Prevalence of Dissociative Disorders in Psychiatric Outpatients
Abstract
Objective: The purpose of the study was to assess the prevalence of DSM-IV dissociative disorders in an inner-city outpatient psychiatric population. Method: Subjects were 231 consecutive admissions (84 men and 147 women, mean age=37 years) to an inner-city, hospital-based outpatient psychiatric clinic. The subjects completed self-report measures of dissociation (Dissociative Experiences Scale) and trauma history (Traumatic Experiences Questionnaire). Eighty-two patients (35%) completed a structured interview for dissociative disorders (Dissociative Disorders Interview Schedule). Results: The 82 patients who were interviewed did not differ significantly on any demographic measure or on the self-report measures of trauma and dissociation from the 149 patients who were not interviewed. Twenty-four (29%) of the 82 interviewed patients received a diagnosis of a dissociative disorder. Dissociative identity disorder was diagnosed in five (6%) patients. Compared to the patients without a dissociative disorder diagnosis, patients with a dissociative disorder were significantly more likely to report childhood physical abuse (71% versus 27%) and childhood sexual abuse (74% versus 29%), but the two groups did not differ significantly on any demographic measure, including gender. Chart review revealed that only four (5%) patients in whom a dissociative disorder was identified during the study had previously received a dissociative disorder diagnosis. Conclusions: Dissociative disorders were highly prevalent in this clinical population and typically had not been previously diagnosed clinically. The high prevalence of dissociative disorders found in this study may be related to methodological factors (all patients were offered an interview rather than only those who had scored high on a screening self-report measure) and epidemiological factors (extremely high prevalence rates for childhood physical and sexual abuse were present in the overall study population).
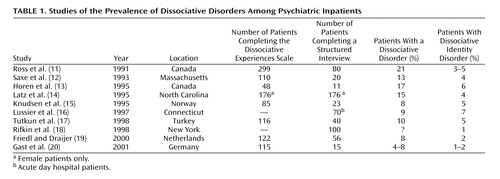
Dissociative disorders, including dissociative identity disorder (formerly multiple personality disorder), were once thought to be exotic and rare disorders, if indeed they existed at all (1) . Several epidemiological studies over the past 15 years have shown that dissociative disorders may have been previously underdiagnosed and that with proper screening and diagnostic instrumentation, a much higher prevalence is encountered. Several studies have assessed the prevalence of dissociative experiences and/or dissociative disorders in community samples around the world (2 – 6) and in various special populations (e.g., substance abusers or survivors of childhood sexual abuse) (7 – 10) . To date, inpatient populations have been studied most thoroughly (11 – 20) ( Table 1 ). In most of these studies, a dissociative disorder had been correctly diagnosed in only a small percentage of the patients before their inclusion in the study. Given that the population receiving outpatient psychiatric treatment is much larger than the psychiatric inpatient population, it is plausible that many patients with dissociative pathological features are receiving outpatient treatment without the benefit of a correct diagnosis. However, outpatient populations have not been studied in sufficient detail to address this question.
The prevalence of dissociative disorders in psychiatric outpatient populations has been examined in two previous studies, but these studies had significant methodological weaknesses, including lack of standardized diagnostic measures and skewed samples drawn from settings specializing in the treatment of dissociative disorders (21 , 22) . In the only methodologically strong outpatient study to date, Sar et al. (23) found that 12% of Turkish outpatients could qualify for a diagnosis of a dissociative disorder, including 4% with dissociative identity disorder and 8% with dissociative disorder not otherwise specified. Only 1% of those patients had been given a dissociative disorder diagnosis before entering the study.
Sar et al. used a methodological approach common to the large majority of prevalence studies to date. This approach involves first screening the population with a self-report measure of dissociation (the Dissociative Experiences Scale, described in the Method section) and then administering diagnostic interviews only to patients who score above a given cutoff point, as high scorers are more likely to carry a dissociative diagnosis. Dissociative Experiences Scale cutoff scores of 15, 20, 25, and 30 have been suggested by various authors (24 – 27) . Latz et al. (14) conducted one of the few studies in which a cutoff score was not used. They administered a structured interview for dissociative disorders (the Dissociative Disorders Interview Schedule, described in the Method section) to every patient in their study and found that the Dissociative Experiences Scale scores of the patients who were found to have a dissociative disorder according to the interview overlapped extensively with the Dissociative Experiences Scale scores of the patients without a dissociative disorder diagnosis according to the interview. Their data indicated that a substantial number of patients with dissociative disorders would have been missed if the Dissociative Experiences Scale screening method had been used.
