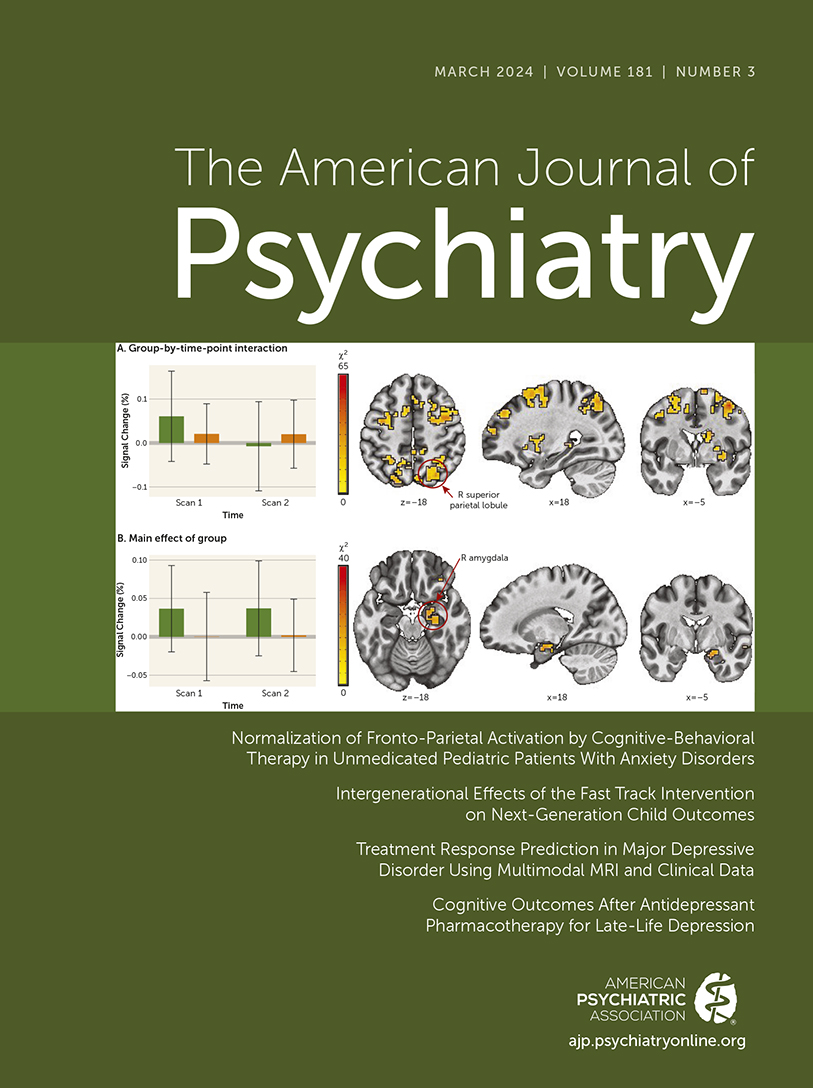
Treatment Response Prediction in Major Depressive Disorder Using Multimodal MRI and Clinical Data: Secondary Analysis of a Randomized Clinical Trial
Abstract
Objective:
Response to antidepressant treatment in major depressive disorder varies substantially between individuals, which lengthens the process of finding effective treatment. The authors sought to determine whether a multimodal machine learning approach could predict early sertraline response in patients with major depressive disorder. They assessed the predictive contribution of MR neuroimaging and clinical assessments at baseline and after 1 week of treatment.
Methods:
This was a preregistered secondary analysis of data from the Establishing Moderators and Biosignatures of Antidepressant Response in Clinical Care (EMBARC) study, a multisite double-blind, placebo-controlled randomized clinical trial that included 296 adult outpatients with unmedicated recurrent or chronic major depressive disorder. MR neuroimaging and clinical data were collected before and after 1 week of treatment. Performance in predicting response and remission, collected after 8 weeks, was quantified using balanced accuracy (bAcc) and area under the receiver operating characteristic curve (AUROC) scores.
Results:
A total of 229 patients were included in the analyses (mean age, 38 years [SD=13]; 66% female). Internal cross-validation performance in predicting response to sertraline (bAcc=68% [SD=10], AUROC=0.73 [SD=0.03]) was significantly better than chance. External cross-validation on data from placebo nonresponders (bAcc=62%, AUROC=0.66) and placebo nonresponders who were switched to sertraline (bAcc=65%, AUROC=0.68) resulted in differences that suggest specificity for sertraline treatment compared with placebo treatment. Finally, multimodal models outperformed unimodal models.
Conclusions:
The study results confirm that early sertraline treatment response can be predicted; that the models are sertraline specific compared with placebo; that prediction benefits from integrating multimodal MRI data with clinical data; and that perfusion imaging contributes most to these predictions. Using this approach, a lean and effective protocol could individualize sertraline treatment planning to improve psychiatric care.
Access content
To read the fulltext, please use one of the options below to sign in or purchase access.- Personal login
- Institutional Login
- Sign in via OpenAthens
- Register for access
-
Please login/register if you wish to pair your device and check access availability.
Not a subscriber?
PsychiatryOnline subscription options offer access to the DSM-5 library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).