Outcome of Anorexia Nervosa: A Case-Control Study
Abstract
OBJECTIVE: Although there have been many studies of the outcome of anorexia nervosa, methodological weaknesses limit their interpretation. The authors used a case-control design to try to improve knowledge about the outcome of anorexia nervosa. METHOD: All new female patients referred to an eating disorders service between Jan. 1, 1981, and Dec. 31, 1984, who had probable or definite anorexia nervosa were eligible for inclusion. Of these women, 86.4% (N=70) were located and agreed to participate. The comparison group (N=98) was a random community sample. All subjects were interviewed with a structured diagnostic instrument. RESULTS: A minority of the patients (10%) continued to meet the criteria for anorexia nervosa a mean of 12 years after initial referral. Even among those who no longer met these criteria, relatively low body weight and cognitive features characteristic of anorexia nervosa (perfectionism and cognitive restraint) persisted. The rates of lifetime comorbid major depression, alcohol dependence, and a number of anxiety disorders were very high. CONCLUSIONS: In the managed care/brief treatment era, therapeutic approaches with an excessive focus on weight gain that neglect the detection and treatment of associated psychological features and comorbidity may be inappropriate. Anorexia nervosa is a serious psychiatric disorder with substantial morbidity. (Am J Psychiatry 1998; 155:939–946)
There have been many studies of the outcome of anorexia nervosa, and high-quality reviews are available (1–7). Although the majority of individuals studied no longer have anorexia nervosa at the time of follow-up (6, 7), substantial psychiatric comorbidity is common (5), and the risk of a fatal outcome is considerable (8–10). Taken together, these studies have demonstrated clearly that anorexia nervosa is a serious psychiatric disorder with substantial morbidity and mortality.
As has been noted (1), however, interpretation of many of the individual studies of the outcome of anorexia nervosa is hampered by numerous methodological weaknesses. These weaknesses include small sample sizes, poor case definitions, and unstandardized and unstructured diagnostic methods. An additional and critical weakness is the general lack of control or comparison groups. These methodological limitations constrain our knowledge of “recovery” from anorexia nervosa and our interpretation of the rather high lifetime prevalence of comorbid diagnoses that is often observed. Consequently, although we may have a general impression of the outcome of anorexia nervosa and its mortality rates, many important details remain obscure.
The purpose of this study was twofold. First, we identified, located, and interviewed—using clear diagnostic definitions and a structured method—women who had been referred for treatment of anorexia nervosa an average of 12 years earlier in order to ascertain their intermediate to long-term outcome. Second, using a case-control design, we compared the outcome of these patients with anorexia nervosa to the status of a random community comparison group screened for the presence of anorexia nervosa.
METHOD
The purpose of this study was to assess the outcome of anorexia nervosa across a number of domains. The design was two-pronged: a historical observational cohort study, in which women with anorexia nervosa (N=70) who had been assessed or treated more than a decade earlier were located and followed up, paired with a case-control study (N=98 in the comparison group). In conjunction with case-control comparisons, the magnitude and significance of outcomes such as depression and functional impairment could be assessed. The study was reviewed and approved by the local ethics committee, and all subjects provided written informed consent.
Potential cases of anorexia nervosa were drawn from the records of the Eating Disorders Service at The Princess Margaret Hospital in Christchurch, New Zealand. This service has been in existence since 1978 and remains the sole specialist assessment and treatment service for eating disorders in the South Island of New Zealand. Any woman assessed or treated by the Eating Disorders Service for the first time from Jan. 1, 1981, to Dec. 31, 1984, was eligible for inclusion in this study. Specifically, this refers to patients admitted, outpatients first seen, and patients assessed during this time period. We studied newly referred patients in order to minimize an important bias (“the clinician's illusion” [11]), which would have severely limited the generalizability of our findings. If we had studied the total set of women with anorexia nervosa, we would have oversampled individuals with chronic anorexia; if our study group had had relatively more individuals with chronic anorexia nervosa, our results would have been less pertinent to the clinical question of the likely prognosis of a patient at the point of referral.
The hospital record of every newly referred patient during 1981–1984 was independently reviewed and abstracted (using a standardized form) by two trained medical students under the close supervision of one of us (P.F.S.). Following a consensus conference between the two raters and the supervisor, potential “cases” were defined as anyone first seen by the Eating Disorders Service in 1981–1984 who met the DSM-III or DSM-III-R criteria for definite or probable anorexia nervosa.
To locate potential cases of anorexia nervosa, we used a variety of methods. First, we arranged for a computerized search of the New Zealand mortality database to identify any women who might have been “case” subjects who had died. Second, we used a wide variety of sources to attempt to obtain a current address and telephone number for each potential anorexia nervosa subject. These sources included the addresses listed in the hospital case notes (e.g., for the person, parents, and general practitioner), all New Zealand telephone directories, and the electoral roll directories. For women not identified through these means, we arranged for a search of the New Zealand Register of Births, Deaths, and Marriages to identify the names of any women who might have married and changed their names. Finally, we also checked the telephone directories and electoral rolls for the major metropolitan areas in Australia.
