Descriptive and Longitudinal Observations on the Relationship of Borderline Personality Disorder and Bipolar Disorder
Abstract
Objective: The purpose of this study was to test whether borderline personality disorder is a variant of bipolar disorder by examining the rates of co-occurrence in both disorders, the effects of co-occurrence on a longitudinal course, and whether the presence of either disorder confers the risk for new onsets of the other. Method: A prospective repeated-measures design with reliable independent diagnostic measures and 4 years of follow-up was used to assess 196 patients with borderline personality disorder and 433 patients with other personality disorders. Results: Patients with borderline personality disorder had a significantly higher co-occurrence of bipolar disorder (19.4%) than did patients with other personality disorders. However, this co-occurrence did not appear to affect the subsequent course of borderline personality disorder. Although only 8.2% of the borderline personality disorder patients developed new onsets of bipolar disorder, this rate was higher than in patients with other personality disorders. Patients with other personality disorders with co-occurring bipolar disorder generally had more new onsets of borderline personality disorder (25%) than did patients with other personality disorders without co-occurring bipolar disorder (10%). Conclusions: A modest association between borderline personality disorder and bipolar disorder is reported.
Advocates for an expanded bipolar disorder construct (i.e., a “bipolar spectrum”) believe that the affective lability and impulsive behaviors characteristic of patients with borderline personality disorder derive from shared genes and that borderline personality disorder should be reconceptualized and reclassified as a part of the bipolar spectrum (1 – 3) . This thesis is timely as psychiatry strives to develop a nosology in which disorders are grouped into spectrums on the basis of shared etiology (4 – 6) . It is also appealing because it encourages an optimistic view that patients with borderline personality disorder might benefit from the extensive research on bipolar disorder and that these patients might also prove to be responsive to mood stabilizing medications. Still, as reviewed elsewhere, only a modest body of methodologically sound research to date addresses the interface of borderline personality disorder and bipolar disorders, and of this research, very little supports the thesis of a spectrum relationship between the two disorders (7) .
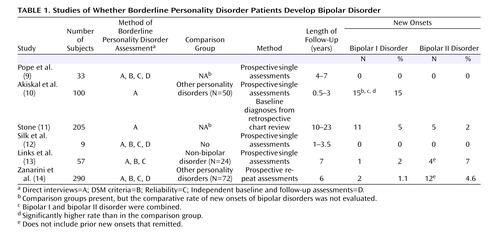
Using data from the Collaborative Longitudinal Personality Disorders Study, we address the interface of borderline personality disorder and bipolar disorder, particularly whether borderline personality disorder evolves into bipolar disorder (8) . Table 1 summarizes six prior longitudinal investigations of whether borderline personality disorder becomes bipolar disorder (9 – 14) . The study conducted by Akiskal and colleagues (10) is notable in that the highest rates of new onsets (i.e., 15%) within 3 years are reported, and their study is the only one to date in which the rate of new onsets was higher than in the comparison group. The two studies with the strongest methodologies (i.e., diagnostic assessments, sample size, length of follow-up) showed fewer new onsets (i.e., 5.7%–9%) and reported no difference from the comparison groups (13 , 14) .
Our study uses a prospective repeated-measures design, reliable and independent diagnostic assessments, 4 years of follow-up, and a comparison group with other personality disorders. This data set was established to determine the following: 1) whether co-occurring bipolar disorder is more common in borderline personality disorder than other personality disorders; 2) whether co-occurring bipolar disorder affects the demographics, comorbidity, treatment utilization, and course of borderline personality disorder; 3) whether borderline personality disorder patients are more apt to develop bipolar disorder; 4) whether new onsets of bipolar disorder occur as an evolution of borderline psychopathology or as sequelae to either neurobiological changes or life event stressors; and 5) whether co-occurring bipolar disorder confers increased risk for developing new onsets of borderline personality disorder.
Method
Detailed descriptions of the Collaborative Longitudinal Personality Disorders Study project have been reported separately (8 , 15) . All participants gave informed consent before entering the study.
