PET Evidence That Loxapine Is an Equipotent Blocker of 5-HT2 and D2 Receptors: Implications for the Therapeutics of Schizophrenia
Abstract
OBJECTIVE: Loxapine, a dibenzoxazepine antipsychotic, is closely related to clozapine and shares clozapine's high affinity for binding to serotonin 5-HT2 and dopamine D4 receptors. The purpose of this study was to document loxapine's 5-HT2 and D2 receptor occupancy in vivo in patients with psychoses. METHOD: Ten patients who were taking loxapine (10–100 mg/day) had their D2 and 5-HT2 receptors assessed by means of positron emission tomography with [11C]raclopride and [18F]setoperone, respectively. RESULTS: The D2 receptor occupancy ranged from 43% to 90% 5-HT2 occupancy varied from 27% to near saturation. Statistical comparison of the results showed that loxapine was equipotent in blocking 5-HT2 and D2 receptors. CONCLUSIONS: Loxapine differs from typical neuroleptics in demonstrating a high degree of 5-HT2 receptor occupancy. However, it is not “atypical” like clozapine and risperidone, since its 5-HT2 occupancy is not higher than its D2 occupancy. The results demonstrate that a high level of 5-HT2 occupancy is not a sufficient condition for atypicality. If atypical antispychotic action is predicated on a combination of 5-HT2 and D2 effects, then it requires >80% 5-HT2 occupancy in conjunction with <80% D2 occupancy. (Am J Psychiatry 1997; 154:1525–1529)
The clinical efficacy of typical neuroleptics, as well as their side effects, has usually been understood in terms of their dopamine D2 receptor activity. It is being increasingly realized that treatment may be optimized further by combining a high level of serotonin 5-HT2 receptor blockade with low to modest levels of dopamine D2 receptor blockade (1–3). The combination of 5-HT2 with D2 blockade provides antipsychotic treatment in which patients have lesser extrapyramidal side effects, greater improvement in negative symptoms, and perhaps even better improvement in positive symptoms in refractory cases (3, 4). It has also been claimed that the superior efficacy of clozapine may actually result from its high level of D4 blockade in combination with low to modest D2 blockade (5). Thus, current theories point toward a beneficial effect of high 5-HT2 and high D4 blockade in combination with low to modest D2 blockade.
Loxapine has traditionally been considered a typical neuroleptic, but its pharmacological properties are rather atypical. Several in vitro studies (1, 6, 7) have shown that its 5-HT2 affinity is higher than its D2 affinity. While the degree to which its 5-HT2 affinity exceeds its D2 occupancy depends on the particular technique and study (e.g., Meltzer et al. [1] reported a 5-HT2/D2 affinity ratio of 2.6; Leysen et al. [7], 6.8; and Singh et al. [6], 3.9), all reports agree that loxapine has a higher in vitro affinity for 5-HT2 receptors than for D2 receptors. Furthermore, in vivo animal studies show that loxapine, like clozapine but unlike other typical neuroleptics, down-regulates 5-HT2 receptors in the prefrontal cortex, an outcome attributed to its prominent 5-HT2 blockade (8, 9). At the same time, loxapine is a very prominent D4 antagonist, its D4 affinity is higher than that of clozapine, and even its D4/D2 affinity ratio is comparable to that of clozapine (6, 10).
However, there are significant differences between data from in vitro studies and the actual behavior of these drugs in humans. First, the affinity of a drug as determined in vitro varies with the assay and the conditions under which it is ascertained, and these may lead to widely varying results between laboratories (10). Second, in vitro, one usually measures the efficacy of the parent drug itself. However, in vivo, the drug is metabolized, and the metabolite may have a pharmacological profile different from that of the parent compound and may reach a concentration higher than that of the parent drug. Third, two drugs with equal affinity in vitro may not penetrate the brain in the same fashion and therefore may give rise to different levels of occupancy in vivo. Finally, the net functional effect of a drug can be determined only in the context of clinical doses. A drug may have a higher relative affinity for 5-HT2 than for D2 receptors; however, if it is used at doses at which both of the systems are saturated, there may be no functional difference in the relative 5-HT2 and D2 blockades (3).