To obtain a community sample of adult women, we randomly selected individuals from the 1993 Christchurch electoral rolls. All adults are required by New Zealand law to register for the electoral roll, and 95.5% of the adult population was in fact registered (12). The comparison group was restricted to women in the same age band as the women with anorexia nervosa (i.e., current age=23–45 years). Three women with a history of anorexia nervosa or subthreshold anorexic symptoms were excluded.
Data Collection Protocol
All potential anorexia nervosa subjects who were located were sent a letter from the consultant psychiatrist who had been on the Eating Disorders Service in the early 1980s. This letter described the study and invited participation. The letter was followed a few days later by a telephone call from the study interviewer (A.P.). She explained the study further and attempted to obtain consent for a personal interview. The interview was performed face-to-face with 91.4% of the patients, and the remainder were interviewed by telephone when geographic distance was prohibitive (i.e., residence in Australia, England, or North America).
All potential comparison subjects were sent a letter describing the study and requesting participation. This was followed a few days later by a telephone call from the study interviewer, who attempted to obtain consent for a personal interview.
The study interviewer had previously completed more than 500 structured psychiatric interviews, which included over 100 with the instrument used in this study. She underwent additional training to prepare her for interviewing women with eating disorders and was directly supervised by P.F.S. She met with the investigators on a weekly basis to discuss progress in the study and to clarify any uncertainties that had arisen. Because of the nature of the contact protocol, it was impossible for the interviewer to be blind to case-control status.
The subject interview had several components. The first component was a standardized and structured diagnostic interview, the Diagnostic Interview for Genetic Studies (13, 14), which yields lifetime and current DSM-III-R diagnoses of mood disorders, substance use disorders, anxiety disorders, eating disorders, childhood conduct disorder, and adult antisocial personality. The Diagnostic Interview for Genetic Studies also collects information about demo~graphic characteristics, medical and psychiatric history, psychotic symptoms, the temporal course of comorbid disorders, and suicidal behavior. We modified the instrument to obtain more detailed information about eating disorder symptoms and their time course (using a life history chart to facilitate active recall) and added sections on childhood overanxious disorder and separation anxiety disorders (modified from versions by K.R. Merikangas, unpublished). In addition, the interviewer rated each subject's current “global” social and occupational functioning (Global Assessment of Functioning Scale) (15 and DSM-III-R).
The second component was a booklet that contained several self-report inventories. In this article, we report the results from the first five scales (drive for thinness, bulimia, body dissatisfaction, perfectionism, and interoceptive awareness) of the Eating Disorders Inventory (16, 17) and the cognitive restraint, disinhibition, and hunger scales of the Three-Factor Eating Questionnaire (18).
All available medical records were requested for any subject who had had a psychiatric hospitalization or a medical admission or specialist referral that might have been related to an eating disorder (e.g., an outpatient amenorrhea investigation).
Psychiatric Diagnoses
The completed Diagnostic Interview for Genetic Studies interviews were reviewed independently by two of us (P.F.S. and C.M.B.), who were blind to subjects' case or control status while doing the reviews. The eating disorders section was reviewed after diagnoses for all other sections had been recorded in order to minimize any tendency to assign diagnoses with reference to case-control status. Using all available information, the two of us independently assigned psychiatric diagnoses according to DSM-III-R criteria. The diagnostic standard was conservative: no diagnosis was given unless there was clear, positive supporting evidence, and none was given if there was substantial disagreement between the two diagnostic raters.
The lifetime prevalence of most DSM-III-R psychiatric syndromes in the community comparison group was comparable to that in a much larger study in Christchurch that used electoral roll sampling (12). However, because the Diagnostic Interview for Genetic Studies was overly sensitive to diagnosing lifetime major depression (e.g., lifetime prevalence in the comparison group was 53.0%), we made the DSM-III-R criteria more stringent by requiring functional impairment plus a minimum 4-week duration of symptoms (19).
Statistical Analysis
We considered the outcome of anorexia in three domains. The first outcome domain concerned eating-disorder-related psychopathology and consisted of the follow-up diagnoses of anorexia nervosa and bulimia nervosa plus self-reported body mass index and psychometric scores (Eating Disorders Inventory and Three-Factor Eating Questionnaire). The second outcome domain was other lifetime psychiatric diagnostic comorbidity (i.e., mood, anxiety, and substance use disorders). The third outcome domain was global social and occupational functioning (Global Assessment of Functioning Scale) as an aggregate or summation measure of the functioning of these women. Since these measures were also obtained in a random community sample, we were able to assess their significance and magnitude.