Participants
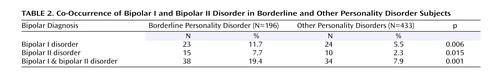
Participants in this study included 629 treatment-seeking patients for whom follow-up data were collected for 4 years (at 6, 12, 24, 36, and 48 months). Patients were excluded if they had been diagnosed with schizophrenia or schizoaffective disorder or if they had current problems with substance abuse in which intoxication or withdrawal could confound assessments. For the purpose of this study, patients were divided into the following two groups: those diagnosed with borderline personality disorder (N=196) and a comparison group of those diagnosed with other personality disorders (i.e., schizotypal personality disorder, avoidant personality disorder, and obsessive-compulsive disorder) (N=433) ( Table 2 ). Patients in both the borderline personality disorder group and the other personality disorders group were between the ages of 18–45 and represented the full range of socioeconomic classes. To examine the relationship of bipolar disorder to borderline personality disorder, we divided the borderline personality disorder group on the basis of presence (N=38) or absence (N=158) of lifetime co-occurring bipolar I or bipolar II disorder. As a comparison group, the patients with other personality disorders were likewise divided on the basis of presence (N=34) or absence (N=399) of lifetime co-occurring bipolar I or bipolar II disorder. To assess whether co-occurring bipolar disorder increased risks for new onsets of borderline personality disorder, we only examined patients with other personality disorders who had three or less borderline personality disorder criteria at baseline (N=299), thereby requiring an incremental increase of at least two borderline personality disorder criteria in order to justify being labeled a “new onset.”
Assessments
All patients were evaluated at baseline using the Diagnostic Interview for DSM-IV Personality Disorders (16) and the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I) (17) . Evaluations were conducted by clinically experienced interviewers trained to distinguish axis I mental-state conditions from axis II personality-trait phenomena. For the 10 axis I disorders where adequate Ns existed, the interrater reliability median was 0.76, and the test-retest kappa median was 0.64 (18) . For bipolar disorder, interrater reliabilities had a median kappa of 0.74. For borderline personality disorder, the interrater and test-retest kappas were 0.68 and 0.69, respectively. The patients were evaluated again at 6, 12, 24, 36, and 48 months, with a prospective version of the Diagnostic Interview for DSM-IV Personality Disorders that records monthly variations in borderline criteria. Retrospective reliability for borderline personality disorder was good (kappa = 0.70). Longitudinal reliability between original raters and subsequent raters was also tested. Correlations between new raters for the number of criteria (mean=0.75–0.92) and correlation of new raters with the original raters (mean=0.75–0.94) were similar. Thus, prospective reliability was good, and rater drift was minimal (19) .
Prospective assessments of bipolar disorder were evaluated using psychiatric status ratings of the Longitudinal Interval Follow-Up Evaluation (20) , which records weekly variations in major depressive, manic, and hypomanic DSM-IV criteria. New onsets of bipolar I disorder were defined as either 1 week or more of mania in a patient with no prior manic or hypomanic episodes. New onsets of bipolar II disorder were defined as 1 week or more of hypomania and 2 weeks or more of depression in a patient with no prior hypomanic episodes. To examine stability, remission was operationally defined as 2 consecutive months, with two or fewer criteria for both borderline personality disorder and bipolar disorder. This definition, as used in other Collaborative Longitudinal Personality Disorders Study reports (19) , is a widely used precedent in studies of major depressive disorder and other axis I disorders (21 , 22) . This definition of remission is arbitrary with respect to personality disorders, but it was used in our study to assure that most aspects of borderline psychopathology were absent—rather than merely having subthreshold or temporary lulls in criteria.
The following are three possible precipitants for new onsets of bipolar disorder, which were assessed using relevant data from the preceding 4 months: 1) borderline personality disorder evolves into bipolar disorder (monthly DIPD-prospective version ratings were used to determine whether changes in the number of borderline personality disorder criteria precede onsets); 2) neurobiological changes (weekly Longitudinal Interval Follow-Up Evaluation-based ratings were used to rate whether significant changes in psychoactive medication usage or in substance use/misuse had occurred); and 3) stressful life events (both the Longitudinal Interval Follow-Up Evaluation narrative accounts and the Life Events Assessment (23) identified whether significant life events had occurred). Four authors (J.G.G., M.D., K.D.K., I.W.) independently rated whether the relevant data documented the presence of these three precipitants as definite=2, possible=1, or no=0. The level of agreement for borderline personality disorder criteria changes was kappa=0.82. The level of agreement for neurobiological changes was kappa=0.64, and the level for life events was kappa=0.71.