Given evidence for the in vitro atypicality of loxapine, we were interested in documenting its in vivo receptor effects. We present here the results of the first systematic positron emission tomography (PET) study of the 5-HT2 and D2 occupancy profile of loxapine in humans.
METHOD
Ten patients (eight men and two women) aged 21–38 years participated in this study conducted in the Schizophrenia Division of The Clarke Institute of Psychiatry, Toronto. Patients were enrolled if they 1) had been taking a fixed dose of loxapine for 7 days or more; 2) had a DSM-III-R diagnosis of schizophrenia, delusional disorder (subject 2 in table 1), or brief reactive psychosis (subject 5); 3) had not received a depot neuroleptic in the last 6 months; 4) were not taking any concurrent psychotropic medication except a benzodiazepine or an antiparkinsonian agent; and 5) had no concurrent substance abuse or dependence. Written consent was obtained from each subject on forms approved by the University of Toronto Human Subjects Review Committee. The main purpose of the study was to obtain the in vivo 5-HT2/D2 profile of loxapine in patients, for which this cross-sectional design is sufficient. However, because of the small size of the study group, the inadequate control over the treatment, and the fact that the patients were in various degrees of remission at the time of scanning, the design was limited in its ability to obtain reliable associations between receptor occupancy and clinical outcome. This is an important limitation of the study.
The 5-HT2 and D2 receptor status was assessed with the use of PET imaging with [18F]setoperone and [11C]raclopride, respectively, on a single day, after the patients had been taking a stable dose of loxapine for at least 7 days. The scans for dopamine D2 receptors were done 11–13 hours after the nightly dose of loxapine. The 5-HT2 receptor scans followed the D2 scans and were done 13–15 hours after the nightly dose. D2 receptor scans preceded 5-HT2 receptor measurements because the long half-life of [18F]setoperone would confound any subsequent [11C]raclopride studies. Both of the PET scans were obtained with a GEMS 2048-15B head-only scanner.
Seven of the patients (patients 1–7, table 1) were part of an earlier brief report on the effects of loxapine on dopamine D2 receptors (11). The PET scans for D2 receptors were obtained after the injection of 10 mCi (mean=10.02 mCi, SD=0.55) of high specific activity [11C]raclopride (300–1600 Ci/mmol) according to a bolus-plus-infusion protocol described in detail elsewhere (11, 12). Striatal and cerebellar regions of interest were drawn on two contiguous PET slices on a composite PET image with reference to a coregistered magnetic resonance imaging (MRI) scan (GE Signa 1.5-T scanner, T2-weighted spin-echo sequence coregistered to the PET scan with the use of a surface-matching algorithm as implemented in ANALYZE 7.0 [Biomedical Imaging Resource, Rochester, Minn.]). To estimate the dopamine D2 receptor binding potential (D2BP) (which represents the total number of receptors available to the ligand, [11C]raclopride, divided by the affinity of the ligand for the D2 receptors [Bmax/Kd]), we used a two-tissue compartment model that partitions the decay-corrected time activity counts obtained from the striatum into those which are specifically bound to the D2 receptor and those which reflect the free radioligand and nonspecific binding (13). The counts from the cerebellum were used as an estimate of the free and nonspecific binding in the striatum. The details of this method and its application to the determination of D2 receptor occupancy have been described earlier (12). This method yields a test-retest standard deviation of 6% and has been standardized to have an interrater and intrarater intraclass correlation coefficient, type III (ICC-III) greater than 0.95.
To estimate receptor occupancy we used an age-corrected baseline value derived from a pool of 12 neuroleptic-naive patients with DSM-III-R-defined schizophrenia. Loxapine-induced D2 receptor occupancy was calculated as (D2BPBas–D2BPLox)/(D2BPBas), where D2BPBas is the age-corrected D2BP baseline, and D2BPLox is the D2BP for the dopamine D2 receptors in patients taking loxapine (11). The absence of a subject's own baseline values introduces a potential error; the error is expected to vary from 0% to 9% for patients with 50% occupancy and from 0% to 4% for patients who have 80% occupancy (11).