We used simple statistics (chi-square test, analysis of variance, and analysis of covariance) (20) to compare the subjects in the anorexia group with those in the community group. All p values are two-tailed. Assuming alpha=0.05 and beta=0.80, these comparisons could detect differences in continuous variables of medium magnitude (d=0.44) and differences in discrete variables of small to medium magnitude (w=0.21) (21).
RESULTS
Of the referrals between Jan. 1, 1981, and Dec. 31, 1984, 239 records were abstracted because they contained some evidence of an eating disorder. Upon review, 89 individuals were thought to have had definite or probable anorexia nervosa. Of these 89 potential subjects, one person had died, three could not be located, eight did not give full consent, and upon interview and diagnostic review, seven clearly had never met criteria for anorexia nervosa. (The single death was that of a woman in her early 20s who had committed suicide while hospitalized for the treatment of severe anorexia nervosa. She was notable for her high impulsiveness and rather extreme reluctance to engage in treatment.) Therefore, personal interviews with 70 women were obtained, all of whom met lifetime DSM-III-R criteria for anorexia nervosa. The participation rate for persons with anorexia was thus 86.4% (70/[89–1–7]). For the comparison group, 111 women were approached; 10 refused and three were excluded because of the presence of subthreshold anorexic symptoms. Personal interviews were obtained with 98 women, none of whom met lifetime DSM-III-R criteria for anorexia nervosa. The participation rate for the comparison group was 91.0% (101/111). The participation rates for the anorexic subjects and the comparison subjects were not statistically different (χ2=1.01, df=1, p=0.32) and were somewhat greater than the rate in the large community survey that used the Christchurch electoral rolls (12).
In comparison with 49 other studies of the outcome of anorexia nervosa (10), the total number of cases (N=70) was larger than the norm (median=48, mean=66), and the participation rate (86.4%) was similar (median=89%, mean=84%). However, the participation rate of the comparison group places the latter figure in context, since potential comparison subjects were as likely as potential subjects with anorexia not to participate in the study. The mean age at onset of anorexia in our study group (table 1) was similar to that in four large outcome studies (8, 22–24). The follow-up interval in our group (i.e., time from initiation of treatment to outcome interview; mean=12.0 years, range=9.8–14.4) was greater than the median (7.2 years) or the mean (9.1 years) in the 49 other studies of the outcome of anorexia nervosa.
Despite our attempt to match case subjects and comparison subjects by age banding, the mean age of the comparison group was significantly greater than that of the anorexia group (table 1). Because many of the outcomes we studied are influenced by age (e.g., marriage and risk of depression), we incorporated age at interview as a covariate in the analyses that follow. The anorexia group and the comparison group were otherwise similar in demographic characteristics, with the exception of marital status; even when we controlled for current age, the anorexic subjects were markedly less likely to have ever been married.
The single death in the anorexia group was that of the woman who had committed suicide while hospitalized for treatment of anorexia nervosa. Thus, the crude mortality rate was 1.4%, or 0.0017% per person-year of follow-up.
Table 2 presents data on the first outcome domain. By definition, all members of the anorexia group and none of the comparison group met the criteria for lifetime anorexia nervosa. At the outcome interview, 15.7% of the anorexia group continued to meet criteria for full syndromic or subthreshold anorexia nervosa. Over one-half the anorexia group had met criteria for lifetime bulimia nervosa—a far greater proportion than in the comparison group—and 15.7% of the anorexia group and none of the comparison group continued to meet criteria for full syndromic or subthreshold bulimia nervosa. Only one individual had both current anorexia nervosa and bulimia nervosa.
There were profound differences between the anorexia patients and the comparison group on all of the body mass index variables. Some of these differences followed from the case and comparison group definitions (e.g., lowest adult body mass index). However, even when we controlled for the presence of current anorexia nervosa, there were marked differences between the anorexic subjects and the comparison group in current body mass index and reported ideal body mass index. For example, the mean body mass index at interview for the subjects with current anorexia nervosa was 16.9 (SD=1.1), and for the subjects without current anorexia nervosa it was 20.4 (SD=1.8).
On the Eating Disorders Inventory and Three-Factor Eating Questionnaire, there were significant differences between the anorexia group and the comparison group in drive for thinness and perfectionism on the former and in cognitive restraint and hunger on the latter. These differences were statistically significant when we controlled for the presence of current anorexia nervosa. The anorexia group was characterized by higher drive for thinness, perfectionism, and cognitive restraint and by lower hunger.