Analyses
We used chi-square analyses to examine whether the prevalence of bipolar disorder was more common in the borderline personality disorder group than in the other personality disorders group. We used chi-square analyses or analyses of variance (ANOVA) to compare baseline differences in the 164 borderline personality disorder patients without bipolar disorder to our target group of the 23 borderline personality disorder patients with co-occurring bipolar I disorder and the 15 with co-occurring bipolar II disorder according to the following conditions: borderline personality disorder criteria; global assessment of functioning; comorbidity of major depressive disorder, alcohol/substance abuse/dependence, or posttraumatic stress disorder (PTSD); number of psychiatric hospitalizations; and types of prescribed psychotropic medications (i.e., lithium, selective serotonin reuptake inhibitors [SSRIs], other antidepressants, neuroleptics, anticonvulsants). Because of the number of comparisons between groups, Bonferroni corrections were used. This meant that statistical significance was reached at p<0.006 for borderline personality disorder criteria and p<0.007 for medication types.
For the patients with and without bipolar disorder, comparative rates of remission of borderline personality disorder were analyzed using Kaplan-Meier survival methods. Repeated-measures ANOVA was used to examine how co-occurring bipolar disorder affected the course of the global assessment of functioning of the borderline personality disorder patients and the number of weeks of their hospitalization. Generalized estimating equations (24) were used to examine whether co-occurring bipolar disorder affected rates of medication usage across the 4 years. The generalized estimating equations models included a linear-time term to test for an increase or decrease in the use of each medication over time. Chi-square analyses were used to compare the rates of new onsets of bipolar disorder, borderline personality disorder, and other personality disorders and to compare the rates of new onsets of borderline personality disorder in other personality disorders patients with and without bipolar disorder.
Results
As shown in Table 2 , bipolar I disorder and bipolar II disorder were significantly more common in patients with borderline personality disorder than in patients with other personality disorders. Comorbid bipolar I or bipolar II disorder occurred in 19.4% of borderline personality disorder patients, versus 7.9% of patients with other personality disorders (χ 2 =17.71, df=1, p<0.001). Bipolar I disorder alone was more common in patients with borderline personality disorder (χ 2 =7.48, df=1, p<0.006) than bipolar II disorder (χ 2 =10.09, df=1, p<0.015).
The presence of comorbid bipolar I or bipolar II disorder had no significant effect on baseline rates of number and types of borderline personality disorder criteria, demographic data, global assessment of functioning, comorbidity, or history of psychiatric hospitalizations. The only significant differences were that patients with comorbid bipolar disorder had, as expected, histories of more use of lithium (32% versus 6.7%, χ 2 =13.36, df=1, Fisher’s exact [two-sided] p<0.0014) and more anticonvulsants (50% versus 17.8%, χ 2 =11.59, df=1, Fisher’s exact [two-sided] p<0.0007). Because of the limited number of bipolar patients, however, only large differences could be detected reliably.
Next, we examined whether the co-occurrence of bipolar I or bipolar II disorder at baseline affected the course of borderline personality disorder. Of the 31 patients with borderline personality disorder with co-occurring bipolar disorder, 66% (N=19) achieved remission by 4 years, which was the same as the 65% (N=89 of 141) for patients with borderline personality disorder without bipolar disorder (Wilcoxon χ 2 =0.0011, df=1, p<0.885). With respect to whether co-occurring bipolar I or bipolar II disorder affected global assessment of functioning scores, we found that global assessment of functioning scores improved over the course of 4 years for patients with borderline personality disorder with or without bipolar disorder. Repeated-measures ANOVA showed no difference by group (Wilk’s lambda F value=0.96, df=4, 138, p<0.44). Repeated-measures ANOVA also showed that co-occurring bipolar disorder had no effect on the number of hospitalizations (Wilk’s lambda F=0.03, df=2, 10, p<0.97). Generalized estimating equations, controlling for baseline usage, showed that co-occurring bipolar I or bipolar II disorder had no significant effect on use of SSRIs (χ 2 =1.28, df=1, p<0.26), other antidepressants (χ 2 =0.01, df=1, p<0.91), neuroleptics (χ 2 =0.66, df=1, p<0.42), or anticonvulsants (χ 2 =0.68, df=1, p<0.41) over the 4 years. The limited use of lithium made this analysis unfeasible.
