Comparison of Cortical 5-HT2A Receptor Binding in Bulimia Nervosa Patients and Healthy Volunteers
Abstract
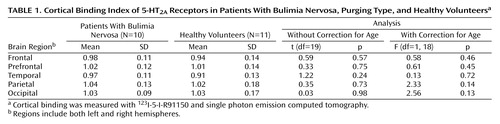
OBJECTIVE: Bulimia nervosa has been associated with alterations in central serotonergic (5-HT) function. This study investigated iodine-labeled 4-amino-N-[1-[3-(4-fluorophenoxy) propyl]-4-methyl-4-piperidinyl]-5-iodo-2-methoxybenzamide (123I-5-I-R91150) binding to the 5-HT2A receptor in the brain by using single photon emission computed tomography in acutely ill bulimia nervosa patients. METHOD: Cortical 123I-5-I-R91150 binding in 10 normal-weight patients with bulimia nervosa, purging type, was compared with that of 11 healthy volunteers. RESULTS: The 5-HT2A binding index of the bulimia nervosa patients, with and without correction for age, was not significantly different from that of the comparison group. CONCLUSIONS: As a group, acutely ill bulimia nervosa patients cannot be discriminated from healthy subjects on the basis of cortical 123I-5-I-R91150 binding to the 5-HT2A receptor.
Bulimia nervosa is characterized by binge eating and inappropriate compensatory behaviors to avoid weight gain. The etiology of bulimia nervosa likely involves interactions among genetic, psychological, and biological variables. Of interest is the attention given to neurobiological alterations. Several authors have addressed the role of the serotonin (5-HT) neurotransmitter system in bulimia nervosa. In the majority of these studies, indirect measurements of central 5-HT function were used, and contradictory results were reported (1). Single photon emission computed tomography (SPECT) allows for a more direct exploration of the central 5-HT system. The SPECT radiopharmaceutical, iodine-labeled 4-amino-N-[1-[3-(4-fluorophenoxy) propyl]-4-methyl-4-piperidinyl]-5-iodo-2-methoxybenzamide (123I-5-I-R91150), specifically binds to the 5-HT2A receptor in the brain (2). Recently, we used 123I-5-I-R91150 and SPECT to compare 5-HT2A receptor availability in anorexia nervosa patients and healthy comparison subjects and found lower 5-HT2A receptor availability in the left frontal, bilateral parietal, and occipital regions in the anorexia nervosa patients (3). The present study reports on 123I-5-I-R91150 binding in acutely ill bulimia nervosa patients.
Method
We studied 10 normal-weight patients who met the DSM-IV criteria for bulimia nervosa, purging type, without a history of anorexia nervosa (nine women, one man). Duration of the eating disorder varied between 1 and 4 years. None of the patients had a concomitant psychiatric disorder. Patients were free of psychotropic medication for at least 1 year. Additional exclusion criteria were a history of major medical or neurological disorder, previous ECT, current pregnancy or lactation, and abnormal menstrual function. Depressive symptoms were rated with the Beck Depression Inventory.
Eleven medication-free healthy volunteers (seven women, four men) without a personal or family (first-degree relatives) history of neurological and psychiatric disorder, served as the comparison group. Detailed characteristics of this group were described elsewhere (3). This study was approved by the local ethics committee. Written informed consent was obtained from each subject.
All subjects had the same standardized, low-protein breakfast on the morning of the study. Thyroid blockade was achieved by oral administration of 100 mg of potassium chloride. Subjects received 185 MBq of 123I-5-I-R91150 intravenously as a single bolus. Transmission and emission SPECT scans were performed at pseudoequilibrium (2). After automatic image coregistration to stereotactic space, a predefined volume-of-interest analysis was performed. Radioactivity estimates in the cortex represent total ligand binding. Since the cerebellum contains only a small number of 5-HT2A receptors (4), and therefore represents nonspecific activity, calculation of binding index was performed by volume-of-interest normalization to the activity-per-volume element in the cerebellum.
As binding index values were normally distributed, between-group comparisons of mean binding index were made by using two-tailed group t tests. Since 5-HT2A binding has been shown to decline with age (5), between-group comparisons were recalculated by using the general linear model procedure with age as a covariate. Correlation analyses were used to examine relationships between binding index values and psychopathological data.
Results
The 21 individuals in this study had an average age of 23.6 years (SD=3.5, range=16.9–29.3). Mean ages were significantly different between the two study groups (patients: mean=21.3 years [SD=3.2]; healthy volunteers: mean=25.6 years [SD=2.5]) (U=18, p=0.01). The two groups did not differ significantly in gender (p=0.30, Fisher’s exact test) or body mass index (U=34.5, p=0.25). None of the patients met the criteria for a major depressive episode nor for any other comorbid psychiatric disorder at the moment of the SPECT scanning. The Beck Depression Inventory score was below 10 in all patients.
Correlation analysis, in the bulimia nervosa patients as well as in the healthy subjects, revealed a significant (at the 5% level) negative relationship between age and binding index in the prefrontal cortex. In addition, a nonsignificantly negative correlation between age and binding index was found in the temporal, parietal, and occipital regions. Further, there were no significant relationships between binding index values and gender, body mass index, or disease duration. The mean 5-HT2A binding index in the bulimia nervosa patients, with and without correction for age, was not significantly different in any predefined cortical brain region from the mean binding index values in the healthy comparison subjects (Table 1).