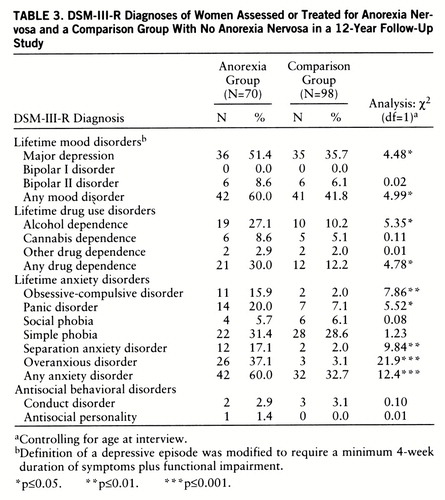
Table 3 presents the DSM-III-R/Diagnostic Interview for Genetic Studies diagnoses of the anorexia group and the comparison group. There were significant differences across groups in the lifetime prevalence of any mood, anxiety, and substance use disorders. In particular, major depression, alcohol dependence, obsessive-compulsive disorder, panic disorder, separation anxiety disorder, and overanxious disorder were significantly more common in the anorexia group than in the comparison group.
The mean Global Assessment of Functioning Scale score of the anorexia group (68.9, SD=15.9) was significantly worse than that of the comparison group (80.3, SD=10.0) (F=36.0, df=1,166, p<0.001). Since this score is an aggregate measure that is influenced by any current disorder, we refined this analysis by performing a multiple regression with Global Assessment of Functioning Scale score as the dependent variable and the independent variables of case-control status, age, and the presence of any current eating, mood, anxiety, or drug/alcohol dependence disorder. After controlling for all of these covariates, we found that the anorexia group had significantly worse Global Assessment of Functioning Scale scores than the comparison group (F=9.70, df=1,161, p=0.002).
DISCUSSION
In this study, we investigated the outcome of 70 women who had been referred for treatment of anorexia nervosa a mean of 12.0 years earlier (a mean of 15.4 years after onset of the disorder) across three domains. The study had several important methodological features that facilitate its interpretability and that allow a more accurate portrait of the outcome of anorexia nervosa. Although these features have been used in prior studies of the outcome of anorexia nervosa, to our knowledge all three have not been used previously. First, we studied individuals at the point of first referral to a specialist treatment facility, avoiding a sample artifactually enriched by individuals with chronic anorexia nervosa and thereby yielding data directly applicable to the clinically important question of an individual's prognosis at the point of first referral. Second, as has been advocated (1, 5, 7), we paid careful attention to a number of procedural details, including case ascertainment, tracing, interviewing, and the use of structured diagnostic interviews. Of note, the participation rate of women with anorexia was typical of that in other studies of the outcome of anorexia nervosa and not significantly different from that of the comparison group. Third, the interpretation of these data was facilitated by the simultaneous recruitment of a random community comparison group. Only a minority of previous studies of the outcome of anorexia nervosa have included comparison groups (25–30), and in most of these studies, the comparison group was not randomly sampled nor necessarily representative of the general population. Our comparison group was comparable to the anorexia group in terms of ethnicity and occupation and appeared to have lifetime prevalences of many psychiatric disorders in the ranges of those reported in several community samples of studies conducted in Christchurch. Current age was an important exception: despite our use of age banding, the anorexic subjects were significantly younger than the comparison subjects. We controlled for this difference by including current age as a covariate in all subsequent analyses.
Eating Disorder Outcomes
The first outcome domain pertained to mortality and eating-disorder-related psychopathology. There was only one death in the group studied. A meta-analysis estimated the risk of mortality in anorexia nervosa to be 5.6% per decade of follow-up (10). The observed mortality was thus slightly less than expected but consistent with a trend toward decreased mortality in more recent treatment cohorts (7).
More than a decade after first referral for treatment, a substantial fraction of the study group continued to meet the criteria for anorexia nervosa (10.0%) or a subthreshold variant (5.7%). Strict comparison with prior studies is made difficult by the varying study designs and different diagnostic and outcome definitions that were used. Prior studies of the outcome of anorexia nervosa that used operationalized diagnostic criteria after a decade or more of follow-up have reported persistent anorexia nervosa in approximately 11% (29) to 17% (31) of subjects. When less precise definitions have been used, chronic symptoms, a poor outcome, or an unimproved clinical state has been reported in from 16% (32) to over 50% (33) of subjects. Thus, our finding is generally consistent with prior reports: chronic anorexic symptoms appear to persist in a sizable minority of patients even after a relatively long period of follow-up.
Of particular interest was our finding that the anorexic subjects and the comparison group differed in several body mass index, Eating Disorders Inventory, and Three-Factor Eating Questionnaire variables. The anorexia group had a markedly lower body mass index than the comparison group and reported an ideal body mass index that was both lower than that of the comparison group and fairly close to their own current body mass indexes. These data suggest—even after control for age and the presence of current anorexia nervosa—that anorexia patients are distinguished by a persisting focus on thinness and by maintaining a relatively low body weight. Self-reported higher scores on Eating Disorders Inventory drive for thinness, higher scores on Three-Factor Eating Questionnaire cognitive restraint, and lower scores on Three-Factor Eating Questionnaire hunger are consistent with this finding.
