and 0.3% [N=2]), depersonalization disorder (0.2% [N=1], 0.0%, and (0.2% [N=1]), dissociative identity disorder (0.5% [N=2], 0.3% [N=1], and 0.0%), and dissociative disorder not otherwise specified (0.7% [N=3], 2.0% [N=6], and 0.0%). Membership in the dissociative taxon on the Dissociative Experiences Scale-T was as follows: six inpatients (1.4%), six outpatients (2.0%), and three factory workers (0.5%), a nonsignificant difference.
Symptoms
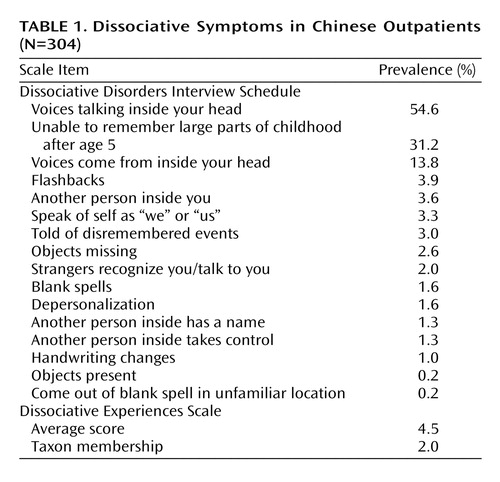
There were significant differences among the inpatients, outpatients, and factory workers on the following sections of the Dissociative Disorders Interview Schedule: somatization symptoms (1.2 [SD=2.0], 2.1 [SD=2.9], and 1.9 [SD=2.5], respectively; F=14.76, p<0.00001), positive substance abuse items (0.03 [SD=0.2], 0.02 [SD=0.2], and 0.08 [SD=0.3]; F=10.64, p<0.00001), Schneiderian symptoms (1.9 [SD=1.9], 2.8 [SD=2.3], and 0.01 [SD=0.2]; F=414.11, p<0.00001), secondary features of dissociative identity disorder (0.9 [SD=1.1], 1.3 [SD=1.2], and 0.5 [SD=0.7]; F=65.64, p<0.00001), borderline personality disorder criteria (0.4 [SD=1.0], 0.5 [SD=1.0], and 0.2 [SD=0.6]; F=19.71, p<0.00001), and extrasensory/paranormal experiences (0.5 [SD=1.3], 0.3 [SD=0.8], and 0.2 [SD=0.6]; F=12.54, p<0.00001). Symptoms of the outpatients are shown in Table 1 .
The average score on the Dissociative Experiences Scale was 4.1 (SD=7.5) for inpatients, 4.5 (SD=7.9) for outpatients, and 2.6 (SD=4.3) for factory workers, a significant difference (F=11.64, p<0.00001).
Discussion
The results of our study support the epidemiological prediction of the trauma model of dissociation and are not consistent with the sociocognitive model. Pathological dissociation was reported by Chinese respondents, despite the lack of contamination, role demands, and iatrogenic suggestion in China. Pooling the 1,345 Chinese respondents, a dissociative disorder of some type was diagnosed in 24 individuals by the Dissociative Disorders Interview Schedule, while 15 respondents were in the dissociative taxon on the Dissociative Experiences Scale. There were three individuals with dissociative identity disorder.
As shown in Table 1 , there are hints in the secondary features of dissociative identity disorder that full or partial forms of dissociative identity disorder could affect more than 2.3% of the Chinese outpatient sample (the sum of the frequencies of these two diagnoses on the Dissociative Disorders Interview Schedule). For instance, 3.6% of the Chinese outpatients said that they have another person inside of them.
The outpatients reported more childhood trauma than the other two groups. The outpatients had more dissociative disorders on the Dissociative Disorders Interview Schedule, more members of the dissociative taxon on the Dissociative Experiences Scale, higher average scores on the Dissociative Experiences Scale, and more secondary features of dissociative identity disorder on the Dissociative Disorders Interview Schedule. Thus, the outpatients were more dissociative than the other two groups on four different ways of assessing dissociation. The fact that they also reported more childhood abuse is consistent with the trauma model of pathological dissociation.
Our study has several strengths and limitations. All interviews were conducted by practicing psychiatrists; three separate samples of Chinese respondents were included; and the measures used have established reliability and validity (32 , 34 , 35 , 44) . China provides an example of a culture largely uncontaminated by popular or professional knowledge of dissociative identity disorder and therefore is suitable for testing the epidemiological predictions of the trauma and sociocognitive models.
