Sleep Disturbances in the Vietnam Generation: Findings From a Nationally Representative Sample of Male Vietnam Veterans
Abstract
OBJECTIVE: This study analyzed questionnaire items that address complaints about sleep from the National Vietnam Veterans Readjustment Study, a nationally representative sample of the 3.1 million men and women who served in Vietnam. This study compared the frequency of nightmares and difficulties with sleep onset and sleep maintenance in male Vietnam theater veterans with male Vietnam era veteran and male civilian comparison subjects. It focused on the role of combat exposure, nonsleep posttraumatic stress disorder (PTSD) symptoms, comorbid psychiatric and medical disorder, and substance abuse in accounting for different domains of sleep disturbance. METHOD: The authors undertook an archival analysis of the National Vietnam Veterans Readjustment Study database using correlations and linear statistical models. RESULTS: Frequent nightmares were found exclusively in subjects diagnosed with current PTSD at the time of the survey (15.0%). In the sample of veterans who served in Vietnam (N=1,167), combat exposure was strongly correlated with frequency of nightmares, moderately correlated with sleep onset insomnia, and weakly correlated with disrupted sleep maintenance. A hierarchical multiple regression analysis showed that in Vietnam theater veterans, 57% of the variance in the frequency of nightmares was accounted for by war zone exposure and non-sleep-related PTSD symptoms. Alcohol abuse, chronic medical illnesses, panic disorder, major depression, and mania did not predict the frequency of nightmares after control for nonsleep PTSD symptoms. CONCLUSIONS: Frequent nightmares appear to be virtually specific for PTSD. The nightmare is the domain of sleep disturbance most related to exposure to war zone traumatic stress. (Am J Psychiatry 1998; 155:929–933)
The DSM-IV criteria for posttraumatic stress disorder (PTSD) include two aspects of sleep disturbance: recurrent nightmares, listed in the reexperiencing cluster (criteria B), and sleep continuity disturbances, listed in the hyperarousal cluster (criteria D). However, a careful analysis as to whether sustained sleep disturbances in chronic PTSD are specifically related to the impact of exposure to traumatic stress or are a consequence of comorbid disorders has not occurred. This is because of insufficient measurement and control of comorbid conditions, the lack of careful measurement of traumatic exposure, and the use of treatment-seeking patients who may not reflect the general population with PTSD. This study addressed these problems by examining the role of exposure to trauma, nonsleep PTSD symptoms, and comorbid medical and psychiatric disorders in contributing to different domains of sleep disturbance in a nationally representative community sample of male Vietnam veterans and two comparison groups.
We analyzed the questionnaire items that address specific complaints about sleep from the National Vietnam Veterans Readjustment Study (1). That study was a major population-based study conducted in the late 1980s whose theater sample was selected to represent the entire group of 3.1 million men and women who served in the Vietnam theater. That study estimated the prevalence of current PTSD and other psychiatric disorders in Vietnam theater veterans in comparison to Vietnam era veterans and civilians. It remains the most comprehensive survey to date that examines the relationships among war zone exposure, PTSD, and postwar adjustment in multiple domains of psychosocial functioning. The goal of our study was to compare the frequency of nightmares and sleep continuity disturbances in combat veterans to that in Vietnam era veteran and civilian comparison subjects. We also sought to examine the role of combat exposure, comorbid psychiatric and medical disorder, and substance abuse in accounting for different domains of sleep disturbance.
Our hypothesis was that exposure to war zone trauma would be strongly linked to nightmares and less associated with sleep continuity disturbance. This hypothesis was guided by a published survey of 4,042 mono~zygotic and dizygotic Vietnam era veteran twins which found that combat exposure was highly correlated with reports of dreams and nightmares but only weakly associated with sleep onset and sleep maintenance insomnia (2). Further, we hypothesized that nightmares would be related predominantly to combat exposure and less related to comorbid psychiatric disorder, substance abuse, and chronic medical illness.