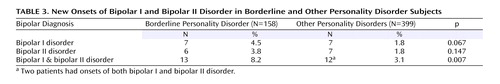
As shown in Table 3 , patients with borderline personality disorder without lifetime bipolar disorder had seven (4.5%) new onsets of bipolar I disorder during the 4-year period. This was a higher rate, although not significantly, than the seven (1.8%) new onsets found in patients with other personality disorders without bipolar (χ 2 =3.36, df=1, p<0.07). The borderline personality disorder patients had six (3.8%) new onsets of bipolar II disorder, which was not significantly higher than the 1.8% rate (N=7 of 399) of bipolar II disorder new onsets in patients with other personality disorders (χ 2 =2.11, df=1, p<0.15). The combined rate of new onsets for bipolar I and bipolar II disorder in the borderline personality disorder group (N=13 of 158, 7.9%) was significantly higher than the 3.1% rate in the other personality disorders group (χ 2 = 7.29, df=1, p<0.007). Of the new onsets, 10 of 13 (77%) for either bipolar I or bipolar II disorder occurred in patients with borderline personality disorder with current or lifetime major depressive disorder at baseline, versus 12 of 14 (86%) in patients with other personality disorders (χ 2 =3.15, df=1, p<0.77). (These respective percentages are somewhat higher than the overall lifetime rate of major depressive disorder in our borderline personality disorder group [60%] or other personality disorders group [59%].)
We examined whether the new onsets of bipolar disorder were preceded by changes in borderline psychopathology, neurobiology, or life events. Our ratings indicated that in no instance did these new onsets follow borderline personality disorder criteria change (either increase or decrease). Six new bipolar onsets followed significant stressful life events; two followed significant neurobiological changes; one followed both stressful life events and neurobiological change; and no precipitants were observed in three.
To examine whether the presence of bipolar I disorder or bipolar II disorder conferred a risk for development of borderline personality disorder, we compared the 277 patients with other personality disorders without comorbid bipolar disorder to the 22 patients with bipolar disorders. The rates of new borderline personality disorder onsets were generally higher in patients with other personality disorder with co-occurring bipolar disorder (i.e., 23%, N=5) than in patients with other personality disorders without co-occurring bipolar disorder (i.e., 10%, N=28) (χ 2 =3.31, df=1, p=0.07).
Discussion
Although our study provides significant improvements in design and methodology, the results should still be interpreted with some degree of caution. For example, although the rate of co-occurrence of bipolar and borderline disorder observed (i.e., the lifetime rates at baseline and new onsets combined brought lifetime co-occurrence to 27.6%) seems high enough to suggest a significant relationship, this may not be the case. Analyses of co-occurrence rates from multiple other studies show that the rate of borderline personality disorder comorbidity in bipolar patients is not higher than for patients with other personality disorders (7) . Moreover, the rate of bipolar co-occurrence in our borderline personality disorder group is modest compared to the rates found for other disorders (even before following for new onsets). For example, in borderline personality disorder patients, the rates of co-occurrence for major depressive disorder, substance abuse, and PTSD were all more than twice the rate we found for bipolar I and bipolar II disorder (25 , 26) . Finally, because rates of co-occurrence are always elevated in clinical samples, good epidemiological data on the co-occurrence rates of these two disorders in healthy populations are needed before a relationship can be inferred. The validity of diagnosing new bipolar episodes, especially bipolar II disorder, when they are derived retrospectively in follow-up interviews is also problematic (27 , 28) . Thus, this study can offer the reassuring facts that our interviewers were clinically experienced, and they used standardized interviews on which they were well trained and recurrently retrained to avoid rater drift. Moreover, they had no preconceptions or hypotheses that might have biased their efforts to document the manic episodes. These state-of-the-art methods do not prevent mistakes, but they are safeguards against systematic or idiosyncratic bias. A third limitation worthy of comment is the composition of personality disorders in our comparison group (i.e., obsessive-compulsive disorder, schizotypal disorder, and avoidant disorder) that might be expected to have less overlap with the affective and impulsive traits of bipolar disorder and borderline personality disorder than would other personality disorders such as antisocial and histrionic personality disorders. Had these latter two disorders been assessed, they might have shed more light on whether borderline personality disorder has a spectrum relationship with bipolar disorder.
