What Happens to Anxiety Levels on Giving Up Smoking?
Abstract
OBJECTIVE: DSM-IV lists increased anxiety as a nicotine withdrawal symptom. Increased anxiety has been reported to follow smoking cessation in most but not all studies. Indeed, there is some evidence for a reduction in anxiety, compared with precessation levels, after the first few weeks of abstinence. This study reports data from 101 smokers who attempted to stop smoking and who satisfied DSM-III-R criteria for nicotine dependence. METHOD: Unlike most studies in this area, a strict criterion of lapse-free abstinence was adopted. It is argued that lapses during an attempt at cessation may underlie a transient increase in anxiety. Anxiety was measured both by a single rating typical in withdrawal studies and by the State-Trait Anxiety Inventory—State Form X. Patients were rated 2 weeks and 1 week before cessation, immediately before cessation, 24 hours after cessation, and 1, 2, 3, and 4 weeks after cessation. RESULTS: Seventy patients were abstinent for the 4-week follow-up period. There was no evidence of an increase in anxiety following smoking cessation. However, there was a significant decrease in anxiety from the first week of abstinence. CONCLUSIONS: The results weaken the view that increased anxiety is a robust and central element of the nicotine withdrawal syndrome and suggest that giving up smoking is quite rapidly followed by a reduction in anxiety that may reflect removal of an anxiogenic agent, nicotine. (Am J Psychiatry 1997; 154:1589–1592)
DSM-IV includes increased anxiety as one of the nicotine withdrawal symptoms. What happens to anxiety following smoking cessation is of theoretical and practical significance. While most studies have reported a transient increase in anxiety (1), some have not (2). Further, some studies appear to show a decrease in anxiety below precessation levels after a few weeks of abstinence (3). The present study reports findings on changes in anxiety levels before, and up to 4 weeks after, smoking cessation in a smokers' clinic.
One feature of existing studies leaves room for doubt about what happens to anxiety when people abstain from smoking. Almost all studies reported in the literature have included data from subjects who had occasional cigarettes during the “abstinence” period. In most cases it is reported that this made no difference to the results, but no details are given, and the power to detect differences between subjects with minor lapses to smoking and those who were totally abstinent would have been low. It remains possible, therefore, that average anxiety levels during the abstinence period might have been inflated by smokers worried that they had not been able to maintain total abstinence. Even when smokers do not report minor lapses, it is possible that lapses may have occurred and gone undetected. This is because most withdrawal studies have involved nicotine replacement therapy, and so biochemical validation of abstinence has had to rely on expired air carbon monoxide concentrations. These concentrations would not normally reveal occasional cigarette smoking because of expired air carbon monoxide's short half-life and the possibility of low levels of exposure from environmental sources.
The issue is of practical significance. If anxiety increases after smoking cessation, one might expect interventions that reduce anxiety to help smokers who are trying to quit. In fact, this has not been the case with drugs tried thus far (4). The issue is also important from a theoretical point of view. Many smokers and some researchers believe that smoking has a calming effect (5, 6). However, the evidence is inconsistent. For example, Perkins et al. (7) reported that nicotine administration increased subjective tension compared with a placebo, even among smokers. Moreover, population studies reveal that current smokers report higher anxiety levels than individuals who have never smoked or ex-smokers (8). It has also been reported that once the acute withdrawal phase is over, perceived stress (9) declines to below precessation levels. Several studies have shown that mean anxiety levels drop below precessation levels after several weeks (3). However, the reports did not include significance tests to determine whether the differences were greater than would be expected by chance. It is also possible, however, that smokers have a constitutionally high level of anxiety that is reduced by smoking, albeit not to the level found in nonsmokers. Under this hypothesis, smokers would have even higher anxiety levels if they did not smoke, and those who succeed in quitting are people with low levels of chronic anxiety who do not need the anxiolytic effect of smoking. Examining changes in anxiety levels on giving up smoking could help to clarify this issue.