METHOD
Subjects
The National Vietnam Veterans Readjustment Study is a cross-sectional survey of three groups: theater veterans (who served in Vietnam and the airspace and waters surrounding Vietnam), era veterans (who served on active duty in the U.S. Armed Forces during the Vietnam era but not in the Vietnam theater), and age- and gender-matched civilian comparison subjects. The sample consisted of 1,200 male theater veterans, 412 male era veterans, and 450 male civilian comparison subjects (3). Subjects, identified by a national probability sampling strategy that drew from rural and urban areas in all 50 states, were interviewed in their homes through use of the National Survey of the Vietnam Generation (1). After complete description of the study to the subjects, written informed consent was obtained. The Vietnam era veteran and civilian comparison subjects were matched by age and ethnicity, and the two groups were weighted to the theater veteran population.
The demographic characteristics, prevalence of PTSD, and comorbid psychiatric diagnoses of the three study groups have been previously reported (3–5). Most subjects were middle-aged, were married, and had attended some college.
Measures
The data analyzed in this study come from responses to the National Survey of the Vietnam Generation, which included the military and civilian version of the Mississippi Scale for Combat-Related Posttraumatic Stress Disorder (6). The case definition for PTSD in this study of sleep was based on a cutoff score of 81 on the Mississippi scale minus the five items pertaining to sleep. This cutoff score yields a prevalence of PTSD of 15.0% in male theater veterans, which is closely comparable to the 15.2% adjusted prevalence reported in the National Vietnam Veterans Readjustment Study (3). We found that a PTSD case definition that used this criterion has a sensitivity of 72.7% and specificity of 83.6% when compared to the Structured Clinical Interview for DSM-III-R—Non-Patient Version (SCID-NP) (7). This case definition was chosen over the modified National Institute of Mental Health Diagnostic Interview Schedule (DIS) PTSD module (1, 8), which produced poor sensitivity when compared to the SCID-NP (9).
The dependent variables in this study were derived from the responses to the five sleep items in the military and civilian versions of the Mississippi scale. All responses were made on a 1–5-point Likert scale ranging from low to high severity of sleep disturbance. The difficulty in sleep onset variable was derived from the mean of the two items that inquire about difficulties with sleep onset: “I fall asleep easily at night” (reflected so that a score of 5 meant that the subject “never” fell asleep easily) and “I am afraid to go to sleep at night.” The Pearson correlation coefficient for these two items is 0.41 (p<0.0001, N=1,167). The measure for nightmares was derived from the two items that refer to frightening dreams: “I have nightmares of experiences in the military [civilian scale uses “in my past"] that really happened” and “My dreams at night are so real that I waken in a cold sweat and force myself to stay awake” (r=0.60, p<0.0001, N=1,167). The measure for sleep maintenance difficulty uses the single item, “I fall asleep, stay asleep and awaken only when the alarm goes off.”
The independent variables used to predict disturbances in the three sleep domains include combat exposure, lifetime history of major depression, alcohol abuse, substance abuse, panic disorder, mania, current major depression, and current medical comorbidity. The combat exposure factor was derived from items that comprise four dimensions of war zone trauma: exposure to combat, exposure to abusive violence, deprivation, and loss of meaning and control. A second-order principal components analysis showed that the four dimensions of exposure could be combined into a single index, ranging from –1.0 to 1.0 (1, 10). Veterans' self-reports of war zone exposure have been validated against studies of military records (1). Lifetime and current comorbid psychiatric disorders were diagnosed by the DIS (8). The factor for current medical comorbidity was based on responses to questions that asked if subjects had been bothered by any one of 32 chronic medical conditions (e.g., asthma, arthritis, diabetes, hypertension, kidney disease, seizures) within the past 12 months. These items were summed and recoded on a 5-point ordinal scale ranging from 0 to 4 (1, 11).
Statistical Analysis
The National Vietnam Veterans Readjustment Study data were obtained by a stratified, weighted sampling strategy that violates the simple random sampling assumptions of the common statistical packages. In this situation, common statistical procedures produce accurate point estimates (when properly weighted), but inaccurate (typically underestimated) variances, with the consequence of type I errors in statistical tests (12). Therefore, we performed all statistical tests by using SUDAAN (13), a software package for the analysis of complex survey data. SUDAAN uses a first-order Taylor series approximation to estimate variance for data sampled under complex survey designs. Both the raw and weighted sample sizes for each group are presented in this report.
Our sample varies slightly from the complete data set for the National Vietnam Veterans Readjustment Study (1) in that we have excluded 33 of the 1,200 theater veterans, one of the 412 era veterans, and 65 of the 450 civilian veterans because of missing data. The cases selected for the current study did not differ on demographic variables from the full National Vietnam Veterans Readjustment Study data set.
