Antidepressant Adherence and Medical Resource Use Among Managed Care Patients With Anxiety Disorders
Anxiety disorders are among the most prevalent psychiatric disorders in the United States. Although findings from studies vary, it is estimated that the lifetime prevalence of anxiety disorders ranges from 13.9 to 28.8 percent ( 1 , 2 ). The term anxiety disorder encompasses several conditions, including generalized anxiety disorder, social anxiety disorder, phobias, panic disorder, obsessive-compulsive disorder, acute stress disorder, and posttraumatic stress disorder (PTSD) ( 3 ). Of all the anxiety disorders identified by the DSM-IV, those most often encountered in primary care are panic disorder, generalized anxiety disorder, social anxiety disorder, and PTSD ( 1 ).
Pharmacotherapy for anxiety disorders has evolved over the years. Benzodiazepines have been used since the 1960s because of their anxiolytic and muscle relaxant properties. Some evidence from the National Medical Expenditure Surveys shows that use of benzodiazepines in the outpatient treatment of anxiety disorders has declined in recent years, although this trend was not statistically significant (a decrease from 42.3 to 31.7 percent from 1987 to 1999; p=.09) ( 4 ). However, the Harvard/Brown Anxiety Research Project (HARP), a prospective naturalistic follow-along study of patients with anxiety disorders, found that medication treatment patterns for panic disorder with agoraphobia changed little from the beginning to the end of the last decade, with benzodiazepine rates declining slightly but remaining high throughout the study period ( 5 ).
Current recommendations for the treatment of anxiety disorders advocate the initiation of antidepressant therapy, with selective serotonin reuptake inhibitors (SSRIs) or serotonin-norepinephrine reuptake inhibitors (SNRIs) recommended as first-line agents ( 6 , 7 , 8 ). Other antidepressant agents, such as tricyclic antidepressants and monoamine oxidase inhibitors, have utility for at least several of the anxiety disorders, although they may no longer be commonly prescribed for these indications ( 7 , 9 ). Other second-generation antidepressant agents (for example, mirtazapine or nefazodone) have very limited evidence for their efficacy in the treatment of anxiety disorders. SSRIs and SNRIs are considered first-line therapy because of their ability to relieve anxiety and depressive symptoms while maintaining better safety and tolerability profiles than tricyclic antidepressants.
But there is evidence, in the case of major depression treatment, of inadequate treatment with SSRIs in the community. Even with the improved tolerability profile, SSRIs have been associated with failure to reach therapeutic dosages and acceptable treatment outcomes, primarily because of premature treatment discontinuation and nonadherence ( 10 ). Eaddy and colleagues ( 11 ) found that 28 percent of 76,107 patients taking SSRIs discontinued antidepressant therapy within the first month of treatment. Lin and colleagues ( 10 ) found similar discontinuation rates, with more than 60 percent of the 43 participants who discontinued treatment early citing adverse effects as the primary reason for ending therapy. Adherence to SSRI treatment for anxiety disorders is an important factor in achieving treatment goals; however, little information exists about the level of adherence among patients with anxiety disorders.
Research evaluating the health-related economic consequences of nonadherence among patients with depression indicates a strong association between nonadherence and increased resource utilization and hospitalizations ( 12 , 13 , 14 ). It has been well established that anxiety disorders are associated with substantial economic burden, fueled by patients' inability to work and impairment in social functioning and by the fact that anxious patients are often high utilizers of medical services ( 3 , 15 , 16 , 17 , 18 ). As suggested by previous work in panic disorder, successful treatment of anxiety disorders may reduce inappropriate medical utilization and is certainly cost-effective ( 19 , 20 ). However, no studies have assessed the association between medication adherence for anxiety and medical resource utilization. The primary objective of this analysis was to evaluate the adherence of patients initiating SSRI or SNRI antidepressant therapy for anxiety alone or anxiety and comorbid depression and to quantify the health-related economic correlates of nonadherence. A database was used to retrospectively examine the data. The primary hypothesis was that nonadherence would be high among patients with anxiety disorders. The secondary hypothesis was that patients who were nonadherent to SSRI or SNRI therapy would incur greater health resource utilization costs than those who were adherent.