Key features of the present study were as follows: the subjects were undergoing cigarette withdrawal without any active medication; the group size was large by comparison with previous studies of this kind; a criterion of lapse-free abstinence was adopted; abstinence was verified by saliva cotinine, which is well suited to detecting minor lapses; anxiety was measured by the Mood and Physical Symptoms Scale (MPSS), previously used in tobacco withdrawal studies (10), and the State-Trait Anxiety Inventory—State Form X (STAI) (11); anxiety was measured for 2 weeks before abstinence and for 4 weeks after it; abstinence rates were high, leading to few dropouts; and the subjects all satisfied DSM-III-R criteria for nicotine dependence.
Another issue addressed in the present study concerned the validity of the MPSS anxiety rating. This has been used extensively in smoking research but has not, to our knowledge, been validated against multi-item anxiety measures more often used in psychological research. We examined correlations between MPSS anxiety ratings and Spielberger STAI scores at each time point.
Other papers arising from the present study are a report on drug efficacy (12), a paper on the effects of abstinence on physical markers of health (unpublished), and a paper examining predictors and sequelae of nicotine withdrawal symptoms (unpublished).
Thus, the main question addressed in the present report is how do anxiety levels change during lapse-free abstinence from smoking? A secondary issue addressed is how does the single anxiety rating in the MPSS compare with the 20-item Spielberger STAI?
METHOD
Data were collected in the course of a double-blind, placebo-controlled study. Subjects were randomly assigned to either the 5-hydroxytryptamine antagonist ondansetron or to a placebo with group treatment. There was no evidence of drug effects on any of the measures. Full details of the trial are given elsewhere (12). Psychological and physical measures were obtained at clinic sessions according to the following schedule: session 1, 2 weeks before cessation; session 2, 1 week before cessation; session 3, just before cessation; session 4, 24 hours after cessation; session 5, 1 week after cessation; session 6, 2 weeks after cessation; session 7, 3 weeks after cessation; session 8, 4 weeks after cessation.
Subjects
Subjects were recruited by advertisement and referral by family practitioners. Eligibility was assessed first by telephone interview and then in a face-to-face interview with a physician. To be eligible for the study the smokers had to have smoked at least 15 cigarettes per day for at least 5 years, have been in good health and not be taking any prescribed medication apart from contraceptive pills or antibiotics, be 18–65 years old (mean age=40), have no diagnosed psychiatric illness, not be serious abusers of alcohol or drugs, and not be taking any other antismoking preparation. They all fulfilled DSM-III-R criteria for nicotine dependence. Forty percent were men. They averaged 25 cigarettes per day (SD=9). Their baseline saliva cotinine level averaged 416 ng/ml (SD=165). A total of 70 subjects maintained abstinence for the full duration of the study and formed the basis for the main analyses. After complete description of the study to the subjects, written informed consent was obtained.
Procedure and Assessments
At the first session subjects completed the MPSS (10). They were asked to rate how they had been feeling over the past 24 hours on a number of dimensions, including “anxious/tense.” The ratings were made on a 5-point scale (1=not at all, 5=extremely). Subjects also completed the STAI (11). Saliva samples were taken to be analyzed for cotinine in order to obtain an index of subjects' nicotine intake in the preceding days. They were instructed to continue smoking as normal until the next visit. This and all subsequent sessions were conducted in the early evening.