We constructed hierarchical regression models to determine the association between the outcome variable for nightmares and the following set of predictors: combat exposure, nonsleep PTSD symptoms, current and lifetime depression, alcohol and substance abuse, lifetime panic disorder, mania, and chronic medical illness.
RESULTS
Male theater veterans with current PTSD at the time when the National Vietnam Veterans Readjustment Study was conducted reported more disturbances in all three domains of sleep. Difficulties with falling asleep occurred with a frequency varying from “sometimes” to “very frequently” in 44.0% of combat veterans with PTSD, 5.5% of combat veterans without PTSD, 9.4% of era veterans, and 5.0% of civilian comparison subjects (χ2=126.0, df=24, p<0.0001) (figure 1). Difficulties staying asleep occurred sometimes or more frequently in 90.7% of combat veterans with PTSD, 62.5% of combat veterans without PTSD, 63.1% of era veterans, and 52.9% of civilian subjects (χ2=52.2, df=12, p<0.0001). Nightmares occurred sometimes or more frequently in 52.4% of combat veterans with PTSD, 4.8% of combat veterans without PTSD, 5.7% of era veterans, and 3.4% of civilian subjects (χ2=185.4, df=24, p<0.0001). Frequent or very frequent nightmares and difficulties with falling asleep were found exclusively in subjects with PTSD.
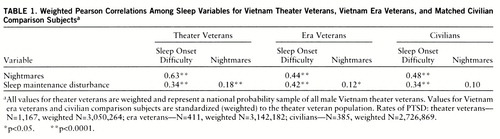
The correlations among the three domains of sleep in the three groups are shown in table 1. Not surprisingly, the sleep onset and nightmare variables were highly correlated in the Vietnam theater group given that one of the sleep onset items asks subjects if they are “afraid to fall asleep.” The Pearson correlation coefficient between the item “afraid to fall asleep” and nightmares was 0.63 (p<0.0001, N=1,167), compared to 0.48 between “fall asleep easily” and nightmares. We retained sleep onset and nightmares as separate variables because they are different facets of sleep disturbance that are distinguished by those with PTSD.
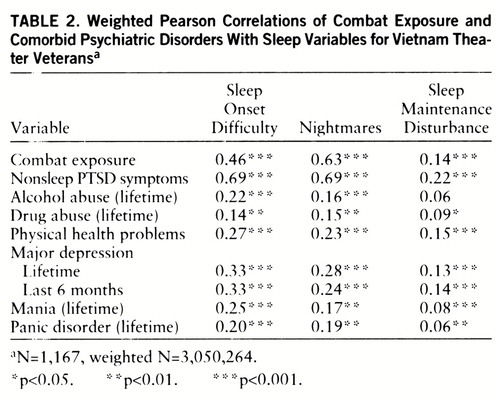
Table 2 shows the correlation matrix of the predictor and sleep variables in the combat veteran group. Of interest, combat exposure was strongly correlated with frequency of nightmares, moderately correlated with sleep onset insomnia, and weakly correlated with disrupted sleep maintenance.
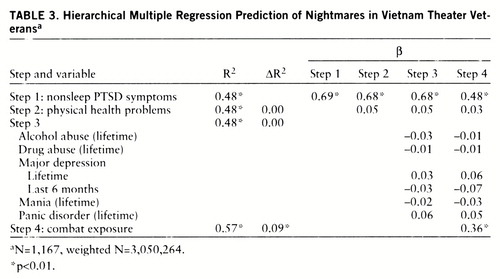
A hierarchical multiple regression model was developed to explain nightmares in Vietnam theater veterans. In this model (table 3), nonsleep PTSD symptoms accounted for 48% of the variance in nightmare frequency. Adding physical health problems, comorbid psychiatric disorder, and substance abuse to the model accounted for less than 1% of incremental variance. When an alternative model was developed in which physical health problems were entered first, followed by comorbid psychiatric disorder and substance abuse, these variables explained 5% and 11% of the variance, respectively. However, table 3 demonstrates that these variables do not contribute to unique variance not explained by the presence of nonsleep PTSD symptoms. The addition of the final predictor variable, combat exposure, yielded an additional 9% of the variance.