The 5-HT2 scans were obtained by using a bolus injection of 5 mCi (mean=5.05 mCi, SD=0.22) of [18F]setoperone according to the method developed and standardized by Blin et al. (14, 15). The [18F]setoperone was synthesized with a modification of methods described by Crouzel et al. (16). The 5-HT2 occupancy was determined in the prefrontal cortex. Since there was no significant difference across the two hemispheres, the data were pooled. The prefrontal region of interest was drawn on the [18F]setoperone scan with reference to a coregistered MRI scan, as described above. Five contiguous PET slices that showed the prefrontal cortex were included in the region of interest. The cerebellar region of interest was drawn on two contiguous slices.
To obtain an index of the 5-HT2 receptors, we chose the ratio of frontal to cerebellar activity over the 65- to 90-minute time period. The cerebellum is practically devoid of 5-HT2 receptors (17), and studies in baboons as well as humans report no displaceable [18F]setoperone binding in this region (14, 15, 18). It can be shown that at a time when the binding of the radioligand is at pseudo-equilibrium, the prefrontal/cerebellum ratio represents (1+k3/k4), or (1+Bmax/Kd); k3 and k4 refer to rate constants that reflect ligand transfer between the free and specific compartments in a three-compartment model (19). While this method does not permit an independent determination of Bmax and Kd, it provides the binding potential for 5-HT2 receptors (5-HT2BP), an index that can be validly used for semiquantitative and within-study comparisons (19). The details of this method have been described elsewhere (20), and as operationalized in our laboratory, it yields an average test-retest deviation of 6%–7% and an acceptably high interrater reliability (ICC-III >0.95 for all regions) (20).
Since these patients were already being treated, it was not possible to measure their baseline 5-HT2BP. In the absence of this baseline, we used the age-corrected 5-HT2BP obtained from 26 age-matched normal control subjects. Controlling for age effects is necessary, since age causes a definite decline in the number of 5-HT2 receptors (21), as was observed in this group of normal control subjects and has been observed in patients with schizophrenia (22). The use of normal control subjects is justified by the fact that two studies that have systematically compared 5-HT2 receptors in schizophrenic subjects versus normal subjects have reported no statistically significant difference (22, 23). The loxapine-induced 5-HT2 occupancy for a given subject was calculated as 100×(5-HT2BPBas–5-HT2BPLox)/(5-HT2BPBas), where 5-HT2BPBas is the age-corrected 5-HT2BP for the drug-free state (obtained from the pool of normal subjects), and 5-HT2BPLox is the measured 5-HT2BP for patients taking loxapine.
The receptor occupancy data were related to plasma levels of loxapine and its metabolites 7-hydroxyloxapine and 8-hydroxyloxapine, which were ascertained at the time of each scan. The plasma levels were assessed by means of a previously standardized procedure in which high-performance liquid chromatography was used (24). Plasma concentrations were estimated by comparing peak height ratios of each analyte with the internal standard and standard curves and with quality control samples analyzed during the same analytical run.
The relationship between an antagonist drug and the receptors that it occupies can be defined by the equation %ROcc=DConc/(ED50+DConc), where %ROcc is the percentage of the available receptors that are occupied by the drug, DConc is the concentration of the drug, and ED50 is a constant that equals the level of the drug required to occupy 50% of the available receptors. DConc should represent the concentration of the drug in the synapse. Since there is no easy way to measure the synaptic concentration of the drug in patients, one can use dose and plasma level as functional surrogates. However, it should be kept in mind that even plasma levels reflect synaptic concentrations only indirectly. Slight changes in the protein binding of an antipsychotic, without any change in total plasma concentration, may result in substantial differences in the levels of the freely available drug in the synapse. The observed receptor occupancy was related to the administered dose and measured plasma levels with use of the above equation implemented in SPSS for Windows (SPSS Inc., Chicago).