The limitations of this study include the fact that all respondents were from one Chinese city, and therefore the results may not be generalizable to China as a whole. This limitation does not affect the test of the study’s primary hypothesis, however. There may have been unrecognized problems with the translations of the Dissociative Experiences Scale and Dissociative Disorders Interview Schedule that affected the validity of the findings. In addition, the meaning of some responses may have been misunderstood because of unrecognized cultural factors. These two possible limitations are tempered by the fact that the interviews were conducted by Chinese psychiatrists practicing in Shanghai.
1. Ross CA: Epidemiology of multiple personality and dissociation. Psychiatr Clin N Am 1991; 14:503–517Google Scholar
2. Akyuz G, Dogan O, Sar V, Yargic LI, Tutkun H: Frequency of dissociative identity disorder in the general population in Turkey. Compr Psychiatry 1999; 40:151–159Google Scholar
3. Ross CA, Ryan L, Voigt H, Edie L: High and low dissociators in a college student population. Dissociation 1991; 4:147–151Google Scholar
4. Murphy PE: Dissociative experiences and disorders in a non-clinical university group. Dissociation 1994; 7:28–34Google Scholar
5. Ross CA, Kronson J, Koensgen S, Barkman K, Clark P, Rockman G: Dissociative comorbidity in 100 chemically dependent patients. Hosp Community Psychiatry 1992; 43:840–842Google Scholar
6. Ellason JW, Ross CA, Sainton K, Mayran LW: Axis I and II comorbidity and childhood trauma history in chemical dependency. Bull Menninger Clin 1996; 60:39–51Google Scholar
7. Dunn GE, Paolo AM, Ryan JJ, Van Fleet JN: Dissociative symptoms in a substance abuse population. Am J Psychiatry 1993; 150:1043–1047Google Scholar
8. Leeper DH, Page B, Hendricks DE: The prevalence of dissociative disorders in a drug and alcohol abusing population of a residential treatment facility in a military medical center. Unpublished manuscriptGoogle Scholar
9. Ross CA, Anderson G, Fleisher WP, Norton GR: The frequency of multiple personality disorder among psychiatric inpatients. Am J Psychiatry 1991; 148:1717–1720Google Scholar
10. Horen SA, Leichner PP, Lawson JS: Prevalence of dissociative symptoms and disorders in an adult psychiatric inpatient population in Canada. Can J Psychiatry 1995; 40:185–191Google Scholar
11. Ross CA, Duffy CMM, Ellason JW: Prevalence, reliability and validity of dissociative disorders in an inpatient setting. J Trauma Dissoc 2002; 3:7–17Google Scholar
12. Latz TT, Kramer SI, Hughes DL: Multiple personality disorder among female inpatients in a state hospital. Am J Psychiatry 1995; 152:1343–1348Google Scholar
13. Saxe GN, van der Kolk BA, Berkowitz R, Chinman G, Hall K, Lieberg G, Schwartz J: Dissociative disorders in psychiatric inpatients. Am J Psychiatry 1993; 150:1037–1042Google Scholar
14. Rifkin A, Ghisalbert D, Dimatou S, Jin C, Sethi M: Dissociative identity disorder in psychiatric inpatients. Am J Psychiatry 1998; 155:844–855Google Scholar
15. Tutkun H, Sar V, Yargic LI, Ozpulat T, Yanik M, Kiziltan E: Frequency of dissociative disorders among psychiatric inpatients in a Turkish university clinic. Am J Psychiatry 1998; 155:800–805Google Scholar
16. Modestin J: Multiple personality disorder in Switzerland. Am J Psychiatry 1992; 149:88–92Google Scholar
17. Knudsen H, Draijer N, Haselrud J, Boe T, Boon S: Dissociative disorders in Norwegian psychiatric inpatients, in Proceedings of the Spring Meeting of the International Society for the Study of Dissociation, Amsterdam, ISSD, 1995Google Scholar
18. Friedl MC, Draijer N: Dissociative disorders in a Dutch psychiatric inpatient population. Am J Psychiatry 2000; 157:1012–1013Google Scholar
19. Gast U, Rodewald F, Nickel V, Emrich HM: Prevalence of dissociative disorders among psychiatric inpatients in a German university clinic. J Nerv Ment Dis 2001; 189:249–257Google Scholar
20. Middleton W, Butler J: Dissociative identity disorder: an Australian series. Aust NZ J Psychiatry 1998; 32:794–804Google Scholar
21. Martinez-Taboas A: Multiple personality disorder in Puerto Rico: analysis of fifteen cases. Dissociation 1989; 2:128–131Google Scholar