To our knowledge, the present study is the first assessment of dissociative disorders among U.S. psychiatric outpatients in which standardized diagnostic instruments were used and the first outpatient study in which an attempt was made to interview all eligible patients, without the use of a screening instrument, in order to capture the prevalence of dissociative disorders as accurately as possible. The study subjects consisted of all patients consecutively admitted to an inner-city, hospital-based psychiatric outpatient clinic. Based on extensive experience working with this particular clinic population, as well as the results of previous studies in which the Dissociative Experiences Scale was administered in the same clinic (28 , 29) , we predicted that diagnostic interviews would reveal a prevalence of dissociative disorders of more than 20% and that chart review would reveal that these disorders had been diagnosed clinically in less than 5% of the patients.
Method
Subjects
All English-speaking adult patients, ages 18 to 65 years, who enrolled for treatment at the Montefiore Medical Center’s Psychiatric Outpatient Department (Bronx, N.Y.) between August 1996 and March 1998 were eligible for the study (N=231). Patients who were unable to speak English could not be interviewed and thus were excluded from the study; there were no other exclusion criteria. As part of the clinic’s routine admission procedure, patients filled out several self-report and demographic measures at the time of making application for treatment. The measures included the Dissociative Experiences Scale and the Traumatic Experiences Questionnaire (described in the next section); the patient’s responses to these self-report measures became part of the patient’s clinical record. After applying for treatment, patients were scheduled for an intake appointment within 1–4 weeks. Within 6 weeks of this initial intake appointment, we attempted to contact all patients and invited them to participate in a 45–90-minute interview in which the Dissociative Disorders Interview Schedule (described in the next section) was used. Each patient was paid $20 for participating in the study. Of 231 patients, 82 (35%) were contacted and interviewed. Reasons for not being interviewed included having no phone or being otherwise unable to be contacted (N=78), declining to be interviewed (N=52), or failing to appear for a scheduled interview (N=19). There were no patients who began the interview and failed to complete it. All of the patients who were interviewed provided written informed consent at the time of the interview, after the interview procedure had been explained. The informed consent form, as well as the overall study design, received the approval of the institutional review boards of Montefiore Medical Center and of the Albert Einstein College of Medicine.
The structured clinical interviews were performed by three raters, including the senior author (B.F.) and two advanced-degree clinicians who were trained in the use of the instrument by the senior author in a 20-hour training program in which videotapes and practice interviews were used. Videotapes of 10 study subjects were rated by the interviewers to assess interrater reliability. Interrater reliability was excellent (kappa=0.95, N=55, p<0.0001) among the three raters. The interviewers were blind to patients’ self-report and clinical data.
Instruments
Dissociative Experiences Scale
The Dissociative Experiences Scale is a widely used 28-item self-report measure for assessment of specific dissociative experiences (30 , 31) . In a 1996 meta-analysis, the Dissociative Experiences Scale was found to have a test-retest reliability of 0.78–0.93 (six studies), an internal reliability (alpha) of 0.93 (16 studies), and a convergent validity (r) of 0.67 (26 studies) (32) .
Traumatic Experiences Questionnaire
The Traumatic Experiences Questionnaire is a 49-item self-report measure used for assessing detailed, specific experiences in four domains: childhood physical abuse, childhood sexual abuse, witnessing of domestic violence, and adult retraumatization (28) . A validation study comparing self-report answers on the Traumatic Experiences Questionnaire to information obtained in a face-to-face interview indicated high rates of agreement in a subset of 50 subjects (kappa=0.83) (33) . For our study, one of the authors (B.F.) constructed a scale to convert the self-reports of childhood sexual and physical abuse into three continuous quantitative variables. Severity of abuse was assigned a rating from 0 to 3, which was multiplied by a duration rating from 0 to 3. Points were then added for aggravating factors (such as the presence of multiple perpetrators) to yield a score from 0 to 10 for childhood physical abuse and from 0 to 10 for childhood sexual abuse. These scores were added to yield a score from 0 to 20 for total childhood abuse. Thus, numerical scores derived from the Traumatic Experiences Questionnaire data are reported for childhood physical abuse, childhood sexual abuse, and total childhood abuse.