Methods
Data source
Medical and pharmacy data were abstracted from the Integrated Healthcare Information Services National Managed Care Benchmark database located in Waltham, Massachusetts. This nationally representative database includes data from 30 health plans covering more than 25 million persons. Institutional review board approval was not required for this study design.
Sample selection
All patients who received at least one prescription for the following antidepressants between July 1, 2001, and December 31, 2002, were identified in the database: venlafaxine, venlafaxine extended release, fluoxetine, sertraline, paroxetine, paroxetine controlled release, citalopram, escitalopram, and fluvoxamine. The index date was the date of each patient's first antidepressant prescription within this period. Patients were required to be at least 18 years of age, have no evidence of antianxiety therapy for six months before their index date, and to be continuously eligible for medical and pharmacy service for six months before and 12 months after their index date. Patients were also required to have a coded diagnosis of anxiety alone or anxiety and comorbid depression in the six months before or within one year after their index date. Table 1 shows the ICD-9-CM codes used for such diagnoses. Patients were excluded from the study if there was evidence of schizophrenia or bipolar disorders or the presence of an antipsychotic medication. Patients who met all selection criteria were then followed for 12 months after their index date to assess six-month antidepressant utilization and 12-month medical resource utilization.
 |
Adherence measure
Antidepressant adherence was measured by calculating a medication possession ratio, which used the methodology of continuous, multiple-interval medications available, as described by Steiner and Prochazka ( 21 ). The medication possession ratio is the sum of the days' supply of all antidepressant prescriptions in a specific period divided by the total number of days during the specified period. In this analysis, all prescriptions were given a starting date (date the prescription was filled) and ending date (date corresponding to the starting date of the prescription plus the days' supply). When prescriptions overlapped (that is, when a patient acquired an additional prescription before the ending date of the preceding prescription), residual days were added to the ending date of the next prescription. Thus patients were assumed to have consumed all medications acquired during the study period. As a result, patients with medication possession ratio values above 100 percent were truncated at 100 percent.
For analysis, the medication possession ratio was dichotomized by using a threshold of 80 percent to deem patients adherent or nonadherent to antidepressant therapy. The 80 percent threshold was adapted from HEDIS depression performance measures that state that patients should be on antidepressant therapy acutely for 84 of 114 days (74 percent) and continuously for 180 of 231 days (78 percent) ( 22 ). Patients were then placed into one of two cohorts on the basis of their adherence with antidepressant therapy.
Because it is understood that various other drug utilization patterns may not be adequately captured by a traditional medication possession ratio, patients were further stratified into two additional cohorts to evaluate resource utilization. Previous findings in the literature have suggested that patients who switch medications, receive additional medications to augment treatment, or receive an increase in antidepressant dosage are the costliest patients ( 12 ). Thus, to capture patients who had continuous antianxiety therapy with these utilization patterns in this analysis, patients who met the minimum criteria for adequate therapy (80 percent medication possession ratio) while having a change in medication or a titration of the medication dosage were placed into two cohorts ("adherent, change in medication" and "adherent, dosage was titrated"), which were distinct from patients with adequate therapy with no change in medication or dosage ("adherent, no change") and from patients without adequate therapy ("nonadherent"). Use of these four distinct cohorts to assess resource utilization is consistent with previous work in this area ( 11 , 12 ).
Medical comorbidity assessment
To assess comorbid conditions across the adherence cohorts, the Charlson index, with Dartmouth-Manitoba and Deyo modification, was used ( 23 , 24 ). This index contains 19 categories of comorbid medical conditions (primarily physical, such as heart, lung, and renal disease; also included are several neuropsychiatric conditions, including Parkinson's disease and dementia), primarily defined by ICD-9-CM diagnosis codes. Higher scores represent a more severe burden of comorbid medical conditions. Charlson index scores for this study were derived by evaluating the presence of various ICD-9-CM codes in the six-month period before each patient's index date.