22. Spanos N: Multiple Identities and False Memories: A Sociocognitive Perspective. Washington, DC, American Psychological Association, 1996Google Scholar
23. Lilienfeld SO, Lynn SJ, Kirsch I, Chaves JF, Sarbin TR, Ganaway GK, Powell RA: Dissociative identity disorder and the sociocognitive model: recalling the lessons of the past. Psychol Bull 1999; 125:507–523Google Scholar
24. Piper A: Hoax and Reality: The Bizarre World of Multiple Personality Disorder. Northvale, NJ, Jason Aronson, 1997Google Scholar
25. Pope HG, Oliva PS, Hudson JI, Bodkin JA, Gruber AJ: Attitudes toward DSM-IV-TR dissociative disorder diagnoses among board-certified American psychiatrists. Am J Psychiatry 1999; 156:321–332Google Scholar
26. Merskey H: The manufacture of personalities: the production of multiple personality disorder, in Dissociative Identity Disorder: Theoretical and Treatment Controversies. Cohen L, Berzoff J, Elin M. Northvale, NJ (eds.). Jason Aronson, 1995Google Scholar
27. Simpson M: Gullible’s travels, or the importance of being multiple. Ibid, pp 87–134Google Scholar
28. Putnam FW: Diagnosis and Treatment of Multiple Personality Disorder. New York, Guilford, 1989Google Scholar
29. Ross CA: Dissociative Identity Disorder: Diagnosis, Clinical Features, and Treatment of Multiple Personality (2nd edition). New York, John Wiley & Sons, 1997Google Scholar
30. Ross CA: The Trauma Model: A Solution to the Problem of Comorbidity in Psychiatry. Richardson, Tex, Manitou Communications, 2000Google Scholar
31. Bernstein EM, Putnam FW: Development, reliability, and validity of a dissociation scale. J Nerv Ment Dis 1986; 174:727–735Google Scholar
32. Carlson EB, Putnam FW, Ross CA, Torem M, Coons P, Bowman ES, Chu J, Dill DL, Loewenstein RJ, Braun BG: Predictive validity of the Dissociative Experiences Scale. Am J Psychiatry 1993; 150:1030–1036Google Scholar
33. Ross CA, Joshi S: Dissociative experiences in the general population. Am J Psychiatry 1992; 147:1547–1552Google Scholar
34. Waller NG, Putnam FW, Carlson EB: The types of dissociation and dissociative types: a taxometric analysis of dissociative experiences. Psychol Methods 1996; 1:300–321Google Scholar
35. Waller NG, Ross CA: The prevalence and biometric structure of pathological dissociation in the general population: taxometric structure and behavior genetic findings. J Abnorm Soc Psychol 1997; 106:499–510Google Scholar
36. Ross CA, Heber S, Norton GR, Anderson G, Anderson G, Barchet P: The Dissociative Disorders Interview Schedule: a structured interview. Dissociation 1989; 2:169–189Google Scholar
37. Ross CA, Miller SD, Reagor P, Bjornson L, Fraser GA, Anderson G: Structured interview data on 102 cases of multiple personality disorder from four centers. Am J Psychiatry 1990; 147:596–601Google Scholar
38. Ellason JW, Ross CA: Two-year follow-up of inpatients with dissociative identity disorder. Am J Psychiatry 1997; 154:832–839Google Scholar
39. Dell PF: Dissociative phenomenology of dissociative identity disorder. J Nerv Ment Dis 2002; 190:10–15Google Scholar
40. Steinberg M: Handbook for the Assessment of Dissociation: A Clinical Guide. Washington, DC, American Psychiatric Press, 1995Google Scholar
41. Steinberg M, Cicchetti D, Buchanan J, Rakfeldt J, Rounsaville B: Distinguishing between multiple personality disorder (dissociative identity disorder) and schizophrenia using the Structured Clinical Interview for DSM-IV Dissociative Disorders. J Nerv Ment Dis 1994; 182:495–502Google Scholar
42. Steinberg M, Rounsaville BJ, Cicchetti DV: The Structured Clinical Interview for DSM-III-R Dissociative Disorders: preliminary report on a new diagnostic instrument. Am J Psychiatry 1990; 147:76–82Google Scholar
43. Ross CA, Joshi S: Schneiderian symptoms and childhood trauma in the general population. Compr Psychiatry 1992; 33:269–273Google Scholar
44. Pincus HA, Rush JA, First MB, McQueen LE: Handbook of Psychiatric Measures. Arlington, Va, American Psychiatric Publishing, 2000Google Scholar
45. Kleinman A, Kleinman J: Somatization: the interconnections in Chinese society among culture, depressive experiences, and the meanings of pain, in Culture and Depression: Studies in Anthropology and Cultural Psychiatry of Affect and Disorder. Edited by Kleinman A, Good B. Berkeley, University of California Press, 1985, pp 429–490Google Scholar