Dissociative Disorders Interview Schedule
The Dissociative Disorders Interview Schedule is a 131-item structured interview used to assess DSM-IV diagnoses of somatization disorder, major depression, borderline personality disorder, alcohol and drug abuse, and the five DSM-IV dissociative disorders (34) . It is also used to inquire about a wide range of other experiences, including trauma history, and about features thought to be associated with dissociative identity disorder, such as Schneiderian symptoms. It has been found to have good interrater reliability (kappa=0.68) and a false positive rate of less than 1% for the diagnosis of dissociative identity disorder. With our population, we repeatedly had the impression that the Dissociative Disorders Interview Schedule questions (in which the DSM-IV diagnostic criteria are essentially incorporated verbatim) were poorly understood by our patients. To compensate for possible misunderstanding, we first asked each Dissociative Disorders Interview Schedule question exactly as worded, and then if the interviewer felt the patient might not have understood the question, the interviewer was permitted to ask the question again, with explanations as necessary. This procedure yielded two diagnostic impressions: a strict Dissociative Disorders Interview Schedule rating and a clinical impression. If either diagnostic impression was negative, the diagnosis was scored as negative.
Data Collection
Data on the presence or absence of childhood physical abuse and childhood sexual abuse were collected from two different sources. One hundred seventy-eight patients completed the Traumatic Experiences Questionnaire and Dissociative Experiences Scale. For these patients, we report data on dissociative symptoms, the presence or absence of self-reported childhood physical abuse and childhood sexual abuse as measured by the Traumatic Experiences Questionnaire, and the quantification of childhood physical abuse and childhood sexual abuse from 0 to 10 as described earlier. For the 82 patients who participated in structured face-to-face interviews with the Dissociative Disorders Interview Schedule, we also report data on childhood physical and sexual abuse from this measure.
Because the outpatient clinic where this study was conducted is not widely known for the treatment of dissociative disorders, specialized referrals were not expected to be a significant source of bias. Nevertheless, the small number of patients (N=2) who had been referred specifically because of a possible dissociative disorder diagnosis during the study period were excluded from the data set.
Statistical Analysis
Subject characteristics measured as continuous variables were compared between groups by using Student’s t tests. Chi-square tests or Fisher’s exact tests were used to analyze categorical data. A logistic regression analysis model was used to assess the predictive value of a history of childhood abuse for a dissociative disorder diagnosis. All tests were two-tailed, and p values <0.05 were considered statistically significant. Data are expressed as means and standard deviations. Analyses were performed by using SPSS 11.0 (SPSS Inc., Chicago). Post hoc Bonferroni corrections were used to correct for multiple comparisons.
Results
Two hundred thirty-one English-speaking patients consecutively applied for treatment in the outpatient clinic during the study period. For the demographic characteristics summarized here, total Ns ranged from 203 to 231. This population was composed of predominantly minority (50% [N=107 of 216] Hispanic, 23% [N=50 of 216] African American, 20% [N=43 of 216] white), female (64%, N=147 of 231), poorly educated (38% [N=81 of 215] without high school degree), Medicaid insured (96%, N=194 of 203), and nonworking (82% [N=174 of 212] unemployed) patients, with a mean age of 37.4 years (SD=11.4). The distribution of primary axis I diagnoses included primarily depressive disorders (46%, N=104 of 228), psychotic disorders (15%, N=34 of 228), anxiety disorders (8%, N=17 of 228), and bipolar disorders (7%, N=15 of 228), with all other diagnoses each accounting for 2% or less of the patients (including PTSD in 2% [N=5 of 228] and dissociative disorders in 0.4% [N=1 of 228]). Of these patients, 82 completed the Dissociative Disorders Interview Schedule. These 82 patients were compared with the 149 noncompleters and did not differ significantly on any demographic measure, including age (t=–1.16, df=229, p=0.25), gender (χ 2 =0.003, df=1, p=0.96), ethnicity (χ 2 =1.91, df=3, p=0.59), educational level (χ 2 =0.23, df=2, p=0.99), and income, measured by Medicaid status (χ 2 =0.53, df=1, p=0.82). The two groups also showed no significant difference on measures of childhood sexual abuse, expressed by Traumatic Experiences Questionnaire score (t=–0.57, df=176, p=0.57), childhood physical abuse (t=–0.76, df=176, p=0.45), or dissociation (t=0.23, df=176, p=0.82). Extremely high levels of trauma and dissociation were found in both groups. The overall group of 231 subjects had a 59% prevalence of self-reported childhood physical abuse (N=103 of 175), a 34% prevalence of self-reported childhood sexual abuse (N=58 of 168), and a mean Dissociative Experiences Scale score of 20.9 (SD=18.7).