Additional variables used to assess comorbid conditions in the six months before each patient's index date included a unique count of non-mental health disease states beyond the index diagnoses and those used to calculate the Charlson index, the total number of prescriptions received, and a unique count of prescription drug categories received.
Analysis of outcomes
Once patients were deemed adherent or nonadherent to antidepressant therapy, their medical resource utilization was evaluated. Medical resource utilization was defined as the total amount charged for physician visits, inpatient hospitalizations, outpatient hospital care, emergency department visits, and other services. Descriptive analyses were conducted to assess the differences in medical resource utilization across the adherence cohorts.
Inferential analyses were performed to assess the impact of antidepressant adherence on medical resource utilization. Statistical differences in charges across adherence cohorts were determined by using analysis of covariance models, controlling for differences in age (continuous), gender, utilization of psychiatric specialty care services (dichotomous, yes or no), therapy change rates (dichotomous, yes or no), titration rates (dichotomous, yes or no), costs in the six months before the index date (continuous), and the comorbidity measures (continuous). Because evidence shows that patients who receive psychiatric specialty care are more adherent to antidepressant treatment than those who receive care from primary care practitioners or other medical specialists, statistical differences across adherence cohorts were also assessed by utilization of mental health specialty practitioners ( 25 ). The alpha level of significance was set a priori at .05.
Results
Sample characteristics
A total of 13,085 patients met all study inclusion criteria. As Table 2 shows, 68 percent of the sample was female; the mean age was 42 years. Patients with anxiety disorders alone or comorbid anxiety and depressive disorders were nearly equally represented in the sample (6,867 patients with anxiety disorders alone, or 52 percent, and 6,218 patients with comorbid anxiety and depressive disorders, or 48 percent). Of the total sample, 35 percent visited a mental health specialist within one year of initiating treatment.
 |
Few differences were found across diagnostic cohorts in background characteristics ( Table 2 ). Patients with anxiety disorders alone and those with comorbid anxiety and depressive disorders were statistically similar in terms of age, Charlson comorbidity index, and the total number of non-anxiety related prescriptions obtained before initiating antianxiety treatment. Patients with a dual diagnosis of anxiety and depression were more likely to be female (66 percent compared with 70 percent; χ 2 =32.7, df=1, p<.05), had more coded disease states before being placed on antianxiety treatment (t=7.14; df=13,083, p<.001), and were more likely to receive care from a mental health specialist (χ 2 =497.11, df=1, p<.001).
Anxiety diagnoses
As shown in Table 2 , when patients were distinguished by the type of anxiety disorder, the most commonly coded single anxiety disorder was generalized anxiety disorder (15 percent). Diagnoses of multiple anxiety disorders were also common (18 percent). Patients who were given dual diagnoses of anxiety and depression were more likely to have more than one type of anxiety disorder or to have PTSD but were less likely to have generalized anxiety disorder, obsessive-compulsive disorder, or panic disorder. However, the most common anxiety disorder category coded was "other" (53 percent); this category included "other" anxiety states ( ICD-9 300.09), anxiety due to a general medical condition ( ICD-9 293.89), and anxiety not otherwise specified ( ICD-9 300.00). The frequent use of the "other" category suggests that treating clinicians were unlikely to make specific anxiety disorder diagnoses.