The presence of a co-occurring bipolar disorder had no appreciable clinical significance on the clinical course of borderline personality disorder—not in remission rates, functional adjustment, or in treatment utilization as measured by rates of hospitalization and medication usage. The failure of comorbid bipolar disorder to be associated with an altered rate of borderline personality disorder remissions echoes an earlier finding in which major depressive disorder showed only a weak association with borderline personality disorder remissions at 2 years (29) and none at 3 years (30) . These results suggest that borderline personality disorder and bipolar disorder are not strongly associated disorders.
Our study also shows, however, that patients with borderline personality disorder are significantly more apt to have comorbid bipolar I or bipolar II disorder than patients with other personality disorders and are more apt to have new onsets of bipolar I or bipolar II disorder (when combined, i.e., 7.9%). This rate (i.e., 7.9%) is similar to the rates found by Links and colleagues (13) and Zanarini and colleagues (14) , and while it is approximately one-half of the rate of onsets found by Akiskal (31) , like Akiskal, it was significantly higher than the comparison group. These findings support the concept of a modest association between borderline personality disorder and bipolar disorder. This modest association is also supported by our finding that patients with other personality disorders with co-occurring bipolar disorder showed more new onsets of borderline personality disorder. Still, given the other results in our study and those of other investigators (7 , 32) , the modest association that has been observed between borderline personality disorder and bipolar disorder is not yet conclusive. Clearly, the new onsets of bipolar disorder did not represent an evolution from borderline personality disorder psychopathology; rather, they most often followed stressful neurobiological or life changes. It remains to be determined whether a neurobiological disposition toward onsets of bipolar episodes was created due to the fact that our borderline personality disorder patients received far more medications than our patients with other personality disorders (33 , 34) .
In summary, our report on the longitudinal course of borderline personality disorder demonstrates a modest association with bipolar disorder. Nonetheless, the evidence in this study for only a small association of borderline personality disorder with bipolar disorder reinforces other results (29 , 30 , 35 , 36) that have documented a noncyclical, good prognosis course for borderline personality disorder, thereby making a strong spectrum relationship with bipolar disorder extremely unlikely.
Clinical Implications
Despite the fact that these disorders only co-occur in 10%–25% of patients with either disorder (7) , it has become unusual for patients with borderline personality disorder not to have been diagnosed with bipolar disorder, usually bipolar II disorder. The absence of a strong association between borderline personality disorder and bipolar disorder, suggested in this study, indicates that clinicians should attend to the differences. Sustained periods of elation, mood lability without evident stressors, or any period of true mania make borderline personality disorder unlikely or secondary. Periods of depression and irritability are rarely instructive. Repeated angry outbursts, suicide attempts, or acts of deliberate self-harm that are reactive to interpersonal stress and reflect extreme rejection sensitivity are axiomatic of borderline personality disorder. In the presence of these symptoms, the diagnosis of a bipolar disorder is unlikely or secondary.
Identifying the co-occurrence of borderline personality and bipolar disorders may be helpful, but the current widespread practice of diagnosing a patient with bipolar disorder and omitting the borderline personality disorder diagnosis has two damaging effects. The bipolar diagnosis encourages patients and their families to have unrealistic expectations about what medications can do. The real—albeit modest—benefits that usually occur when borderline personality disorder is present are then experienced as a failure, which leads to polypharmacy and a growing sense of despair. Moreover, omitting the borderline personality disorder diagnosis diverts therapeutic efforts away from psychosocial interventions that can often make a remarkable difference. Clinicians are frequently reluctant to give patients a diagnosis of borderline personality disorder because it is viewed negatively and is treated most effectively when specialized services that may not qualify for full reimbursement are used. In fact, however, a diagnosis of borderline personality disorder offers patients a reasonable hope for a future that will not require ongoing mental health intervention.