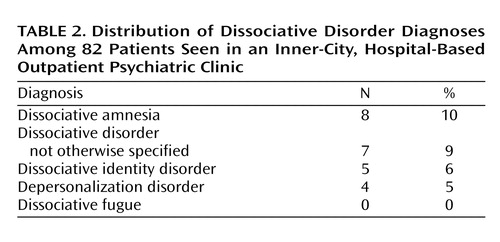
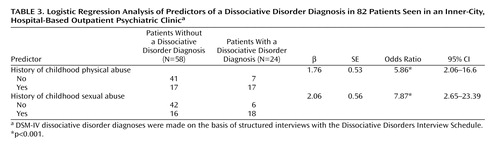
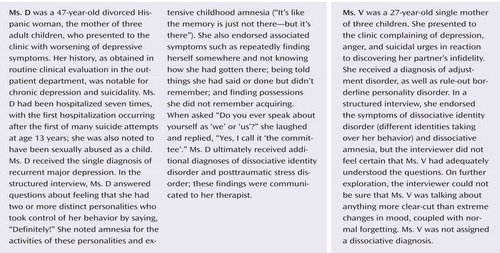
Twenty-four (29%) of the 82 patients (95% confidence interval [CI]=19.4%–39.0%) who were interviewed met the criteria for a DSM-IV dissociative disorder diagnosis, with the diagnoses distributed as follows: dissociative amnesia, N=8 (10%); dissociative disorder not otherwise specified, N=7 (9%); dissociative identity disorder, N=5 (6%); and depersonalization disorder, N=4 (5%) ( Table 2 ). None of the patients had a diagnosis of dissociative fugue. Only four (5%) of the 82 patients had a dissociative diagnosis recorded in their clinical charts. Compared with the 58 interviewees who did not meet the criteria for a dissociative disorder, the 24 patients who met the criteria did not differ on any demographic measure, including age (t=–1.13, df=80, p=0.26), gender (χ 2 =0.16, df=1, p=0.69), ethnicity (χ 2 =0.93, df=3, p=0.82), educational level (χ 2 =0.26, df=2, p=0.88), and income (χ 2 =1.38, df=1, p=0.27). However, the two groups differed significantly, as would be predicted, on measures of childhood trauma and of dissociation. Logistic regression analysis indicated that the patients who met the criteria for a dissociative disorder diagnosis were much more likely to have reported childhood physical abuse (odds ratio=5.86, 95% CI=2.06–16.67, p<0.001) and much more likely to have reported childhood sexual abuse (odds ratio=7.88, 95% CI=2.65–23.39, p<0.001) ( Table 3 ). The histories of the patients who met the dissociative disorder criteria were also marked by significantly more prolonged and more severe childhood physical abuse and childhood sexual abuse, compared with the patients who did not meet the dissociative disorder criteria. For childhood physical abuse, the mean Traumatic Experiences Questionnaire score of the patients who met the dissociative disorder criteria was 5.1 (SD=3.3), compared to 2.8 (SD=2.9) for those who did not meet the criteria (t=15.22, df=80, p<0.001). For childhood sexual abuse, the mean Traumatic Experiences Questionnaire score of the patients who met the dissociative disorder criteria was 3.7 (SD=4.0), compared with 1.0 (SD=2.1) for those who did not meet the criteria (t=9.88, df=80, p<0.002). As would be expected, the patients who received a dissociative disorder diagnosis also scored higher on the self-report measure of dissociative experiences (Dissociative Experiences Scale) (t=16.59, df=80, p<0.001).