Resource use
The costs of medical care, anxiety-related prescriptions, and non-anxiety-related prescriptions were evaluated over the 12-month follow-up period ( Table 3 ). Patients with dual diagnoses of anxiety and depression had significantly higher total costs than patients with anxiety alone ($5,367 compared with $4,411; t=8.31, df=13,083, p<.001). Anxiety-related pharmacy costs, which included both antidepressants and anxiolytic agents, accounted for 11 percent of the total cost of care in each cohort and differed significantly between each cohort: $498 among patients with anxiety alone compared with $589 among patients with anxiety and depression (t=12.26, df=13,083, p<.001). Total one-year costs were driven by medical costs, which accounted for 69 percent of the total costs for patients with anxiety alone and 72 percent of the total costs for patients with both anxiety and depression; medical costs differed significantly between the two groups ($3,057 compared with $3,876, respectively; t=8.03, df=13,083, p<.001).
 |
As shown in Figure 1 , when resource utilization was analyzed across anxiety diagnoses, patients with a coded diagnosis of PTSD had the highest one-year total costs ($6,049), and patients with obsessive-compulsive disorder had the lowest costs ($4,453).
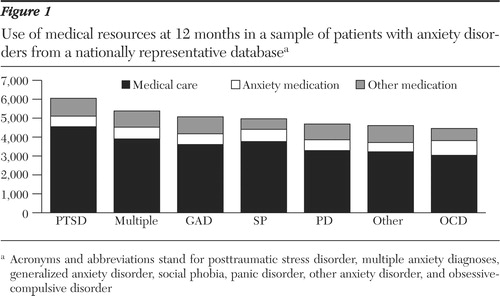
a Acronyms and abbreviations stand for posttraumatic stress disorder, multiple anxiety diagnoses, generalized anxiety disorder, social phobia, panic disorder, other anxiety disorder, and obsessivecompulsive disorder
Adherence
On the basis of an 80 percent medication possession ratio threshold, approximately 57 percent of patients with anxiety disorders were deemed nonadherent at six months ( Tables 4 and 5 ). Adherence rates were lower for patients with anxiety disorders alone (40 percent) than for patients with both anxiety and depression (47 percent; χ 2 =57.26, df=1, p<.001). Among all patients, approximately 32 percent had evidence of some change in medication therapy. Compared with patients with both anxiety and depression, patients with anxiety disorder alone were less likely to change their medication (25 percent compared with 40 percent; χ 2 =167.86, df=1, p<.001) or have their dosage titrated (43 percent compared with 58 percent; χ 2 =21.90, df=1, p<.001).
 |
 |
Patients who received mental health specialty care were more likely than those who did not receive such care to be adherent to their antidepressant therapy after six months. This effect was consistent across diagnostic cohorts: 812 of 1,771 (46 percent) compared with 1,951 of 5,096 patients (38 percent) for patients with anxiety only (χ 2 =31.16, df=1, p<.001) and 1,388 of 2,770 patients (50 percent) compared with 1,523 of 3,448 patients (44 percent) for patients with both anxiety and depression (χ 2 =21.11, df=1, p<.001).
Patients seen by a mental health specialist were also more likely than those who were not to have their dosage titrated (2,895 of 4,541 patients, or 64 percent, compared with 3,665 of 8,544 patients, or 43 percent; χ 2 =515.94, df=1, p<.001) and to have a switch in medication (1,888 of 4,541 patients, or 42 percent, compared with 2,277 of 8,544 patients, or 27 percent; χ 2 =304.45, df=1, p<.001).
Pharmacotherapy patterns and resource use
When patients were placed into cohorts on the basis of their pharmacotherapy utilization patterns—nonadherent; adherent, no change; adherent, dosage was titrated; and adherent, change in medication—patients who were nonadherent to SSRI or SNRI therapy had the lowest anxiety-related pharmacy costs, and patients who were adherent but had a therapy change had the highest anxiety-related pharmacy costs, regardless of diagnostic cohort ( Tables 4 and 5 ).