DISCUSSION
We found that for male veterans, frequent nightmares were virtually specific for those diagnosed with PTSD at the time of the survey and that combat exposure was highly associated with nightmares, moderately associated with sleep onset insomnia, and only weakly related to sleep maintenance insomnia. Our data are consistent with the results of the twin study (2), which showed that combat exposure was highly correlated with reports of dreams and nightmares and only weakly associated with sleep maintenance insomnia. This observation is also consistent with several other studies that show a low to moderate correlation between nightmares and other domains of sleep disturbance (14, 15). The nightmare appears to be the primary domain of sleep disturbance related to exposure to war zone traumatic stress. Further, our findings show that the frequency of nightmares has a strong relationship to level of exposure to war zone trauma even after accounting for nonsleep PTSD symptoms, comorbid psychiatric disorders, substance abuse, and general medical illness. In a manner similar to the acquisition of agoraphobia in individuals with panic disorder, we speculate that sleep onset insomnia in PTSD subjects is driven predominantly by sleep phobia resulting from the experience of frequent nightmares.
There are several limitations of this study that are a consequence of the cross-sectional design of the National Vietnam Veterans Readjustment Study, the retrospective measurement of combat exposure, and the lack of standardized measures of sleep disturbance. Recent prospective data from studies of Gulf War veterans suggest that the development of PTSD symptoms may amplify the recall of combat exposure (16). Thus, the correlation between combat exposure and nightmares might be influenced by this phenomenon. Further, the experience of frequent nightmares could contribute to an increase in the recall of traumatic experiences (17). The longitudinal course of sleep disturbances in PTSD awaits a future hypothetical study in which sleep in a population at high risk for exposure to trauma is studied at baseline and longitudinally after exposure to traumatic stress, after development of PTSD, and after the emergence of comorbidity.
The National Vietnam Veterans Readjustment Study did not use a standardized self-report measure of sleep quality. However, the domains of sleep analyzed here are easily identified and have been assessed with single items in validated instruments. For example, sleep onset, sleep maintenance, and disturbed dreams are assessed with single items in the Pittsburgh Sleep Quality Index, which has been shown to be highly reliable and valid when referenced to polysomnography (18).
The low correlation between our sleep continuity measure and current major depression may suggest that this single item is an insufficient measure. It is also possible that it reflects the fact that most depressed subjects in the National Vietnam Veterans Readjustment Study also had PTSD (11). Given that 90.7% of PTSD subjects reported sleep maintenance difficulties sometimes or more frequently, it is possible that the effects of depression were obscured. Several investigators have suggested that depression in the presence of PTSD may be biologically modified and hence may display different sleep characteristics (19, 20). Dow et al. (21) showed that subjects with both PTSD and major depression had shorter sleep latencies and higher sleep efficiency than subjects with depression alone. More studies of sleep in individuals with PTSD, with and without depression, are needed to clarify this issue.
Ross and colleagues (22) have reviewed the prevalence of nightmares in normal and clinical populations and have suggested that anxiety dreams are relatively specific to PTSD. Historically, nightmares have long been postulated as being a hallmark feature of responses to traumatic stress (23–27). Hartmann, in his studies of frequent nightmare sufferers, found that adult exposure to violent assault increased nightmare frequency; however, he was not able to find a history of early childhood trauma (28). He and others obtained data from frequent nightmare sufferers and suggested that these individuals were distrustful, schizoid, and alienated but not psychotic (29, 30). Kales et al. (30) also found that the onset of nightmares was preceded by “major life events.” The National Comorbidity Survey estimates that the lifetime prevalence of PTSD in the U.S. population is 7.8% (31). It is possible that prior surveys of frequent nightmare sufferers did not account for the presence of PTSD.
 |
 |
 |
Presented at the 149th annual meeting of the American Psychiatric Association, New York, May 4–9, 1996. Received March 19, 1997; revision received Oct. 8, 1997; accepted Dec. 22, 1997. From the Post Traumatic Stress Disorder Program, VA Medical Center, San Francisco, and the Department of Psychiatry, University of California San Francisco. Address reprint requests to Dr. Neylan, PTSD Program, Psychiatry Service 116P, VA Medical Center, 4150 Clement St., San Francisco, CA 94121. Supported in part by the Department of Veterans Affairs and the National Alliance for Research in Schizophrenia and Depression (Dr. Neylan).