Although most of the subjects in our anorexia group no longer met the criteria for anorexia nervosa in terms of low weight and amenorrhea, body shape and weight concerns clearly persisted in a manner that was distinct from the comparison group. Maintaining the “anorectic stance” (34) over time is highly demanding and subjects the individual to substantial scrutiny and both wanted and unwanted attention. At some point, the primary and secondary gain of anorexic symptoms may become not worth the effort. A common pathway in recovery from anorexia nervosa may be for an individual's eating to normalize somewhat, with a subsequent increase in body weight, perhaps even into the low normal or normal range. This allows the individual to retain the perceived benefits of a relatively low body weight without the costs of maintaining an extremely low body weight in the anorexic range. The self-report results (higher Eating Disorders Inventory drive for thinness score and Three Factor Eating Questionnaire cognitive restraint score) suggest that maintenance of low body weight in otherwise “recovered” patients had a conscious or intentional component. The lower Three-Factor Eating Questionnaire hunger scores could reflect either conscious underreporting or biological alterations in appetite and satiety (35) that were consequences of anorexia nervosa or that existed premorbidly. Differences in satiety and appetitive mechanisms in women with eating disorders remain important empirical questions.
Perfectionist traits are frequently observed during the acute phase of anorexia nervosa (36) and may play a causal role in its development (37). Our findings indicate that high perfectionism is not restricted to the acute phase of the illness. Even after controlling for the presence of a current eating disorder, we found that anorexic subjects had markedly higher Eating Disorders Inventory perfectionism scores than the comparison group. These results are consistent with those of Srinivasagam et al. (38), who found that perfectionism scores were significantly higher among individuals with anorexia nervosa who had been weight-recovered for more than 1 year than among control subjects. Our findings suggest that this trait persists even longer. Bastiani et al. (36) hypothesized that perfectionism may reflect one dimension of the rigidity and obsessionality that contribute to vulnerability to developing anorexia nervosa, resistance to treatment, and likelihood of relapse.
A substantial proportion of the study group developed bulimia nervosa at some point over the follow-up period, although this persisted through to the follow-up interview in only a minority. The proportion who developed bulimia nervosa was grossly greater among the anorexic subjects than in the comparison group, consistent with epidemiological evidence that anorexia is a strong risk factor for bulimia (39). We investigated the phenomenon of “crossover” from anorexia nervosa to bulimia nervosa in this group in a prior report (40). Briefly, we found that most individuals developed bulimia nervosa within 2 years of the onset of anorexia nervosa and that the development of bulimia nervosa was unusual more than 5 years after the onset of anorexia nervosa. Using Cox proportional hazard modeling with time-dependent covariates, we determined that “recovery” from anorexia nervosa was a potent risk factor (risk ratio=2.8) for this transition. Conversion from anorexia nervosa to bulimia nervosa may represent a way of retaining eating disorder pathology in a manner less evident to family, friends, and health care workers (i.e., to move from a “visible” to an “invisible” eating disorder).
Psychiatric Diagnostic Comorbidity
A key concern is whether the comparison group was representative of the local populace with respect to the probability of having lifetime psychiatric disorders. Comparison data are available from a randomized community survey based on census data of 1,498 adults conducted in Christchurch (with use of DSM-III and the Diagnostic Interview Schedule [DIS]) (41) and from 1,028 adults randomly selected from the Christchurch electoral rolls as the control group in a suicide study (with use of DSM-III-R and the Structured Clinical Interview for DSM-III-R [SCID]) (12). In our comparison group, the lifetime prevalence estimates for most disorders appear to be comparable to the community lifetime prevalences (41). There were two exceptions: the lifetime prevalence of major depression (by criteria more stringent than those in DSM-III-R) was greater in our comparison group (35.7%) than in the DIS-based community survey (16.3%) (41). Since the DIS may underdiagnose major depression (42), it is notable that a SCID-based survey found the lifetime prevalence of major depression in women aged 23–46 years to be 47.1% (A. Beautrais, personal communication, June 1996). The second exception was the lifetime prevalence of alcohol dependence, which was higher in our comparison group (10.2%) than in one community survey (6.1%) (41). For depression and alcohol dependence, the higher prevalences in our comparison group imparted a conservative bias by making it harder to detect a significant difference between anorexic subjects and the comparison group.
The lifetime prevalences of major depression, alcohol dependence, and, notably, several anxiety disorders (obsessive-compulsive, panic, separation anxiety, and overanxious disorders) were significantly greater in the anorexia group than in the comparison group. The finding of a high prevalence of lifetime major depression is in accord with other studies that used structured interviews (43, 44) and with those that also used a control group (28, 29, 45). In these studies, lifetime prevalences of major depression ranged from 40% to 100%. The association of anorexia nervosa with mood disorders has intrigued researchers for decades (46) and has led to suggestions that anorexia nervosa is a forme fruste of affective illness. This appears to be unlikely; with stringent definitions of major depression such as those in our study, the lifetime prevalence of major depression is far less than 100%. However, anorexia nervosa is likely to be a heterogeneous condition, and affective illness may be etiologically related to it in a subset of subjects. Alternatively, the association between anorexia nervosa and affective illness may represent confounding, with both conditions resulting from common genetic or environmental causes.