After the analysis controlled for background covariates through multivariate techniques, the cohort that was adherent to no change was associated with lower medical costs compared with the other three groups, although the level of significance varied slightly ( Tables 4 and 5 ). Anxiety-related pharmacy costs for patients in the adherent to no change cohort were statistically lower than those for patients who were adherent and who changed medication or whose dosage was titrated and higher than those for patients who were nonadherent (F=373.15, df=6, 850, p<.05). When medical and anxiety-related pharmacy costs were summed, costs for patients who were adherent and had no change in medication were similar to those for nonadherent patients and lower than those for patients who were adherent and changed medication or whose dosage was titrated. For total one-year costs (medical and all pharmacy), similar results were found: the cost for patients who were adherent to no change in medication or dosage was statistically similar to those of nonadherent patients but significantly lower costs for patients who required a titration in dosage or a change in medication (F=136.24, df=6, 850, p<.05).
Discussion
The purpose of this analysis was to evaluate the adherence of patients who initiated non-tricyclic antidepressant therapy for anxiety disorders alone or comorbid anxiety and depressive disorders and to quantify the health economic consequences of nonadherence. By using claims data with clinician-coded diagnoses, we found that only 43 percent of patients with a diagnosis of anxiety, alone or in combination with depression, were adherent to SSRI or SNRI therapy over a six-month period. Although similar data have been reported among patients with major depression, to the best of our knowledge, this is the first report of SSRI or SNRI adherence figures in a large representative sample of patients with anxiety disorders. The findings add to the current literature showing low rates of quality of pharmacotherapy among patients with anxiety disorders managed in primary care settings and overall low rates of adequate care provided to patients with anxiety disorders in the U.S. general population ( 26 , 27 ). This finding is important because treatment recommendations for anxiety disorders emphasize the importance of prolonged treatment with SSRIs or SNRIs ( 6 , 7 , 8 ).
These results parallel similar findings evaluating rates of discontinuation among all patients initiating SSRI therapy ( 11 ). The nature and cause of poor medication adherence have been primarily linked to a high incidence of medication-related adverse events, which is also one of the main reasons for a change in therapy ( 10 , 28 , 29 ). In this study patients with anxiety disorders with comorbid depression were more likely than those with comorbid depression to require a change in therapy. A possible explanation for this finding may be that patients with comorbid anxiety and depression commonly have more severe symptoms and a poorer outcome than patients without comorbid depression and may thus require more aggressive treatment ( 30 , 31 ). Of interest is that more patients with comorbid depression and anxiety had PTSD or multiple anxiety disorders, consistent with results from representative national U.S. surveys ( 32 ).
The level of adherence was lower among patients with anxiety than among patients with comorbid anxiety and depression. A possible reason for the lower rates of adherence is the lower likelihood of mental health specialty care within this population. In this study, compared with patients with comorbid depression, significantly fewer patients with anxiety alone received mental health specialty care during the year after antidepressant initiation (26 percent compared with 45 percent; χ 2 =506.71, df=1, p<.001).
When adherence was stratified by mental health specialty care, we saw that patients who received specialty care had significantly higher rates of antidepressant therapy adherence at six months and were more likely to have received a dosage titration or medication change, paralleling previous studies in which patients who were seen by a mental health practitioner were more likely to adhere to therapy and more likely to receive adequate therapy ( 25 , 27 ). Another possible reason for the low rates of adherence in the anxiety-only cohort is the possible mistaken belief on the part of practitioners or patients that anxiety disorders require a lower intensity or duration of treatment than depression. The inordinately frequent use of the "other" anxiety diagnosis category (including "anxiety not otherwise specified") may speak to the relative inattention of practitioners to anxiety diagnoses. It would not be surprising if this inattention extended to their beliefs about the importance of aggressively treating these disorders. Future studies that directly address practitioner and physician attitudes toward anxiety disorders and their treatment will be required to evaluate this and other possibilities.