RESULTS
Data from all of the subjects studied are presented here. Dose significantly predicted loxapine and metabolite levels (loxapine levels in ng/ml=0.24×loxapine dose in mg/day [linear fit with no constant: F=23.7, df=1,9, p<0.001, R2=0.72]; 7-hydroxyloxapine levels in ng/ml=0.08×loxapine dose in mg/day [linear fit: F=370.6, df=1,9, p<0.001, R2=0.97]; 8-hydroxyloxapine levels in ng/ml=0.66×loxapine dose in mg/day [linear fit: F=79.9, df=1,9, p<0.001, R2=0.89]). The 7-hydroxyloxapine levels were, on average, 40% of the level of the parent compound, while the average of the 8-hydroxyloxapine levels was nearly 250% of that of the parent compound. The levels of the parent compound and the two metabolites were very highly correlated (for loxapine and 7-hydroxyloxapine, Pearson's r=0.87; for loxapine and 8-hydroxyloxapine, r=0.95; for 7-hydroxyloxapine and 8-hydroxyloxapine, r=0.97). The loxapine levels (not the metabolite levels) of one subject (subject 9) were clearly lower than expected and were reanalyzed to rule out any technical errors. He had, perhaps, an idiosyncratic metabolic profile, although the D2 and 5-HT2 occupancies were quite consistent with his dose.
The D2 and 5-HT2 occupancies are shown in table 1. The relation between occupancy and dose is captured by a saturating hyperbola depicted in figure 1. As shown in this plot, the dose to occupy 50% of D2 receptors was 9.6 mg/day (95% confidence interval=7.2–12.0); the dose to occupy 50% of 5-HT2 receptors was 13.6 mg/day (95% confidence interval=9.8–17.3). Loxapine is equipotent at the 5-HT2 and D2 receptors, since within a subject the D2 and 5-HT2 occupancies were not significantly different (t=1.72, df=1,9, p=0.12, paired t test), and the doses of loxapine to occupy 50% of D2 and 50% of 5-HT2 receptors were statistically indistinguishable.
DISCUSSION
Our study demonstrates that loxapine induces equivalent 5-HT2 occupancy and D2 occupancy as measured by [18F]setoperone and [11C]raclopride, respectively. We discuss these results in three conceptually different sections. First, we discuss the results of the in vivo 5-HT2 and D2 occupancies of loxapine in the context of the in vitro findings. Next, we compare the in vivo 5-HT2/D2 results of loxapine to those of the more widely accepted atypical neuroleptics clozapine and risperidone. Finally, we discuss these findings in light of our current knowledge regarding the 5-HT2/D2 receptor systems and their role in conferring atypicality upon antipsychotic action. We end the discussion with some suggestions for innovative pharmacological combinations that may be able to utilize the pharmacological profile of loxapine.
The first issue highlighted by our findings is the difference between the in vitro and in vivo results with loxapine. In vitro data from three different sources (1, 6, 7) all show that loxapine has a two- to five-times higher affinity for 5-HT2 receptors than for D2 receptors. If the in vitro affinity applies in vivo, one would expect that the dose of loxapine that gives 50% D2 occupancy would give anywhere between 66% and 80% 5-HT2 occupancy. In our data we found no support for this. Loxapine's superior affinity for 5-HT2 (versus D2) in vitro was not observed in vivo.
Stockmeier et al. (25) found a similar discrepancy between in vitro data and findings in rats. Loxapine showed a >2.5 times higher affinity for 5-HT2 versus D2 receptors in vitro (1), but this was reduced to <1.5 times higher in vivo (25). Stockmeier et al. speculated that loxapine's metabolites may have a higher affinity for the D2 receptor, thus obscuring the in vitro superior affinity for 5-HT2 of the parent compound. Our data support this contention of Stockmeier et al., since loxapine was extensively metabolized to hydroxy metabolites in the patients. In particular, the patients displayed high levels of 7-hydroxyloxapine, a metabolite that has a five times higher affinity for the D2 receptor in comparison with the parent compound (26). The other metabolite, 8-hydroxyloxapine, was found in higher quantities; however, it is relatively inert at the D2 receptors (26). Therefore, in all likelihood, the higher affinity of the 7-hydroxyloxapine metabolite for D2 receptors may have diminished the in vitro superiority of the parent compound for 5-HT2 (versus D2).