Discussion
These results confirmed both the high prevalence and the extensive underdiagnosis of dissociative disorders in an outpatient psychiatric population. The 29% prevalence of dissociative disorders in this population was surprisingly high, as the bulk of past data would lead us to expect that the prevalence of dissociative disorders, as well as prevalence of trauma history, would increase in a stratified fashion from community samples to outpatient populations to inpatient populations; yet the prevalence we found in this outpatient population was higher than that found in previous studies of inpatients.
Two explanations are suggested. First, in most past studies, the Dissociative Experiences Scale was used as a screening instrument, and only subjects with a high score on the screen (or only those with very high or very low scores) were interviewed. In our study, as in the study by Latz et al. (14) , the Dissociative Experiences Scale scores of patients who ultimately received a dissociative disorder diagnosis displayed a wide range. Specifically, if we had used a Dissociative Experiences Scale score of 30 as a cutoff, 46% of the positive diagnoses we identified would have been missed; use of a more inclusive cutoff score of 20 still would have resulted in elimination of 25% of the dissociative disorder diagnoses. Thus the method of offering an interview to every patient, although more onerous, may prove to yield more accurate, higher prevalence rates.
Second, we must note the extremely high prevalence of childhood trauma and of dissociative symptoms in this poor inner-city population. By our presumably most accurate trauma assessment measure—the face-to-face interview—this population had a prevalence of childhood physical abuse of 40% and a prevalence of childhood sexual abuse of 42%. The mean Dissociative Experiences Scale score for the entire sample was 20.9, which is higher than the score suggested by some authors as a cutoff for screening. The values for prevalence of trauma and the mean Dissociative Experiences Scale scores reported for the inpatient populations studied to date ranged from somewhat lower to much lower than those of the subjects in our study. Given the widely recognized connection between trauma and dissociation (35 – 39) , it is not surprising that the outpatients in our study had a higher prevalence of dissociative disorders than the inpatient populations studied to date. A high prevalence of traumatic experiences, sometimes reflected in high Dissociative Experiences Scale scores, has been reported previously in poor inner-city populations (29 , 40) .
It is interesting to note that the prevalence of dissociative identity disorder in this population (6%) was not strikingly higher than that found in previous inpatient studies, whereas the overall rate of dissociative disorders (29%) was much higher. Reexamination of the inpatient studies revealed the tendency to diagnose a preponderance of dissociative identity disorder and dissociative identity disorder not otherwise specified, and very few cases of the “minor” dissociative disorders (dissociative amnesia and depersonalization). This finding is surprising given that the interviewers in all of these studies used either the same diagnostic instrument that was used in the current study (the Dissociative Disorders Interview Schedule) or the Structured Clinical Interview for DSM-IV Dissociative Disorders (SCID-D) (41) . Both of these instruments allow detailed inquiry about symptoms of all of the dissociative disorders and can be used to diagnose dissociative amnesia and depersonalization. In the current study, 50% of the diagnoses were from these “minor” categories. A hypothesis that was examined retrospectively in light of these data was that the higher prevalence of the minor disorders was a result of the methodological choice not to use a Dissociative Experiences Scale screen, i.e., patients with dissociative amnesia and depersonalization may score lower on the Dissociative Experiences Scale than those with dissociative identity disorder and dissociative identity disorder not otherwise specified and may therefore be selectively omitted when a Dissociative Experiences Scale screen is used. This hypothesis is consistent with the results of recent studies of depersonalization, in which mean Dissociative Experiences Scale scores in the low 20s were found for these patients (42 , 43) , and with the findings of numerous studies showing that patients with dissociative identity disorder and dissociative identity disorder not otherwise specified typically score in the 30s and 40s (31) . We reexamined the Dissociative Experiences Scale scores of the patients in each diagnostic category and did not find any support for this hypothesis, however. The subjects with dissociative identity disorder and dissociative identity disorder not otherwise specified in this study did not have significantly higher Dissociative Experiences Scale scores than the subjects with dissociative amnesia and depersonalization.