Although the reasons for low medication adherence cannot be definitively determined, the health economic correlates of low adherence are nonetheless worth considering. Studies of depression have shown that improved antidepressant adherence is associated with not only a decrease in resource utilization but also an improvement in treatment outcomes ( 14 ). Our study indicates that patients adherent to therapy without the need of titration or therapy change incurred higher pharmacy costs than patients who were not adherent to therapy. However, the increased pharmacy costs were offset by reduced medical costs, resulting in similar total costs (medical and pharmacy) between the two groups. These data are observational only and cannot speak to whether efforts directed at improving adherence would result in a cost offset—as has been seen in some studies ( 20 )—and improve health-related quality of life in a cost-effective fashion. Prospective studies that directly target medication adherence among patients with anxiety disorders are needed to test this hypothesis.
In this study, benzodiazepines and tricyclic antidepressants were not included as initial antianxiety agents, but data for patients who switched to these agents or whose therapy was augmented with them were included in the analyses; therefore, the results may not be generalizable to all agents used to treat anxiety. However, adherence was still less than optimal. This finding may indicate the need for improved patient or provider education about the benefits of higher adherence with SSRI or SNRI therapy or the increased use of agents that are associated with improved adherence. Disease management programs that target, among other things, medication adherence, may be beneficial in this regard. In fact, preliminary evidence shows that collaborative care programs for panic disorder in primary care may improve medication adherence ( 33 ), although increased levels of adherence have not always been found ( 34 ).
Although this is the first study to assess anxiety-related pharmacotherapy utilization patterns and the association with resource utilization in a managed care population, various limitations must be addressed. First, therapy change in this population was associated with higher resource utilization. However, the reason and effectiveness of the switch or augmentation could not be measured and does not take into account whether such patterns of care are successful in the management of anxiety. The differential rates of therapy change and costs may be associated with a population with more severe symptoms. For instance, patients with comorbid anxiety and depression had higher rates of mental health specialty care and a greater burden of medical comorbidity than patients with anxiety disorders alone.
In addition, the use of claims data may not allow for the accurate representation of the prevalence of anxiety or comorbid depression ( 35 ). The actual incidence of these comorbid disorders may be higher than that reported. This lack of control over diagnostic accuracy can also be seen in the frequent use of the "other" anxiety diagnosis category and lower than expected rates of PTSD and social anxiety disorder. The inordinately high rate of the "other" anxiety diagnosis category may speak to the relative inattention of practitioners to diagnosing anxiety disorders versus transient feelings of anxiety that may not require prolonged pharmacotherapy. Although undercoding and use of the "other" category may signify differences in perception between recommended therapy and actual practice, the effects of undercoding were not measurable in this study. Future studies to address practitioner and physician attitudes toward anxiety disorders and their treatment will be required to evaluate this and other possibilities.
Despite the discussed limitations, this study highlights the relatively low rate of antidepressant adherence among patients with anxiety disorders in managed care settings. It also draws attention to the somewhat better rates of antidepressant adherence that occur in specialty mental health settings compared with primary care settings. It has been well established that anxiety disorders are associated with substantial health economic burden ( 3 , 36 ). Additional work is needed to assess the effects of medication adherence on social functioning and work productivity. Our study found that, much like studies in depression ( 12 ), patients requiring a medication change or a titration in dosage were the most costly cohorts. Future studies should also evaluate whether changes in anxiety therapy result from ineffective treatment or adverse events and whether such changes could be avoided by the initial use of strategies to maximize effectiveness and tolerability of pharmacological agents in the treatment of anxiety disorders.
Conclusions
Only 43 percent of patients who initiated treatment with SSRI or SNRI therapy for anxiety disorders were adherent over a six-month period, with the lowest levels of adherence being found among patients without a comorbid diagnosis of depression (that is, anxiety disorders only). Adherence was higher among patients treated in mental health specialty settings than among those treated in primary care settings. Patients with anxiety disorders who were adherent to therapy and did not need to change their medication or have their dosage titrated incurred lower 12-month medical costs than adherent patients who required such changes and nonadherent patients. However, total 12-month costs (incorporating pharmacy costs) were similar for adherent patients with no change in medication or dosage and nonadherent patients and were significantly greater for adherent patients whose medication was changed or whose dosage was titrated. Future studies should evaluate whether rates of adherence can be improved by using specific strategies to minimize adverse events (which could include the selection of specific therapeutic agents or optimization of dosing regimens), to educate physicians about the importance of long-term treatment for anxiety disorders, and to better engage patients in management of their illness.