Discussion
In this study, no changes in cortical 5-HT2A receptor binding, assessed by 123I-5-I-R91150 and SPECT, were observed in acutely ill bulimia nervosa patients, relative to healthy comparison subjects. In addition, a significantly negative relationship between binding index and age in the prefrontal cortex indicated that in bulimia nervosa patients, as well as in healthy subjects, an age-related decline in 5-HT2A receptor availability was preserved. These results agree with those of the literature (5). In a previous (indirect) study, no significant difference in CSF levels of 5-hydroxyindoleacetic acid (5-HIAA) was found between bulimia nervosa patients and healthy comparison subjects (6). This finding could indicate that central 5-HT turnover is not disturbed in acutely ill bulimia nervosa patients. Yet, in another study using [123I]β-CIT and SPECT, a reduction of available binding sites in 5-HT transporter-rich areas was documented in 10 medication-free female patients with bulimia, compared with 10 age-matched healthy female subjects (7). Although decreased [123I]β-CIT binding may reflect central 5-HT dysfunction, secondary changes may involve the postsynaptic 5-HT2A receptor as well. In a positron emission tomography study that used [18F]altanserin, a ligand for the postsynaptic 5-HT2A receptor, reduced binding in the orbital frontal cortex was found in patients who recovered from bulimia nervosa (8). Based on the observation that recovered bulimia nervosa patients have elevated CSF 5-HIAA concentrations (9) and in agreement with in vitro studies (10), the authors postulated that 5-HT2A receptors were down-regulated. Based on our findings, acutely ill bulimia nervosa patients are not characterized by altered cortical 5-HT2A receptor binding in specific (prefrontal) brain regions. These results clearly differ from those in acutely ill anorexia nervosa patients (3), suggesting that different biological mechanisms are involved in patients with different types of eating disorders.
In reporting our findings we are aware of several limitations. A major limitation of this study was the small number of subjects. Consequently, we did not correct for a large number of potential confounding factors, such as psychopathological variables.
 |
Received April 28, 2003; revisions received June 3 and Sept. 3, 2003, and Feb. 17, 2004; accepted Feb. 24, 2004. From the Division of Nuclear Medicine, the Department of Psychiatry and Medical Psychology, and the Department of Radiopharmacy, Ghent University Hospital, Ghent, Belgium. Address reprint requests to Dr. Goethals, Division of Nuclear Medicine, Polikliniek 7, Ghent University Hospital, De Pintelaan 185, 9000 Ghent, Belgium; [email protected] (e-mail). The authors thank Koen Van Laere, M.D., Ph.D., Dr.Sc., for comments on the manuscript and Erik Nolf, M.Sc., for technical advice.
1. Walsh BT, Devlin MJ: Eating disorders: progress and problems. Science 1998; 280:1387–1390Crossref, Medline, Google Scholar
2. Busatto GF, Pilowsky LS, Costa DC, Mertens J, Terriere D, Ell PJ, Mulligan R, Travis MJ, Leysen JE, Lui D, Gacinovic S, Waddington W, Lingford-Hughes A, Kerwin RW: Initial evaluation of 123I-5-I-R91150, a selective 5-HT2A ligand for single-photon emission tomography, in healthy human subjects. Eur J Nucl Med 1997; 24:119–124Crossref, Medline, Google Scholar
3. Audenaert K, Van Laere K, Dumont F, Vervaet M, Goethals I, Slegers G, Mertens J, van Heeringen C, Dierckx RA: Decreased 5-HT2a receptor binding in patients with anorexia nervosa. J Nucl Med 2003; 44:163–169Medline, Google Scholar
4. Pazos A, Probst A, Palacios JM: Serotonin receptors in the human brain, IV: autoradiographic mapping of serotonin-2 receptors. Neuroscience 1987; 21:123–139Crossref, Medline, Google Scholar
5. Baeken C, D’haenen H, Flamen P, Mertens J, Terriere D, Chavatte K, Boumon R, Bossuyt A: 123I-5-I-R91150, a new single-photon emission tomography ligand for 5-HT2A receptors: influence of age and gender in healthy subjects. Eur J Nucl Med 1998; 25:1617–1622Crossref, Medline, Google Scholar
6. Kaye WH, Ballenger JC, Lydiard RB, Stuart GW, Laraia MT, O’Neil P, Fossey MD, Stevens V, Lesser S, Hsu G: CSF monoamine levels in normal-weight bulimia: evidence for abnormal noradrenergic activity. Am J Psychiatry 1990; 147:225–229Link, Google Scholar
7. Tauscher J, Pirker W, Willeit M, de Zwaan M, Bailer U, Neumeister A, Asenbaum S, Lennkh C, Praschak-Rieder N, Brucke T, Kasper S: [123I]beta-CIT and single photon emission computed tomography reveal reduced brain serotonin transporter availability in bulimia nervosa. Biol Psychiatry 2001; 49:326–332Crossref, Medline, Google Scholar
8. Kaye WH, Frank GK, Meltzer CC, Price JC, McConaha CW, Crossan PJ, Klump KL, Rhodes L: Altered serotonin 2A receptor activity in women who have recovered from bulimia nervosa. Am J Psychiatry 2001; 158:1152–1155Link, Google Scholar
9. Kaye WH, Greeno CG, Moss H, Fernstrom J, Fernstrom M, Lilenfeld LR, Weltzin TE, Mann JJ: Alterations in serotonin activity and psychiatric symptoms after recovery from bulimia nervosa. Arch Gen Psychiatry 1998; 55:927–935Crossref, Medline, Google Scholar
10. Barnes NM, Sharp T: A review of central 5-HT receptors and their function. Neuropharmacology 1999; 38:1083–1152Crossref, Medline, Google Scholar