Halmi et al. (29) expected to—but did not—find a greater lifetime prevalence of alcohol dependence in their follow-up sample of anorexic subjects than in control subjects. In our study, over one-fourth of the anorexia group reported a lifetime history of alcohol dependence. The structured diagnostic interview that we used was designed, in part, for genetic studies of alcoholism and has a very careful assessment of alcohol use. Our finding, which is in accord with clinical experience, may have resulted from the greater sensitivity of the Diagnostic Interview for Genetic Studies. This finding is also plausible and may represent maladaptive anxiolytic pharmacotherapy (“self-medication”) given the very high prevalence of anxiety disorders or more general and persistent difficulties in coping with life.
A striking finding in our study was the very high lifetime prevalence of several anxiety disorders. Prior reports have noted significantly elevated prevalences of obsessive-compulsive disorder (28, 29, 45), panic disorder (28), and social phobia (28, 29) (the latter was not found in the present study). However, the two childhood anxiety disorders (separation anxiety and overanxious disorders) were markedly more prevalent in the anorexia group than in the comparison group. We are aware of no other case-control comparisons of these disorders in anorexia nervosa. In a prior report (47), we compared the lifetime prevalences of several anxiety disorders across four groups (case subjects and control subjects from this study plus clinical samples of women with bulimia nervosa and major depression). In multivariate analyses, anorexia nervosa appeared to be particularly associated with obsessive-compulsive disorder (odds ratio=11.8, p=0.03) and overanxious disorder (odds ratio=13.4, p=0.003). Given these findings, it appears more likely that anorexia nervosa may be closely allied to certain anxiety disorders than to affective disorders.
Global Functioning
Although worse overall or global functioning in samples treated previously for anorexia nervosa has been reported (e.g., reference 30), the studies have typically not controlled for additional psychopathology whose symptoms often impair functioning. In contrast to the comparison group, and after control for the presence of current eating, mood, anxiety, and drug/alcohol dependence disorders, our anorexia group still had significantly worse Global Assessment of Functioning Scale scores. This finding suggests that women referred for treatment of anorexia nervosa many years earlier remain notable for worse global functioning, even taking into account their high prevalence of chronicity, crossover to bulimia nervosa, and comorbid psychiatric disorders.
Limitations and Implications of the Study
Our findings must be interpreted in the context of three potentially important limitations. First, although this was the only practical design available to us, we studied a group of subjects who were referred for treatment, and important but unknown biases may have distinguished these individuals from the wider population from which they were drawn. Second, we relied heavily on retrospective self-report. Although we used a structured diagnostic interview supplemented by medical records when available, recall bias could have altered our results, especially if it was more prominent in the anorexia group than in the comparison group. Third, the study interviewer was, unavoidably, not blind to case-control status. We attempted to compensate for this by a blind diagnostic review (of the non-eating-disorders sections of the Diagnostic Interview for Genetic Studies) by two clinicians and the use of a conservative diagnostic standard.
In our study group, as in many others, only a minority of the subjects continued to meet the criteria for anorexia nervosa more than a decade after initial referral. However, even in recovery (i.e., when the criteria for anorexia nervosa were no longer met), relatively low body weight and certain cognitive features (perfectionism and cognitive restraint) tended to persist. Comorbid major depression, alcohol dependence, and a number of anxiety disorders were very frequent. In the managed care/brief treatment era, therapeutic approaches with an excessive focus on weight gain that neglect the detection and treatment of associated attitudes and comorbidity may be inappropriate. Anorexia nervosa is a serious psychiatric disorder with substantial morbidity.
 |
 |
 |
Received Sept. 11, 1997; revision received Dec. 31, 1997; accepted Feb. 9, 1998. From the Department of Psychiatry, Virginia Institute for Psychiatric and Behavioral Genetics, Virginia Commonwealth University; the New Zealand Health Information Service, Wellington; and the University Department of Psychological Medicine, Christchurch School of Medicine, Christchurch, New Zealand. Address reprint requests to Dr. Sullivan, Department of Psychiatry, Virginia Institute for Psychiatric and Behavioral Genetics, P.O. Box 980126, Richmond, VA 23298-0126; [email protected] (e-mail). Supported by the Canterbury Medical Research Foundation and a research training fellowship from the New Zealand Health Research Council to Dr. Sullivan. The authors thank Prof. Peter Joyce; Drs. Janice McKenzie, J. Elisabeth Wells, Kim McFadden, and Ingrid Jolley; and the study participants for their assistance.