The second issue of importance is the relationship of the loxapine findings to PET studies of risperidone and clozapine. Nordström et al. (27) reported that patients taking clozapine exhibited 85%–94% 5-HT2 occupancy even at low doses, while their D2 occupancy varied from 20% to 67%. In a series of patients scanned with use of the methods described here, we observed that over the range of 2–12 mg/day, risperidone shows greater 5-HT2 than D2 occupancy. While at lower doses the difference between 5-HT2 occupancy and D2 occupancy may be as large as 15%–20%, at higher doses (>6 mg/day) the difference between occupancies is minimal, since both of the systems are near saturation. Therefore, the two atypical neuroleptics risperidone and clozapine show not only a high 5-HT2/D2 affinity ratio in vitro (7, 28, 29) but also a high 5-HT2 occupancy with a concomitant lower D2 occupancy at clinical doses. This may help us understand why loxapine, despite having a high 5-HT2/D2 affinity ratio in vitro, has not been associated with atypical clinical benefits. While it does have a potential for producing high 5-HT2 blockade, it does so only at doses that give a high degree of D2 blockade.
If these suggestions regarding the reasons for atypical efficacy (that is, high 5-HT2 occupancy with modest D2 occupancy) are correct, then it would seem that augmenting the 5-HT2 action of loxapine at a dose at which its D2 occupancy is low should lead to the atypical benefits of atypical neuroleptics. Loxapine may be an opportune agent for augmentation, because it shares with clozapine a high affinity for the dopamine D4 receptor (6, 30) along with affinity for the 5-HT3 receptor (31) and 5-HT6/5-HT7 receptors (32, 33). The exact contribution of these receptors to clozapine's uniqueness is not known (6, 31–33). However, given that loxapine also exhibits these properties, it is reasonable to hypothesize that augmenting the 5-HT2 profile of loxapine with an add-on 5-HT2 blocker, at a dose of the drug that provides modest D2 blockade (10–25 mg/day), would give it a profile very similar to that of clozapine and other atypical neuroleptics.
The main hurdle in testing this hypothesis is that there are no specific 5-HT2 antagonists available for regular human use. However, to provide a practical alternative, we have investigated cyproheptadine, an over-the-counter medication that is known to be a potent 5-HT2 blocker in vitro. We found that 12–18 mg/day of cyproheptadine produced more than 85% 5-HT2 blockade, as measured by the methods described above, in normal subjects (34). A combination of 10–25 mg/day of loxapine and 12–18 mg/day of cyproheptadine should provide a clozapine-like profile not only at the D2 and 5-HT2 receptors but also at the D4 and other serotonin, muscarinic, and histaminergic receptors. This combination needs to be tested in a clinical trial.
In summary, loxapine shows a higher affinity for 5-HT2 receptors than D2 receptors in vitro, but in humans the relative 5-HT2 superiority is lost. This may result from the potent action of its metabolite 7-hydroxyloxapine at D2 receptors, which may explain why loxapine, despite a very clozapine-like profile in the test tube, is not clinically an atypical neuroleptic. However, since loxapine shares several pharmacological properties with clozapine, it raises the possibility that if a low dose of loxapine (10–25 mg/day) is combined with a prominent 5-HT2 antagonist—thereby reinstating the 5-HT2 superiority that is lost in vivo—it may provide atypical antipsychotic benefits.