Our findings add to the growing amount of data concerning both the association between childhood trauma and adult dissociative psychopathology and the surprisingly high prevalence of dissociative disorders in clinical populations, with most of those disorders being previously undiagnosed. Our study had several limitations. First, we examined a specific largely Hispanic inner-city population, and prevalence in other outpatient populations could be different. Although the Dissociative Experiences Scale has been translated into Spanish and is widely used, we did not have the resources to conduct diagnostic interviews in Spanish, so data concerning a large subset (16%) of the population treated could not be used. Also, only 35% of the consecutively admitted patients could be interviewed, largely because of logistical factors. Although no differences were found on demographic measures or measures of trauma or dissociation between the interviewed patients and those not interviewed, this low percentage is still a possible source of error. Follow-up is inherently more difficult with outpatient populations, compared to inpatient populations, but participation in future studies could be improved by offering a larger financial incentive or by using a better method of tracking and contacting the patients other than trying to contact them by phone at home. It is worth noting, however, that even if none of the noninterviewed patients had a dissociative diagnosis, the frequency of dissociative disorders in the overall group nonetheless would have exceeded 10%—still a sizable number.
In addition, although we tried to improve on the diagnostic accuracy of the structured interview by giving the interviewer the option to ask clarifying questions after finishing the structured interview, this method is still not the same as the commonly accepted “gold standard” for ascertainment of a dissociative diagnosis, which is the administration of a structured interview (Dissociative Disorders Interview Schedule or SCID-D) followed by an open-ended clinical interview administered by an experienced diagnostician with expertise in dissociative disorders. A clinician using the most conservative diagnostic standard would need to witness alter personality states in the interview before making a definitive diagnosis of dissociative identity disorder. Also, in the assessment of trauma history, it should be noted that self-report of past traumatic experiences is subject to distortion and misremembering. Finally, this study focused solely on specific acts of childhood physical abuse and sexual abuse; we did not measure other childhood trauma, such as emotional abuse or neglect, or adult traumatic experiences, which have been shown to influence adult psychiatric and dissociative symptoms (44 – 47) .
However, we believe that this study is the first methodologically sound large-sample survey of dissociative disorders in a U.S. outpatient population and that our findings are a robust demonstration of the extremely high prevalence of these disorders, especially in a poor inner-city population. Patients with dissociative disorders are notoriously difficult to treat; this difficulty is of course greatly amplified when the condition goes undiagnosed. Because no definitive pharmacological treatments are available for dissociative disorders and because most other comorbid conditions are treated pharmacologically, the dissociative symptoms of patients with undiagnosed dissociative disorders remain untreated and perhaps may be masked or even worsened by the medications given, even as the patients are deprived of appropriate psychotherapy. This study, like many others, highlights the importance of developing better methods of screening for these disorders, with the hope of delivering more effective and better targeted care. Our findings suggest that the prevalence of dissociative disorders in poor inner-city populations may be even greater than previously suspected and point to the need for further studies to assess the magnitude of this problem.
1. Putnam F: Diagnosis and Treatment of Multiple Personality Disorder. New York, Guilford, 1989Google Scholar