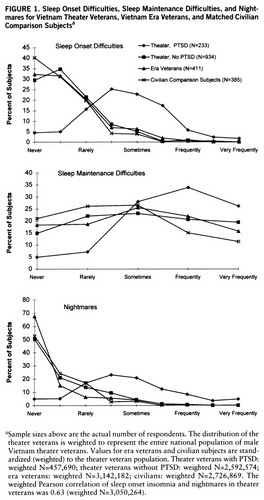
FIGURE 1. Sleep Onset Difficulties, Sleep Maintenance Difficulties, and Nightmares for Vietnam Theater Veterans, Vietnam Era Veterans, and Matched Civilian Comparison Subjectsa
aSample sizes above are the actual number of respondents. The distribution of the theater veterans is weighted to represent the entire national population of male Vietnam theater veterans. Values for era veterans and civilian subjects are standardized (weighted) to the theater veteran population. Theater veterans with PTSD: weighted N=457,690; theater veterans without PTSD: weighted N=2,592,574; era veterans: weighted N=3,142,182; civilians: weighted N=2,726,869. The weighted Pearson correlation of sleep onset insomnia and nightmares in theater veterans was 0.63 (weighted N=3,050,264).
1 Kulka RA, Schlenger WE, Fairbank JA, Hough RL, Jordan BK, Marmar CR, Weiss DS: Trauma and the Vietnam War Generation: Report of Findings From the National Vietnam Veterans Readjustment Study. New York, Brunner/Mazel, 1990Google Scholar
2 True WR, Rice J, Eisen SA, Heath AC, Goldberg J, Lyons MJ, Nowak J: A twin study of genetic and environmental contributions to liability for posttraumatic stress symptoms. Arch Gen Psychiatry 1993; 50:257–264Crossref, Medline, Google Scholar
3 Schlenger WE, Kulka RA, Fairbank JA, Hough RL, Jordan BK, Marmar CR, Weiss DS: The prevalence of post-traumatic stress disorder in the Vietnam generation: a multimethod, multisource assessment of psychiatric disorder. J Trauma Stress 1992; 5:333–363Crossref, Google Scholar
4 Weiss DS, Marmar CR, Schlenger WE, Fairbank JA, Jordan BK, Hough RL, Kulka RA: The prevalence of lifetime and partial post-traumatic stress disorder in Vietnam theater veterans. J Trauma Stress 1992; 5:365–376Crossref, Google Scholar
5 Jordan BK, Schlenger WE, Hough RL, Kulka RA, Weiss D, Fairbank JA, Marmar CR: Lifetime and current prevalence of specific psychiatric disorders among Vietnam veterans and controls. Arch Gen Psychiatry 1991; 48:207–215Crossref, Medline, Google Scholar
6 Keane TM, Caddell JM, Taylor KL: Mississippi Scale for Combat-Related Posttraumatic Stress Disorder: three studies in reliability and validity. J Consult Clin Psychol 1988; 56:85–90Crossref, Medline, Google Scholar
7 Spitzer RL, Williams JBW, Gibbon M, First MB: Structured Clinical Interview for DSM-III-R—Non-Patient Version (SCID-NP). New York, New York State Psychiatric Institute, Biometrics Research, 1987Google Scholar
8 Robins LN, Helzer JE, Croughan J, Ratcliff KS: The National Institute of Mental Health Diagnostic Interview Schedule: its history, characteristics, and validity. Arch Gen Psychiatry 1981; 38:381–389Crossref, Medline, Google Scholar
9 Kulka RA, Schlenger WE, Fairbank JA, Jordan BK, Hough RL, Marmar CR, Weiss DS: Assessment of posttraumatic stress disorder in the community: prospects and pitfalls from recent studies of Vietnam veterans. Psychol Assess 1991; 3:547–560Crossref, Google Scholar
10 Marmar CR, Weiss DS, Schlenger WE, Fairbank JA, Jordan BK, Kulka RA, Hough RL: Peritraumatic dissociation and posttraumatic stress in male Vietnam theater veterans. Am J Psychiatry 1994; 151:902–907Link, Google Scholar
11 Zatzick DF, Marmar CR, Weiss DS, Browner WS, Metzler TJ, Golding JM, Stewart A, Schlenger WE, Wells KB: Posttraumatic stress disorder and functioning and quality of life outcomes in a nationally representative sample of male Vietnam veterans. Am J Psychiatry 1997; 154:1690–1695Link, Google Scholar