 |
Received Jan. 22, 1997; revision received May 2, 1997; accepted May 16, 1997. From the Schizophrenia Division and PET Centre, The Clarke Institute of Psychiatry, Department of Psychiatry, University of Toronto; the Rotman Research Institute, Baycrest Centre, University of Toronto; and the College of Pharmacy and Nutrition, University of Saskatchewan, Saskatoon, Canada. Address reprint requests to Dr. Kapur, PET Centre, The Clarke Institute of Psychiatry, 250 College St., Toronto, ON, Canada M5T 1R8; [email protected].ca (e-mail). Supported by an award from the National Alliance for Research on Schizophrenia and Depression and the Medical Research Council of Canada (Dr. Kapur) and partial financial assistance from Wyeth-Ayerst Laboratories. The authors thank Doug Hussey, Kevin Cheung, Stephen Dobbin, and Terry Bell for technical assistance; Astra Arcus AB for providing the precursor used in the synthesis of [11C]raclopride; Janssen-Cilag (France) for providing the precursor for the synthesis of setoperone; and Drs. Alan Wilson and Jean DaSilva for radiochemical synthesis of [18F]setoperone and [11C]raclopride for the study.
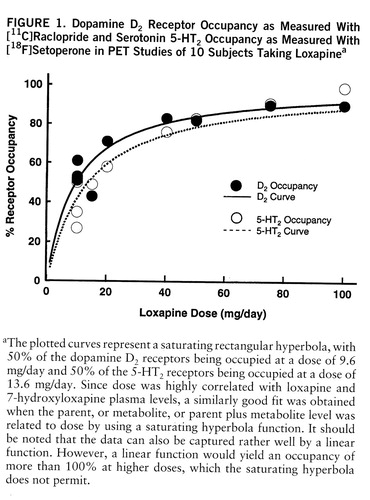
FIGURE 1. Dopamine D2 Receptor Occupancy as Measured With [11C]Raclopride and Serotonin 5-HT2 Occupancy as Measured With [18F]Setoperone in PET Studies of 10 Subjects Taking Loxapinea
aThe plotted curves represent a saturating rectangular hyperbola, with 500f the dopamine D2 receptors being occupied at a dose of 9.6 mg/day and 500f the 5-HT2 receptors being occupied at a dose of 13.6 mg/day. Since dose was highly correlated with loxapine and 7-hydroxyloxapine plasma levels, a similarly good fit was obtained when the parent, or metabolite, or parent plus metabolite level was related to dose by using a saturating hyperbola function. It should be noted that the data can also be captured rather well by a linear function. However, a linear function would yield an occupancy of more than 100at higher doses, which the saturating hyperbola does not permit.
1. Meltzer HY, Matsubara S, Lee JC: The ratios of serotonin-2 and dopamine-2 affinities differentiate atypical and typical antipsychotic drugs. Psychopharmacol Bull 1989; 25:390–392Medline, Google Scholar
2. Meltzer HY, Matsubara S, Lee JC: Classification of typical and atypical antipsychotic drugs on the basis of dopamine D-1, D-2 and serotonin-2 pKi values. J Pharmacol Exp Ther 1989; 251:238–246Medline, Google Scholar
3. Kapur S, Remington G: Serotonin-dopamine interaction and its relevance to schizophrenia. Am J Psychiatry 1996; 153:466–476Link, Google Scholar
4. Meltzer HY: The role of serotonin in schizophrenia and the place of serotonin-dopamine antagonist antipsychotics. J Clin Psychopharmacol 1995; 15:2S–3SCrossref, Medline, Google Scholar
5. Seeman P: Therapeutic receptor-blocking concentrations of neuroleptics. Int Clin Psychopharmacol 1995; 10:5–13Medline, Google Scholar
6. Singh AN, Barlas C, Singh S, Franks P, Mishra RK: A neurochemical basis for the antipsychotic activity of loxapine: interactions with dopamine D1, D2, D4 and serotonin 5-HT2 receptor subtypes. J Psychiatry Neurosci 1996; 21:1–7Google Scholar