When the subjects returned for their second visit, they completed the MPSS and the STAI. Their expired air carbon monoxide concentrations were measured. The third visit followed a pattern similar to that of the second, except that the subjects were instructed that from this visit onward, they should abstain completely from all tobacco products and return for the next visit on the following day so that data could be collected after 24-hour abstinence. The fourth visit was the first at which subjects should have been abstinent. In addition to the measures taken during preceding visits, they were asked whether they had managed to maintain abstinence since the last visit. Saliva samples were not obtained at this visit because significant residual levels of cotinine from the previous day's smoking would have precluded their use as a means of verifying claims of abstinence. For this visit, claims of abstinence were validated by expired air carbon monoxide levels of less than 7 parts per million above ambient. Data similar to those collected in the fourth visit, plus saliva cotinine levels, were collected in the visits taking place 1, 2, 3, and 4 weeks after the designated start of abstinence. Subjects were classified as abstainers if they reported no smoking at all since the quit date and if in visits after 24 hours, their saliva cotinine level was below 20 ng/ml.
Data Analysis
Changes over time in MPSS anxiety and STAI scores were tested by means of repeated measures analyses of variance (ANOVAs). Changes from the average of the three baseline measures in each postcessation visit were assessed by post hoc comparison with Bonferroni adjustment. MPSS ratings and STAI scores, and anxiety ratings on successive visits, were compared by means of Pearson correlations.
RESULTS
Of 101 subjects, 96 were abstinent at 24 hours, 78 were abstinent at 1 week, 72 were abstinent at 2 weeks, and 70 were abstinent for the whole 4-week follow-up period.
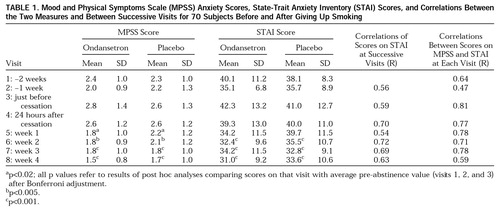
Table 1 shows the mean MPSS anxiety ratings and mean STAI scores. According to both measures anxiety levels decreased at the second visit and then increased again at the third visit, just before cessation. Anxiety levels then showed no change up to 24 hours after abstinence, following which they decreased significantly. Week 2, 3, and 4 scores on both MPSS and STAI were significantly lower than the precessation baseline scores. Figure 1 shows the changes graphically. The mean baseline STAI scores were similar to those of nonpatient populations given in the STAI manual (11).
Table 1 also shows moderate to high correlations between anxiety levels in successive visits including the immediate precessation and postcessation visits (R=0.70). Thus, it was largely the same individuals who were anxious immediately before cessation as after cessation. There were also high correlations between the MPSS anxiety ratings and STAI scores at each time point. Figure 1 shows that the mean MPSS ratings and STAI scores were almost identical in proportion to the full-scale range at every time point.
To check that there were no differences in baseline anxiety levels between subjects included in our analysis and those who relapsed during the study, we carried out a t test comparing these groups. The mean baseline STAI score (averaged over the three pre-abstinence visits) for subjects who remained abstinent was 38.7 (SD=8.5). The mean STAI score for those who relapsed at some point in the 4 weeks of treatment was 39.9 (SD=9.8). The difference between the groups was not significant (t=0.63, df=99). To check for differences in the change in STAI score over the first 24 hours between those who remained abstinent for the whole 4 weeks of treatment and those who relapsed after 24 hours, we carried out an ANOVA with total abstainers after 24 hours versus relapsers as a between-groups factor and baseline score versus 24 hours' abstinence score as a within-groups factor. The interaction (equivalent to a between-groups t test on the change score) was not significant (F=1.9, df=1,99).
DISCUSSION
There was no increase in anxiety on smoking cessation; indeed, there was a significant decrease from baseline by week 2. The MPSS anxiety ratings were highly correlated with STAI scores and were at a similar level proportionate to the range of values that could be obtained.
The simplest interpretation of the findings is that giving up smoking does not increase anxiety but, rather, decreases it. A second interpretation is that smoking cessation does increase anxiety, but the increase in this case was masked by a precessation rise in anticipation of smoking cessation. A further possible interpretation is that smoking cessation increases anxiety, but by chance this failed to emerge in the present study. It is also possible that there is an increase in anxiety, but the smoking cessation program used in this study counteracted it. Finally, any increase in anxiety may be present only in anxiety-provoking situations and would therefore not have been detected.