Acknowledgments
This study was funded by GlaxoSmithKline. Dr. Stein has been a paid consultant to GlaxoSmithKline and to numerous other pharmaceutical companies that market SSRIs or SNRIs.
1. Stein MB: Attending to anxiety disorders in primary care. Journal of Clinical Psychiatry 64(suppl 15):35-39, 2003Google Scholar
2. Kessler RC, Berglund P, Demler O, et al: Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry 62:593-602, 2005Google Scholar
3. Arikian S, Gorman J: A review of the diagnosis, pharmacologic treatment, and economic aspects of anxiety disorders. Primary Care Companion of the Journal of Clinical Psychiatry 3:110-117, 2001Google Scholar
4. Olfson M, Marcus SC, Wan GJ, et al: National trends in the outpatient treatment of anxiety disorders. Journal of Clinical Psychiatry 65:1166-1173, 2004Google Scholar
5. Bruce SE, Vasile RG, Goisman RM, et al: Are benzodiazepines still the medication of choice for patients with panic disorder with or without agoraphobia? American Journal of Psychiatry 160:1432-1438, 2003Google Scholar
6. Practice guideline for the treatment of patients with panic disorder: Work Group on Panic Disorder: American Psychiatric Association. American Journal of Psychiatry 155 (suppl 5):1-34, 1998Google Scholar
7. Practice Guideline for the Treatment of Patients With Acute Stress Disorder and Posttraumatic Stress Disorder. American Psychiatric Association, 2004. Available at www.psych.org/psychpract/treatg/pg/ptsd-pg-partsa-b-c-new.pdfGoogle Scholar
8. Ballenger JC, Davidson JRT, Lecrubier Y, et al: Consensus statement on generalized anxiety disorder from the International Consensus Group on Depression and Anxiety. Journal of Clinical Psychiatry 62(suppl 11):53-58, 2001Google Scholar
9. Simon NM, Emmanuel N, Ballenger J, et al: Bupropion sustained release for panic disorder. Psychopharmacology Bulletin 37:66-72, 2003Google Scholar
10. Lin EH, Von Korff M, Katon W, et al: The role of the primary care physician in patients' adherence to antidepressant therapy. Medical Care 33:67-74, 1995Google Scholar
11. Eaddy M, Bramley T, Regan T: Time to antidepressant discontinuation: a comparison of controlled-release paroxetine and immediate-release selective serotonin-reuptake inhibitors. Managed Care Interface 16:22-27, 2003Google Scholar
12. Thompson D, Buesching D, Gregor KJ, et al: Patterns of antidepressant use and their relation to costs of care. American Journal of Managed Care 2:1239-1246, 1995Google Scholar
13. White TJ, Vanderplas A, Ory C, et al: Economic impact of patient adherence with antidepressant therapy within a managed care organization. Disease Management and Health Outcomes 11:817-822, 2003Google Scholar
14. Sheehan DV, Eaddy M, Sarnes M, et al: Evaluating the economic consequences of early antidepressant treatment discontinuation. Journal of Clinical Psychopharmacology 24:544-548, 2004Google Scholar
15. Katon W, Von Korff M, Lin E, et al: Distressed high utilizers of medical care: DSM-III-R diagnoses and treatment needs. General Hospital Psychiatry 12:355-362, 1990Google Scholar
16. Schmitz N, Kruse J: The relationship between medical disorders and medical service utilization in a representative community sample. Social Psychiatry and Psychiatric Epidemiology 37:380-386, 2002Google Scholar
17. Sanderson K, Andrews G: Prevalence and severity of mental health-related disability and relationship to diagnosis. Psychiatric Services 53:80-86, 2002Google Scholar