1. Akiskal HS: The bipolar spectrum—the shaping of a new paradigm in psychiatry. Curr Psychiatry Rep 2002; 4:1–3Google Scholar
2. Perugi G, Akiskal HS: The soft bipolar spectrum redefined: focus on the cyclothymic, anxious-sensitive, impulse-dyscontrol, and binge-eating connection in bipolar II and related conditions. Psychiatr Clin North Am 2002; 25:713–737Google Scholar
3. Akiskal HS: Demystifying borderline personality: critique of the concept and unorthodox reflections on its natural kinship with the bipolar spectrum. Acta Psychiatr Scand 2004; 110:401–407Google Scholar
4. Hudson JI, Pope HG: The concept of affective spectrum disorder: relationship to fibromyalgia and other syndromes of chronic fatigue and chronic muscle pain. Baillieres Clin Rheumatol 1994; 8:839–856Google Scholar
5. Hollander E, Kwon JH, Stein DJ, Broatch J, Rowland CT, Himelein CA: Obsessive-compulsive and spectrum disorders: overview and quality of life issues. J Clin Psychiatry 1996; 57(suppl 8):3–6Google Scholar
6. Kupfer DJ, Frank E, Grochocinski VJ, Cluss PA, Houck PR, Stapf DA: Demographic and clinical characteristics of individuals in a bipolar disorder case registry. J Clin Psychiatry 2002; 63:120–125Google Scholar
7. Paris J, Gunderson JG, Weinberg I: The interface between borderline personality disorder and bipolar spectrum disorders, Proceedings from the McLean Hospital Conference on Borderline Personality Disorder: New Acceptance and Heightened Optimism. Boston, McLean Hospital, 2003Google Scholar
8. Gunderson JG, Shea MT, Skodol EA, McGlashan TH, Morey LC, Stout RI, Zanarini MC, Grilo CM, Oldham JM, Keller MB: The Collaborative Longitudinal Personality Disorders Study I: development, aims, design, and sample characteristics. J Personal Disord 2000; 14:300–315Google Scholar
9. Pope HG Jr, Jonas JM, Hudson JI, Cohen BM, Gunderson JG: The validity of DSM–III borderline personality disorder: a phenomenologic, family history, treatment response, and long-term follow-up study. Arch Gen Psychiatry 1983; 40:23–30Google Scholar
10. Akiskal HS, Chen SE, Davis GC, Puzantian VR, Kashgarian M, Bolinger JM: Borderline: an adjective in search of a noun. J Clin Psychiatry 1985; 46:41–48Google Scholar
11. Stone MH: The Fate of Borderline Patients. New York, Guilford, 1990Google Scholar
12. Silk KR, Westen D, Lohr NE, Benjamin J, Gold L: DSM–III and DSM–III–R schizotypal symptoms in borderline personality disorder. Compr Psychiatry 1990; 31:103–110Google Scholar
13. Links PS, Heslegrave RJ, Mitton JE, Van Reekum R, Patrick J: Borderline psychopathology and recurrences of clinical disorders. J Nerv Ment Dis 1995; 83:582–586Google Scholar
14. Zanarini MC, Frankenburg FR, Hennen J, Reich DB, Silk KR: Axis I comorbidity in patients with borderline personality disorder: 6-year follow-up and prediction of time to remission. Am J Psychiatry 2004; 161:2108–2114Google Scholar
15. McGlashan TH, Grilo CM, Skodol AE, Gunderson JG, Shea MT, Morey LC, Zanarini MC, Stout RI: The Collaborative Longitudinal Personality Disorders Study: baseline axis I/II and II/II diagnostic co-occurrence. Acta Psychiatr Scand 2000; 102:256–264Google Scholar
16. Zanarini MC, Shea MT; The Diagnostic Interview for DSM–IV Personality Disorders—Follow-along Version (DIPD-IV-FA). Belmont, McLean Hospital 1996Google Scholar
17. First MB, Spitzer RL, Gibbon M, William JBW: Structured Clinical Interview for DSM–IV Axis I Disorders/Patient Edition (SCID-I/P). New York, New York State Psychiatric Institute, Biometrics Research Department, 1996Google Scholar
18. Zanarini MC, Skodol AE, Bender D, Dolan R, Sanislow C, Schaefer E, Morey LC, Grilo CM, Shea MT, McGlashan TH, Gunderson JG: The Collaborative Longitudinal Personality Disorders Study: reliability of axis I and II diagnoses. J Personal Disord 2000; 14:291–299Google Scholar