2. Ross C: Epidemiology of multiple personality disorder and dissociation. Psychiatr Clin North Am 1991; 14:503–517Google Scholar
3. Vanderlinden J, Van Dyck R, Vandereycken W, Vertommen T: Dissociative experiences in the general population in the Netherlands and Belgium: a study with the Dissociative Questionnaire (DIS-Q). Dissociation 1991; 4:180–184Google Scholar
4. Vanderlinden J, Varga K, Peuskens J, Pieters G: Dissociative symptoms in a population sample of Hungary. Dissociation 1995; 8:205–208Google Scholar
5. Akyuz G, Dogan O, Sar V, Yargic LI: Frequency of dissociative identity disorder in the general population in Turkey. Compr Psychiatry 1999; 40:151–159Google Scholar
6. Murphy PE: Dissociative experiences and dissociative disorders in a non-clinical university student group. Dissociation 1994; 7:28–34Google Scholar
7. Ross CA, Kronson J, Koensgen S, Barkman K, Clark P, Rockman G: Dissociative comorbidity in 100 chemically dependent patients. Hosp Community Psychiatry 1992; 43:840–842Google Scholar
8. Anderson G, Yasenik L, Ross CA: Dissociative experiences and disorders among women who identify themselves as sexual abuse survivors. Child Abuse Negl 1993; 17:677–686Google Scholar
9. Dunn GE, Ryan JJ, Paolo AM, Van Fleet JN: Comorbidity of dissociative disorders among patients with substance use disorders. Psychiatr Serv 1995; 46:153–156Google Scholar
10. Carrion VG, Steiner H: Trauma and dissociation in delinquent adolescents. J Am Acad Child Adolesc Psychiatry 2000; 39:353–359Google Scholar
11. Ross CA, Anderson G, Fleisher WP, Norton GR: The frequency of multiple personality disorder among psychiatric inpatients. Am J Psychiatry 1991; 148:1717–1720Google Scholar
12. Saxe GN, van der Kolk BA, Berkowitz R, Chinman G, Hall K, Lieberg G, Schwartz J: Dissociative disorders in psychiatric inpatients. Am J Psychiatry 1993; 150:1037–1042Google Scholar
13. Horen SA, Leichner PP, Lawson JS: Prevalence of dissociative symptoms and disorders in an adult psychiatric inpatient population in Canada. Can J Psychiatry 1995; 40:185–191Google Scholar
14. Latz TT, Kramer SI, Hughes DL: Multiple personality disorder among female inpatients in a state hospital. Am J Psychiatry 1995; 152:1343–1348Google Scholar
15. Knudsen H, Draijer N, Haslerud J, Boe T, Boon S: Prevalence of dissociative disorders in a Norwegian general psychiatric department (inpatients and daycare), in Proceedings of the Fifth Annual Spring Conference of the International Society for the Study of Dissociation. Edited by van der Hart O, Boon S, Draijer N. Amsterdam, International Society for the Study of Dissociation, 1995, p 79Google Scholar
16. Lussier RG, Steiner J, Grey A, Hansen C: Prevalence of dissociative disorders in an acute care day hospital population. Psychiatr Serv 1997; 48:244–246Google Scholar
17. Tutkun H, Sar V, Yargic LI, Ozpulat T, Yanik M, Kiziltan E: Frequency of dissociative disorders among psychiatric inpatients in a Turkish university clinic. Am J Psychiatry 1998; 155:800–805Google Scholar
18. Rifkin A, Ghisalbert DO, Dimatou S, Jin C, Sethi M: Dissociative identity disorder in psychiatric inpatients. Am J Psychiatry 1998; 155:844–845Google Scholar
19. Friedl MC, Draijer N: Dissociative disorders in Dutch psychiatric inpatients. Am J Psychiatry 2000; 157:1012–1013Google Scholar
20. Gast U, Rodewald F, Nickel V, Emrich HM: Prevalence of dissociative disorders among psychiatric inpatients in a German university clinic. J Nerv Ment Dis 2001; 189:249–257Google Scholar
21. Bliss EL, Jeppsen EA: Prevalence of multiple personality among inpatients and outpatients. Am J Psychiatry 1985; 142:250–251Google Scholar
22. Graves SM: Dissociative disorders and dissociative symptoms at a community mental health center. Dissociation 1989; 2:119–127Google Scholar
23. Sar V, Tutkun H, Alyanak B, Bakim B, Baral IM: Frequency of dissociative disorders among psychiatric outpatients in Turkey. Compr Psychiatry 2000; 41:216–222Google Scholar
24. Steinberg M, Rounsaville B, Cicchetti D: Detection of dissociative disorders in psychiatric patients by a screening instrument and a structured interview. Am J Psychiatry 1991; 148:1050–1054Google Scholar
25. Chu, JA, Dill LD: Dissociative symptoms in relation to childhood physical and sexual abuse. Am J Psychiatry 1990; 147:887–892Google Scholar