1 Hsu LKG: Outcome of anorexia nervosa: a review of the literature (1954–1978). Arch Gen Psychiatry 1980; 37:1041–1046Crossref, Medline, Google Scholar
2 Schwartz DM, Thompson MG: Do anorectics get well? current research and future needs. Am J Psychiatry 1981; 138:319–323Link, Google Scholar
3 Swift WJ: The long-term outcome of early-onset anorexia nervosa. J Am Acad Child Psychiatry 1982; 21:38–46Crossref, Medline, Google Scholar
4 Steinhausen HC, Glanville K: Follow-up studies of anorexia nervosa: a review of research findings. Psychol Med 1983; 13:239–249Crossref, Medline, Google Scholar
5 Herzog DB, Keller MB, Lavori PW: Outcome in anorexia nervosa and bulimia nervosa: a review of the literature. J Nerv Ment Dis 1988; 176:131–143Crossref, Medline, Google Scholar
6 Hsu LKG: The outcome of anorexia nervosa: a reappraisal. Psychol Med 1988; 18:807–812Crossref, Medline, Google Scholar
7 Steinhausen H-C, Rauss-Mason C, Seidel R: Follow-up studies of anorexia nervosa: a review of four decades of outcome research. Psychol Med 1991; 21:447–454Crossref, Medline, Google Scholar
8 Patton GC: Mortality in eating disorders. Psychol Med 1988; 18:947–951Crossref, Medline, Google Scholar
9 Crisp AH, Callender JS, Halek C, Hsu LKG: Long-term mortality in anorexia nervosa: a 20-year follow-up of the St George's and Aberdeen cohorts. Br J Psychiatry 1992; 161:104–107Crossref, Medline, Google Scholar
10 Sullivan PF: Mortality in anorexia nervosa. Am J Psychiatry 1995; 152:1073–1074Link, Google Scholar
11 Cohen P, Cohen J: The clinician's illusion. Arch Gen Psychiatry 1984; 41:1178–1182Crossref, Medline, Google Scholar
12 Beautrais AL, Joyce PR, Mulder RT, Fergusson DM, Deavoll BJ, Nightingale SK: Prevalence and comorbidity of mental disorders in persons making serious suicide attempts: a case-control study. Am J Psychiatry 1996; 153:1009–1014Link, Google Scholar
13 Nurnberger JI, Blehar MC, Kaufmann CA, York-Cooler C, Simpson SG, Harkavy-Friedman J, Severe JB, Malaspina D, Reich TD: Diagnostic Interview for Genetic Studies: rationale, unique features, and training. Arch Gen Psychiatry 1994; 51:849–859Crossref, Medline, Google Scholar
14 Frances A: The Diagnostic Interview for Genetic Studies. Arch Gen Psychiatry 1994; 51:863–864Crossref, Google Scholar
15 Endicott J, Spitzer RL, Fleiss JL, Cohen J: The Global Assessment Scale: a procedure for measuring overall severity of psychiatric disturbance. Arch Gen Psychiatry 1976; 33:766–771Crossref, Medline, Google Scholar
16 Garfinkel DM, Olmsted MP, Polivy J: The Eating Disorders Inventory: a measure of cognitive-behavioral dimensions of anorexia nervosa and bulimia, in Anorexia Nervosa: Recent Developments in Research. Edited by Darby PL, Garfinkel PE, Garner DM, Coscina DV. New York, Alan R Liss, 1983, pp 173–184Google Scholar
17 Garner DM: Eating Disorders Inventory-2: Professional Manual. Odessa, Fla, Psychological Assessment Resources, 1991Google Scholar
18 Stunkard AJ, Messick S: Three-Factor Eating Questionnaire to measure dietary restraint, disinhibition, and hunger. J Psycho~som Res 1985; 29:71–83Crossref, Medline, Google Scholar
19 Gershon ES, Mark A, Cohen N, Belizon N, Baron M, Knobe KE: Transmitted factors in the morbid risk of affective disorders: a controlled study. J Psychiatr Res 1975; 12:283–299Crossref, Google Scholar
20 SAS User's Guide: Basics. Cary, NC, SAS Institute, 1982Google Scholar
21 Cohen J: Statistical Power Analysis for the Behavioral Sciences. Hillsdale, NJ, Lawrence Erlbaum Associates, 1988Google Scholar
22 Crisp AH, Hsu LKG, Harding B, Hartshorn J: Clinical features of anorexia nervosa: a study of a consecutive series of 102 female patients. J Psychosom Res 1980; 24:179–191Crossref, Medline, Google Scholar
23 Isager T, Brinch M, Kreiner S, Tolstrup K: Death and relapse in anorexia nervosa: survival analysis of 151 cases. J Psychiatr Res 1985; 19:515–521Crossref, Medline, Google Scholar