19. Skodol AE, Gunderson JG, Shea MT, McGlashan TH, Morey LC, Sanislow CA, Bender DS, Grilo CM, Zanarini MC, Yen S, Pagano ME, Stout RI: The Collaborative Longitudinal Personality Disorders Study (CLPS): overview and implications. J Personal Disord 2005; 19:487–504Google Scholar
20. Keller MB, Lavori PW, Friedman B, Nielsen E, Endicott J, McDonald-Scott P, Andreasen NC: The Longitudinal Interval Follow-Up Evaluation: a comprehensive method for assessing outcome in prospective longitudinal studies. Arch Gen Psychiatry 1987; 44:540–548Google Scholar
21. Keller MB, Shapiro RW, Lavori PW, Wolfe N: Recovery in major depressive disorder: analysis with the life table and regression models. Arch Gen Psychiatry 1982; 39:905–910Google Scholar
22. Stout RL, Dolan R, Dyck I, Eisen J, Keller MB: Course of social functioning after remission from panic disorder. Compr Psychiatry 2001; 42:441–447Google Scholar
23. Holmes TH, Rahe RH: The Social Readjustment Rating Scale. J Psychosom Res 1967; 11:213–218Google Scholar
24. Diggle PJ, Liang K: Analysis of Longitudinal Data. Oxford, Oxford University Press, 1994Google Scholar
25. McGlashan TH, Grilo CM, Skodol AE, Gunderson JG, Shea MT, Morey LC, Zanarini MC, Stout RI: The Collaborative Longitudinal Personality Disorders Study: baseline axis I/II and II/II diagnostic co-occurrence. Acta Psychiatrica Scand 2000; 102:256–264Google Scholar
26. Zanarini MC, Frankenburg FR, Hennen J, Reich DB, Silk KR: Axis I comorbidity in patients with borderline personality disorder: 6-year follow-up and prediction of time to remission. Am J Psychiatry 2004; 161:2108–2114Google Scholar
27. Akiskal HS: The prevalent clinical spectrum of bipolar disorders: beyond. DSM–IV: J Clin Psychopharmacol 1996; 16:4–14Google Scholar
28. Dunner DI, Tay KL: Diagnostic reliability of the history of hypomania in bipolar II patients and patients with major depression. Compr Psychiatry 1993; 34:303–307Google Scholar
29. Shea MT, Stout RL, Yen S, Pagano ME, Skodol AE, Morey LC, Gunderson JG, McGlashan TH, Grilo CM, Sanislow CA, Bender DS, Zanarini MC: Associations in the course of personality disorders and axis I disorders over time. J Abnorm Psychol 2004; 113:499–508Google Scholar
30. Gunderson JG, Morey LC, Stout RL, Skodol AE, Shea MT, McGlashan TH, Zanarini MC, Grilo CM, Sanislow CA, Yen S, Daversa MT, Bender DS: Major depressive disorder and borderline personality disorder revisited: longitudinal interactions. J Clin Psychiatry 2004; 65:1049–1056Google Scholar
31. Akiskal HS: Borderline: an adjective still in search of a noun, in Handbook of Borderline Disorders. Edited by Silver D, Rosenbluth M. Madison, International Universities Press, 1992, pp 155–177Google Scholar
32. White CN, Gunderson JG, Zanarini MC, Hudson JI: Family studies of borderline personality disorder: a review. Harv Rev Psychiatry 2003; 11:8–19Google Scholar
33. Bender DS, Dolan RT, Skodol AE, Sanislow CA, Dyck IR, McGlashan TH, Shea MT, Zanarini MC, Oldham JM, Gunderson JG: Treatment utilization by patients with personality disorders. Am J Psychiatry 2001; 158:295–302Google Scholar
34. Bender DS, Skodol AE, Pagano ME, Dyck IR, Grilo CM, Shea MT, Sanislow CA, Zanarini MC, Yen S, McGlashan TH, Gunderson JG: Prospective treatment utilization by patients with personality disorders. Psychiatr Serv 2006; 57:254–257Google Scholar
35. Grilo CM, Shea MT, Sanislow CA, Skodol AE, Gunderson JG, Stout RL, Pagano ME, Yen S, Morey LC, Zanarini MC, McGlashan TH: Two-year stability and change in schizotypal, borderline, avoidant and obsessive-compulsive personality disorders. J Consult Clin Psychol 2004; 72:767–775Google Scholar
36. Zanarini MC, Frankenburg FR, Hennen J, Silk KR: The longitudinal course of borderline psychopathology: 6-year prospective follow-up of the phenomenology of borderline personality disorder. Am J Psychiatry 2003; 160:274–283Google Scholar