In support of the first interpretation is the large group, use of dependent smokers, multiple baseline measures, and strict criterion of lapse-free abstinence. Against it is the fact that most studies in the literature find a transient increase in anxiety following smoking cessation, albeit with a more lax criterion of abstinence.
Against the second interpretation is the fact that it is not parsimonious to postulate two highly correlated (table 1) yet different sources of anxiety operating within 24 hours. Against the third interpretation is the fact that the power to detect an increase in anxiety of the size normally found with withdrawal studies was greater than 90%, that the same results were obtained with MPSS rating of anxiety and the STAI, and that the absolute levels of anxiety at their highest were still in the lower half of the MPSS and STAI scale ranges.
With regard to the fourth possibility, the treatment program is unlikely to have affected anxiety levels. The drug had no effect on anxiety, other withdrawal ratings, or abstinence (12); and the sessions focused on group discussion of abstinence and had no relaxation or stress management components (13). Some of the studies reporting an increase in anxiety used more stress-focused treatments. Moreover, this interpretation could not explain the difference between the present study and studies that reported an increase in anxiety and that also used smokers' clinic patients.
Finally, while the STAI asked about the feeling “at this moment,” the MPSS, which obtained the same result, covered the preceding 24 hours. If there was an increase in situational anxiety, it should have been detected.
The possibility that we did not detect an increase in anxiety because this only affects more dependent smokers can be ruled out. Our group was restricted to patients who fulfilled DSM-III-R criteria for nicotine dependence. Moreover, their baseline saliva cotinine concentrations were higher than those for the average smoker.
It is important to note that our group excluded subjects with current psychiatric morbidity. It is possible that such patients may experience a deterioration when they stop smoking. However, it is also possible that they would experience an even greater decrease in anxiety than our group did, given that they would be starting from a higher baseline. From our analysis, studies reporting an increase in anxiety in psychiatric samples would, like other studies, have to show that they had excluded any subjects with minor lapses to smoking before claiming increased anxiety to be a withdrawal symptom.
Thus, although we cannot rule out the possibility that the failure to find an increase in anxiety on smoking cessation was an aberration or the possibility that there was an increase that was masked by precessation worries, the size of the study, the care with which anxiety was measured, the high abstinence rate, and the strict criterion of abstinence all mean that our findings must be considered seriously and that there is a question mark over whether increased anxiety should be considered a core nicotine withdrawal symptom and whether it should be featured in DSM.
The finding of decreased anxiety after 4 weeks of abstinence is more in line with previous research and supports the view that smoking is chronically anxiogenic rather than anxiolytic. That is, averaged over a day, smoking leads to higher anxiety levels. The high lapse-free abstinence rate strengthens this view, as against the view that smokers use cigarettes to manage constitutionally high levels of anxiety and that the small proportion of smokers who manage to quit at any one attempt are those who have less need of this self-medication. It remains a possibility that the smokers became less anxious as they felt better about themselves and had a growing confidence that they could become nonsmokers. In that case one would expect the effect to wear off after a few weeks and anxiety levels to increase. However, there is clear evidence that long-term ex-smokers report lower stress levels and less mood disturbance than current smokers (9). Thus, the present findings, in consort with previous research, lend support to the view that smoking leads to chronically increased anxiety and that giving up smoking improves the situation.
With regard to the comparison between the MPSS anxiety rating and the Spielberger scale, it appears that both give equivalent results in this context. Thus, for smoking cessation research, the added value of the Spielberger scale is limited.
In conclusion, the results show that a single anxiety rating performs similarly to the 20-item Spielberger scale in this context. They call into question the robustness of the finding of increased anxiety following smoking cessation, and they support the view that anxiety levels drop below precessation values within 4 weeks of abstinence.
 |
Received May 24, 1996; revision received March 10, 1997; accepted April 25, 1997. From St. George's Hospital Medical School. Address reprint requests to Dr. West, St. George's Hospital Medical School, University of London, Cranmer Terrace, London SW17 0RE, England. The authors thank Margaret Reuben, Teresa Webb, and Julia Wilson for help with data collection.