24 Szmukler G, McCance C, McCrone L, Hunter D: Anorexia nervosa: a psychiatric case register study from Aberdeen. Psycho~som Med 1986; 16:49–58Crossref, Medline, Google Scholar
25 Casper RC: Personality features of women with good outcome from restricting anorexia nervosa. Psychol Med 1990; 52:156–170Crossref, Google Scholar
26 Engel K: Prognostic factors in anorexia nervosa. Psychother Psychosom 1988; 49:137–144Crossref, Medline, Google Scholar
27 Rollins N, Piazza E: Anorexia nervosa: a quantitative approach to follow-up. J Am Acad Child Psychiatry 1981; 20:167–183Crossref, Medline, Google Scholar
28 Toner BB, Garfinkel PE, Garner DM: Affective and anxiety disorders in the long-term follow-up of anorexia nervosa. Int J Psychiatry Med 1988; 18:357–364Crossref, Medline, Google Scholar
29 Halmi KA, Eckert E, Marchi P, Sampurgnaro V, Apple R, Cohen J: Comorbidity of psychiatric diagnoses in anorexia nervosa. Arch Gen Psychiatry 1991; 48:712–718Crossref, Medline, Google Scholar
30 Gillberg IC, Råstam M, Gillberg C: Anorexia nervosa outcome: six-year controlled longitudinal study of 51 cases including a population cohort. J Am Acad Child Adolesc Psychiatry 1994; 33:729–739Crossref, Medline, Google Scholar
31 Rosenvinge JH, Mouland SO: Outcome and prognosis of anorexia nervosa: a retrospective study of 41 subjects. Br J Psychiatry 1990; 156:92–97Crossref, Medline, Google Scholar
32 Beck JC, Br<179>chner-M<179>rtensen K: Observations on the prognosis in anorexia nervosa. Acta Med Scand 1954; 149:409–430Crossref, Medline, Google Scholar
33 Frazier SH: Anorexia nervosa. Dis Nerv Syst 1965; 26:155–159Medline, Google Scholar
34 Crisp AH: Anorexia nervosa. Proc R Soc Med 1977; 70:464–470Medline, Google Scholar
35 Kaye WH: Neuropeptide abnormalities in anorexia nervosa. Psychiatry Res 1996; 62:65–74Crossref, Medline, Google Scholar
36 Bastiani AM, Rao R, Weltzin T, Kaye WH: Perfectionism in anorexia nervosa. Int J Eating Disorders 1995; 17:147–152Crossref, Medline, Google Scholar
37 Strober M: Personality factors in anorexia nervosa. Pediatrician 1983–1985; 12(2–3):134–138Google Scholar
38 Srinivasagam NM, Kaye WH, Plotnikov KH, Greeno C, Weltzin TE, Rao R: Persistent perfectionism, symmetry, and exactness after long-term recovery from anorexia nervosa. Am J Psychiatry 1995; 152:1630–1634Link, Google Scholar
39 Kendler KS, MacLean C, Neale M, Kessler R, Heath A, Eaves L: The genetic epidemiology of bulimia nervosa. Am J Psychiatry 1991; 148:1627–1637Link, Google Scholar
40 Bulik CM, Sullivan PF, Fear JL, Pickering A: Predictors of the development of bulimia nervosa in women with anorexia nervosa. J Nerv Ment Dis 1997; 185:704–707Crossref, Medline, Google Scholar
41 Wells JE, Bushnell JA, Hornblow AR, Joyce PR, Oakley-Browne MA: Christchurch psychiatric epidemiology study, part I: methodology and lifetime prevalence for specific psychiatric disorders. Aust NZ J Psychiatry 1989; 23:315–326Crossref, Medline, Google Scholar
42 Parker G: Are the lifetime prevalence estimates in the ECA study accurate? Psychol Med 1987; 17:275–282Google Scholar
43 Greenfeld DG, Anyan WR, Hobart M, Quinlan DM, Plantes M: Insight into illness and outcome in anorexia nervosa. Int J Eating Disorders 1991; 10:101–109Crossref, Google Scholar
44 Smith C, Feldman SS, Nasserbakht A, Steiner H: Psychological characteristics and DSM-III-R diagnoses at 6-year follow-up of adolescent anorexia nervosa. J Am Acad Child Adolesc Psychiatry 1993; 32:1237–1245Crossref, Medline, Google Scholar
45 Råstam M, Gillberg IC, Gillberg C: Anorexia nervosa 6 years after onset, part II: comorbid psychiatric problems. Compr Psychiatry 1995; 36:70–76Crossref, Medline, Google Scholar
46 Cantwell DP, Stuzenberger S, Burroughs J, Salkin B, Green JK: Anorexia nervosa: an affective disorder? Arch Gen Psychiatry 1977; 34:1087–1093Google Scholar
47 Bulik CM, Sullivan PF, Fear JL, Joyce PR: Eating disorders and antecedent anxiety disorders: a controlled study. Acta Psychiatr Scand 1997; 96:101–107Crossref, Medline, Google Scholar