18. Rapaport MH, Clary C, Fayyad R, et al: Quality-of-life impairment in depressive and anxiety disorders. American Journal of Psychiatry 162:1171-1178, 2005Google Scholar
19. Katon WJ, Von Korff M, Lin E: Panic disorder: relationship to high medical utilization. American Journal of Medicine 92:7S-11S, 1992Google Scholar
20. Katon WJ, Roy-Byrne PP, Russo J, et al: Cost-effectiveness and cost offset of a collaborative care intervention for primary care patients with panic disorder. Archives of General Psychiatry 59:1098-1104, 2002Google Scholar
21. Steiner J, Prochazka A: The assessment of refill compliance using pharmacy records: methods, validity, and applications. Journal of Clinical Epidemiology 50:105-116, 1997Google Scholar
22. Health Plan Employer Data and Information Set (HEDIS). National Committee for Quality Assurance, 2005Google Scholar
23. Charlson ME, Pompei P, Ales KL, et al: A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. Journal of Chronic Diseases 40:373-383, 1987Google Scholar
24. Deyo R, Cherkin DC, Ciol MA: Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. Journal of Clinical Epidemiology 45:613-619, 1992Google Scholar
25. Lewis E, Marcus SC, Olfson M, et al: Patients' early discontinuation of antidepressant prescriptions. Psychiatric Services 55:494, 2004Google Scholar
26. Stein MB, Sherbourne CD, Craske MG, et al: Quality of care for primary care patients with anxiety disorders. American Journal of Psychiatry 161:2230-2237, 2004Google Scholar
27. Wang PS, Lane M, Olfson M, et al: Twelve-month use of mental health services in the United States: results from the National Comorbidity Survey Replication. Archives of General Psychiatry 62:629-640, 2005Google Scholar
28. Bull SA, Hunkeler EM, Lee JY, et al: Discontinuing or switching selective serotonin-reuptake inhibitors. Annals of Pharmacotherapy 26:578-584, 2002Google Scholar
29. Cantrell CR, Eaddy MT, Shah MB, et al: Methods for evaluating patient adherence to antidepressant therapy: a real-world comparison of adherence and economic outcomes. Medical Care 44:300-303, 2006Google Scholar
30. Ballenger JC: Anxiety and depression: optimizing treatments. Primary Care Companion to the Journal of Clinical Psychiatry 2:71-79, 2000Google Scholar
31. Altamura AC, Montresor C, Salvadori D, et al: Does comorbid subthreshold anxiety affect clinical presentation and treatment response in depression? A preliminary 12-month naturalistic study. International Journal of Neuropsychopharmacology 7:1-7, 2004Google Scholar
32. Kessler RC, Nelson CB, McGonagle KA, et al: Comorbidity of DSM-III-R major depressive disorder in the general population: results from the US National Comorbidity Survey. British Journal of Psychiatry 168(suppl 30):17-30, 1996Google Scholar
33. Roy-Byrne PP, Katon W, Cowley DS, et al: A randomized effectiveness trial of collaborative care for patients with panic disorder in primary care. Archives of General Psychiatry 58:869-876, 2001Google Scholar
34. Roy-Byrne PP, Craske MG, Stein MB, et al: A randomized effectiveness trial of cognitive behavior therapy and medication for primary care panic disorder. Archives of General Psychiatry 62:290-298, 2005Google Scholar
35. Jolis JG, Ancukiewicz M, DeLong E, et al: Discordance of databases designed for claims payment versus clinical information systems. Annals of Internal Medicine 119:844-850, 1993Google Scholar
36. Greenberg PE, Sisitsky T, Kessler RC, et al: The economic burden of anxiety disorders in the 1990s. Journal of Clinical Psychiatry 60:427-435, 1999Google Scholar