12 Lee ES, Forthofer RN, Lorimor RJ: Analysis of complex sample survey data: problems and strategies. Sociological Methods and Res 1986; 15(1–2):69–100Google Scholar
13 Shah BV, Folsom RE, Lavange LM, Boyle KE, Wheeles SC, Williams RL: Statistical Methods and Mathematical Algorithms in SUDAAN. Research Triangle Park, NC, Research Triangle Institute, 1993Google Scholar
14 Coren S: The prevalence of self-reported sleep disturbances in young adults. Int J Neurosci 1994; 79:67–73Crossref, Medline, Google Scholar
15 Krakow B, Tandberg D, Scriggins L, Barey M: A controlled comparison of self-rated sleep complaints in acute and chronic nightmare sufferers. J Nerv Ment Dis 1995; 183:623–627Crossref, Medline, Google Scholar
16 Southwick SM, Morgan CA III, Nicolaou AL, Charney DS: Consistency of memory for combat-related traumatic events in veterans of Operation Desert Storm. Am J Psychiatry 1997; 154:173–177Link, Google Scholar
17 Kramer M, Kinney L: Vulnerability to developing delayed post traumatic stress disorder: combat experience and psychological status (abstract). Sleep Res 1985; 14:131Google Scholar
18 Buysse DJ, Reynolds CF III, Monk TH, Berman SR, Kupfer DJ: The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res 1989; 28:193–213Crossref, Medline, Google Scholar
19 Yehuda R, McFarlane AC: Conflict between current knowledge about posttraumatic stress disorder and its original conceptual basis. Am J Psychiatry 1995; 152:1705–1713Link, Google Scholar
20 Woodward SH: Neurobiological perspectives on sleep in post-traumatic stress disorder, in Neurobiological and Clinical Consequences of Stress: From Normal Adaptation to PTSD. Edited by Friedman MJ, Charney DS, Deutch AY. Philadelphia, Lippincott-Raven, 1995, pp 315–333Google Scholar
21 Dow BM, Kelsoe JR Jr, Gillin JC: Sleep and dreams in Vietnam PTSD and depression. Biol Psychiatry 1996; 39:42–50Crossref, Medline, Google Scholar
22 Ross RJ, Ball WA, Sullivan KA, Caroff SN: Sleep disturbance as the hallmark of posttraumatic stress disorder. Am J Psychiatry 1989; 146:697–707Link, Google Scholar
23 Freud S: Beyond the pleasure principle (1920), in Complete Psychological Works, standard ed, vol 18. London, Hogarth Press, 1955, pp 7–64Google Scholar
24 Kardiner A, Spiegel H: War Stress and Neurotic Illness. New York, Paul B Hoeber, 1947Google Scholar
25 Horowitz MJ: Stress Response Syndromes. New York, Jason Aronson, 1976Google Scholar
26 Brett EA, Ostroff R: Imagery and posttraumatic stress disorder: an overview. Am J Psychiatry 1985; 142:417–424Link, Google Scholar
27 Kramer M, Kinney L: Sleep patterns in trauma victims with disturbed dreaming. Psychiatr J Univ Ottawa 1988; 13:12–16Medline, Google Scholar
28 Hartmann E: The Nightmare: The Psychology and Biology of Terrifying Dreams. New York, Basic Books, 1984Google Scholar
29 Hartmann E, Russ D, van der Kolk B, Falke R, Oldfield M: A preliminary study of the personality of the nightmare sufferer: relationship to schizophrenia and creativity? Am J Psychiatry 1981; 138:794–797Google Scholar
30 Kales A, Soldatos CR, Caldwell AB, Charney DS, Kales JD, Markel D, Cadieux R: Nightmares: clinical characteristics and personality patterns. Am J Psychiatry 1980; 137:1197–1201Link, Google Scholar
31 Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB: Posttraumatic stress disorder in the National Comorbidity Survey. Arch General Psychiatry 1995; 52:1048–1060Crossref, Medline, Google Scholar