7. Leysen JE, Janssen PM, Schotte A, Luyten WH, Megens AA: Interaction of antipsychotic drugs with neurotransmitter receptor sites in vitro and in vivo in relation to pharmacological and clinical effects: role of 5HT2 receptors. Psychopharmacology (Berl) 1993; 112:S40–S54Google Scholar
8. Helmeste DM, Tang SW: Unusual acute effects of antidepressants and neuroleptics on S2-serotonergic receptors. Life Sci 1983; 33:2527–2533Google Scholar
9. Lee T, Tang SW: Loxapine and clozapine decrease serotonin (S2) but do not elevate dopamine (D2) receptor numbers in the rat brain. Psychiatry Res 1984; 12:277–285Crossref, Medline, Google Scholar
10. Seeman P: Receptor Tables: Drug Dissociation Constants for Neuroreceptors and Transporters, vol 2. Toronto, SZ Research, 1993Google Scholar
11. Kapur S, Zipursky R, Jones C, Remington G, Wilson A, DaSilva J, Houle S: The D2 receptor occupancy profile of loxapine determined using PET. Neuropsychopharmacology 1996; 15:562–566Crossref, Medline, Google Scholar
12. Houle S, Kapur S, Hussey D, Jones C, DaSilva J, Wilson AA: Measurement of [11C]-raclopride binding using a bolus plus infusion protocol, in Quantification of Brain Function Using PET. Edited by Myers R, Cunningham B, Bailey D, Jones T. San Diego, Academic Press, 1996, pp 262–265Google Scholar
13. Farde L, Nordstrom AL, Wiesel FA, Pauli S, Halldin C, Sedvall G: Positron emission tomographic analysis of central D1 and D2 dopamine receptor occupancy in patients treated with classical neuroleptics and clozapine: relation to extrapyramidal side effects. Arch Gen Psychiatry 1992; 49:538–544Crossref, Medline, Google Scholar
14. Blin J, Pappata S, Kiyosawa M, Crouzel C, Baron JC: [18F]Setoperone: a new high-affinity ligand for positron emission tomography study of the serotonin-2 receptors in baboon brain in vivo. Eur J Pharmacol 1988; 147:73–82Crossref, Medline, Google Scholar
15. Blin J, Sette G, Fiorelli M, Bletry O, Elghozi JL, Crouzel C, Baron JC: A method for the in vivo investigation of the serotonergic 5-HT2 receptors in the human cerebral cortex using positron emission tomography and 18F-labeled setoperone. J Neurochem 1990; 54:1744–1754Google Scholar
16. Crouzel C, Venet M, Irie T, Sanz G, Boullais C: Labeling of a serotoninergic ligand with 18F: [18F]-setoperone. J Labelled Compounds and Radiopharmaceuticals 1988; 25:403–414Crossref, Google Scholar
17. Pazos A, Probst A, Palacios JM: Serotonin receptors in the human brain, IV: autoradiographic mapping of serotonin-2 receptors. Neuroscience 1987; 21:123–139Crossref, Medline, Google Scholar
18. Petit-Taboue MC, Landeau B, Osmont A, Tillet I, Barre L, Baron JC: Estimation of neocortical serotonin-2 receptor binding potential by single-dose fluorine-18-setoperone kinetic PET data analysis. J Nucl Med 1996; 37:95–104Medline, Google Scholar
19. Mazoyer B: Investigation of the dopamine system with positron emission tomography: general issues in modelling, in Brain Dopaminergic Systems: Imaging With Positron Emission Tomography, vol 20. Edited by Baron J, Comar D, Farde L, Martinot J, Mazoyer B. Dordrecht, the Netherlands, Kluwer Academic, 1991, pp 64–83Google Scholar
20. Kapur S, Jones C, DaSilva J, Wilson A, Houle S: Reliability of a simple non-invasive method for the evaluation of 5-HT2 receptors using [18F]-setoperone PET imaging. Nucl Med Commun 1997; 18:395–399Crossref, Medline, Google Scholar