26. Draijer N, Boon S: The validation of the Dissociative Experiences Scale against the criterion of the SCID-D using receiver operating characteristics (ROC) analysis. Dissociation 1993; 6:28–37Google Scholar
27. Carlson EB, Putnam FW, Ross CA, Torem M, Coons P, Dill DL, Loewenstein RJ, Braun BG: Validity of the Dissociative Experiences Scale in screening for multiple personality disorder: a multicenter study. Am J Psychiatry 1993; 150:1030–1036Google Scholar
28. Kaplan ML, Asnis GM, Lipschitz DS, Chorney P: Suicidal behavior and abuse in psychiatric outpatients. Compr Psychiatry 1995; 36:229–235Google Scholar
29. Kaplan ML, Erensaft M, Sanderson W, Wetzler S, Foote B, Asnis GM: Dissociative symptomatology and aggressive behavior. Compr Psychiatry 1998; 39:271–276Google Scholar
30. Bernstein EM, Putnam FW: Development, reliability, and validity of a dissociation scale. J Nerv Ment Dis 1986; 174:727–735Google Scholar
31. Carlson EB, Putnam FW: An update on the dissociative experiences scale. Dissociation 1993; 6:16–27Google Scholar
32. van Ijzendoorn MH, Schuengel C: The measurement of dissociation in normal and clinical populations: meta-analytic validation of the Dissociative Experiences Scale (DES). Clin Psychol Rev 1996; 16:365–382Google Scholar
33. Lipschitz DS, Kaplan ML, Sorkenn J, Chorney P, Asnis GM: Childhood abuse, adult assault, and dissociation. Compr Psychiatry 1996; 37:261–266Google Scholar
34. Ross CA, Heber S, Norton GR, Anderson D, Anderson G, Barchet P: The Dissociative Disorders Interview Schedule: a structured interview. Dissociation 1989; 2:169–189Google Scholar
35. Putnam FW: Dissociation as a response to extreme trauma, in Childhood Antecedents of Multiple Personality. Edited by Kluft RP. Washington, DC, American Psychiatric Press, 1985, pp 66–97Google Scholar
36. Spiegel D, Cardena E: Disintegrated experience: the dissociative disorders revisited. J Abnorm Psychol 1991; 100:366–378Google Scholar
37. Krystal JH, Bennett A, Bremner JD: Toward a cognitive neuroscience of dissociation and altered memory functions in post-traumatic stress disorder, in Neurobiological and Clinical Consequences of Stress: From Normal Adaptation to Post-Traumatic Stress Disorder. Edited by Friedman MJ, Charney DS, Deutch AY. Philadelphia, Lippincott-Raven, 1995, pp 239–270Google Scholar
38. Yehuda R, Elkin A, Binder-Brynes K, Kahana B, Southwick SM, Schmeidler J, Giller EL: Dissociation in aging Holocaust survivors. Am J Psychiatry 1996; 153:935–940Google Scholar
39. Spiegel D, Hunt T, Dondershine HE: Dissociation and hypnotizability in posttraumatic stress disorder. Am J Psychiatry 1988; 145:301–305Google Scholar
40. Lipschitz DS, Winegar RK, Hartnick E, Foote B, Southwick S: Posttraumatic stress disorder in hospitalized adolescents: psychiatric comorbidity and clinical correlates. J Am Acad Child Adolesc Psychiatry 1999; 38:385–392Google Scholar
41. Steinberg M: Interviewer’s Guide to the Structured Clinical Interview for DSM-IV Dissociative Disorders (SCID-D), rev. Washington, DC, American Psychiatric Press, 1994Google Scholar
42. Simeon D, Gross S, Guralnik O, Stein DJ, Schmeidler J, Hollander E: Feeling unreal: 30 cases of DSM-III-R depersonalization disorder. Am J Psychiatry 1997; 154:1107–1113Google Scholar
43. Simeon D, Guralnik O, Knutelska M, Schmeidler J: Personality factors associated with dissociation: temperament, defenses, and cognitive schemata. Am J Psychiatry 2002; 159:489–491Google Scholar
44. Herman JL, Perry JC, van der Kolk BA: Childhood trauma in borderline personality disorder. Am J Psychiatry 1989; 146:490–495Google Scholar
45. Briere J, Runtz M: Differential adult symptomatology associated with three types of child abuse histories. Child Abuse Negl 1990; 14:357–364Google Scholar
46. Lipschitz DS, Winegar RK, Nicolaou AL, Hartnick E, Wolfson M, Southwick SM: Perceived abuse and neglect as risk factors for suicidal behavior in adolescent inpatients. J Nerv Ment Dis 1999; 187:32–39Google Scholar
47. Simeon D, Guralnik O, Schmeidler J, Sirof B, Knutelska M: The role of childhood interpersonal trauma in depersonalization disorder. Am J Psychiatry 2001; 158:1027–1033Google Scholar