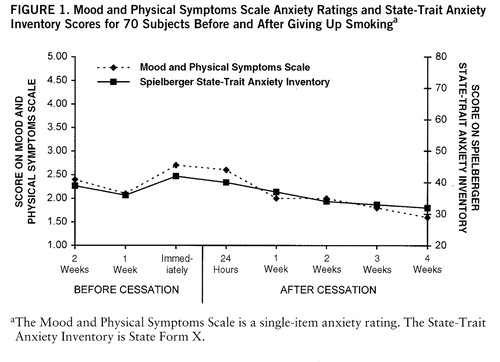
FIGURE 1. Mood and Physical Symptoms Scale Anxiety Ratings and State-Trait Anxiety Inventory Scores for 70 Subjects Before and After Giving Up Smokinga
aThe Mood and Physical Symptoms Scale is a single-item anxiety rating. The State-Trait Anxiety Inventory is State Form X.
1. Hughes J, Higgins S, Bickel W: Nicotine withdrawal versus other drug withdrawal syndromes: similarities and dissimilarities. Addiction 1994; 89:1461–1470Google Scholar
2. Hughes JR, Higgins ST, Hatsukami D: Effects of abstinence from tobacco: a critical review, in Research Advances in Alcohol and Drug Problems, vol 10. Edited by Kozlowski LT, Annis HM, Cappell HD, Glaser FB, Goodstadt MS, Israel Y, Kalant H, Sellers EM, Vingilis ER. New York, Plenum, 1990, pp 317–398Google Scholar
3. Gross J, Stitzer M: Nicotine replacement: ten-week effects on tobacco withdrawal symptoms. Psychopharmacology (Berl) 1989; 98:334–341Crossref, Medline, Google Scholar
4. Hughes J: Non-nicotine pharmacotherapies for smoking. J Drug Development 1994; 6:197–203Google Scholar
5. Hall S, Munoz R, Reus V, Sees K: Nicotine, negative affect and depression. J Consult Clin Psychol 1993; 61:761–767Crossref, Medline, Google Scholar
6. Russell M, Peto J, Patel U: The classification of smoking by factorial structure of motives. J R Statistical Soc Series A 1974; 137:313–346Crossref, Google Scholar
7. Perkins KA, Sexton JE, Stiller RL, Fonte C, DiMarco A, Goettler J, Scierka A: Subjective and cardiovascular responses to nicotine combined with caffeine during rest and casual activity. Psychopharmacology (Berl) 1994; 113:438–444Crossref, Medline, Google Scholar
8. Jarvis M: A profile of tobacco smoking. Addiction 1994; 89:1371–1376Google Scholar
9. Cohen S, Lichtenstein E: Perceived stress, quitting smoking, and smoking relapse. Health Psychol 1990; 9:466–478Crossref, Medline, Google Scholar
10. West R, Russell M: Pre-abstinence smoke intake and smoking motivation as predictors of severity of cigarette withdrawal symptoms. Psychopharmacology (Berl) 1985; 87:334–336Crossref, Medline, Google Scholar
11. Spielberger CD, Gorsuch RL, Lushene RD: STAI Manual. Palo Alto, Calif, Consulting Psychologists Press, 1970Google Scholar
12. West R, Hajek P: Randomised controlled trial of ondansetron in smoking cessation. Psychopharmacology (Berl) 1996; 126:95–96Crossref, Medline, Google Scholar
13. Hajek P: Helping smokers to overcome tobacco withdrawal: background and practice of withdrawal-oriented therapy, in Interventions for Smokers: An International Perspective. Edited by Richmond R, New York, Wilkins, 1994, pp 29–46Google Scholar