21. Wong DF, Wagner HN Jr, Dannals RF, Links JM, Frost JJ, Ravert HT, Wilson AA, Rosenbaum AE, Gjedde A, Douglass KH: Effects of age on dopamine and serotonin receptors measured by positron tomography in the living human brain. Science 1984; 226:1393–1396Google Scholar
22. Lewis R, Kapur S, Jones C, DaSilva J, Roy P, Brown G, Wilson A, Houle S, Zipursky R: PET study of the 5-HT2 receptor density in schizophrenia (abstract). Biol Psychiatry 1997; 41:63SGoogle Scholar
23. Okubo Y, Suhara T, Sudo Y, Someya Y, Sassa T, Terasaki O, Suzuki K, Toru M: Dopamine D1, D2 and 5HT2 receptors in schizophrenic patients: a PET study using [11C]-SCH23390 and [11C]-NMSP, in Abstract Book of the Third Pan Pacific Conference on Brain Topography, Tokyo, Japan, 1997, p 18Google Scholar
24. Midha KK, Hubbard JW, McKay G, Hawes EM, Hsia D: The role of metabolites in a bioequivalence study, 1: loxapine, 7-hydroxyloxapine and 8-hydroxyloxapine. Int J Clin Pharmacol Ther Toxicol 1993; 31:177–183Medline, Google Scholar
25. Stockmeier CA, DiCarlo JJ, Zhang Y, Thompson P, Meltzer HY: Characterization of typical and atypical antipsychotic drugs based on in vivo occupancy of serotonin2 and dopamine2 receptors. J Pharmacol Exp Ther 1993; 266:1374–1384Google Scholar
26. Coupet J, Rauh CE: 3H-Spiroperidol binding to dopamine receptors in rat striatal membranes: influence of loxapine and its hydroxylated metabolites. Eur J Pharmacol 1979; 55:215–218Crossref, Medline, Google Scholar
27. Nordström A-L, Farde L, Nyberg S, Karlsson P, Halldin C, Sedvall G: D1, D2, and 5-HT2 receptor occupancy in relation to clozapine serum concentration: a PET study of schizophrenic patients. Am J Psychiatry 1995; 152:1444–1449Google Scholar
28. Schotte A, Janssen PFM, Gommeren W, Luyten WHML, VanGompel P, Lesage AS, DeLoore K, Leysen JE: Risperidone compared with new and reference antipsychotic drugs: in vitro and in vivo receptor binding. Psychopharmacology (Berl) 1996; 124:57–73Crossref, Medline, Google Scholar
29. Kapur S, Remington G, Zipursky RB, Wilson AA, Houle S: The D2 dopamine receptor occupancy of risperidone and its relationship to extrapyramidal symptoms: a PET study. Life Sci 1995; 57:PL103–PL107Google Scholar
30. Roth BL, Tandra S, Burgess LH, Sibley DR, Meltzer HY: D4 dopamine receptor binding affinity does not distinguish between typical and atypical antipsychotic drugs. Psychopharmacology (Berl) 1995; 120:365–368Crossref, Medline, Google Scholar
31. Bolanos FJ, Schechter LE, Miquel MC, Emerit MB, Rumigny JF, Hamon M, Gozlan H: Common pharmacological and physico-chemical properties of 5-HT3 binding sites in the rat cerebral cortex and NG 108-15 clonal cells. Biochem Pharmacol 1990; 40:1541–1550Google Scholar
32. Roth BL, Craigo SC, Choudhary MS, Uluer A, Monsma FJ Jr, Shen Y, Meltzer HY, Sibley DR: Binding of typical and atypical antipsychotic agents to 5-hydroxytryptamine-6 and 5-hydroxytryptamine-7 receptors. J Pharmacol Exp Ther 1994; 268:1403–1410Google Scholar
33. Shen Y, Monsma FJ Jr, Metcalf MA, Jose PA, Hamblin MW, Sibley DR: Molecular cloning and expression of a 5-hydroxytryptamine7 serotonin receptor subtype. J Biol Chem 1993; 268:18200–18204Google Scholar
34. Kapur S, Zipursky RB, Jones C, Wilson AA, DaSilva JD, Houle S: Cyproheptadine: a potent in vivo serotonin antagonist (letter). Am J Psychiatry 1997; 153:884Google Scholar



