County-Level Estimates of Mental Health Professional Shortage in the United States
The shortage of mental health professionals has been a persistent concern for decades ( 1 , 2 , 3 , 4 ). Most recently, the President's New Freedom Commission on Mental Health report ( 5 ) and the Institute of Medicine's report Crossing the Quality Chasm: A New Health System for the 21st Century ( 6 ) raised concerns about workforce inadequacies. The Annapolis Coalition ( 7 , 8 ) has also called for workforce development to address shortages and poor distribution of behavioral health professionals across the United States.
Most previous reports do not quantify the extent of shortages within professional groups. Quantifying mental health professional shortages can aid in describing systemic problems that are affected by shortages; such problems include bottlenecks in referral for mental health services, involvement of persons with mental illness with the justice system, homelessness, and widespread unmet need for community mental health services. Moving from identifying a shortage as a problem to quantifying it can help small areas and states in planning to meet constituents' needs. Documenting shortages may also motivate states and communities to improve recruitment, training, licensure, and retention. Even documenting an adequate supply of providers in a community can focus attention on the distribution of mental health providers between sectors. For example, mental health providers may gravitate toward employment in the private sector, leaving the public sector in extreme shortage, or they may be restricted to residential institutions (state hospitals or prisons) and may not be available to other community residents.
For a number of reasons, it has been difficult to quantify and address mental health professional shortages. National small-area data on the workforce and need have not been collected regularly. Moreover, there has been a lack of consensus about what constitutes adequate supply. This article presents an approach to quantifying shortages of mental health professionals at a small-area level for the entire United States by using nationally representative secondary data. The goals of the study were to provide a comprehensive picture of current shortages and to motivate a renewed discussion of the data improvements and practice standards required to ultimately develop an adequate workforce of mental health professionals.
Methods
Conceptualizing shortage
Mental health professional shortage was conceptualized as the percentage of need for mental health visits that was unmet within a county as of 2006. This measure improves on earlier measures ( 3 , 9 , 10 ) by taking into account variation in need as well as supply of professionals ( 11 , 12 ). Need was considered across the entire adult community, and we took into account the fact that individuals with and without serious mental illness have different levels of need. Children's needs and the mental health workforce to serve those needs have unique challenges ( 13 , 14 ) and are not addressed in this study. Supply was measured for the mental health professional workforce: psychiatrists, psychologists, advanced practice psychiatric nurses, social workers, licensed professional counselors, and marriage and family therapists. These six professions were categorized as prescribers (psychiatrists) and nonprescribers (all others) in an effort to simplify findings and still reflect this primary functional difference. Although it was recognized that other groups of professionals, such as personal aides, hypnotherapists, and registered counselors, serve people with mental health needs, we focused on major professional groups that are educated at the master's or doctoral level and licensed in most states to diagnose and treat mental disorders.
Shortage was determined at the county level across the United States. The goal was to choose a unit of analysis that reflected local planning responsibility and mental health service use as well as one for which national secondary data were available. Mental health catchment areas developed in the 1970s once served this function, but they are rarely used by states now. Because census data and workforce counts could be measured at a county level, the county was chosen as the unit of analysis.
Compiling the data
Need was estimated as provider full-time equivalents needed in each of 3,140 counties. Details are provided in a companion article in this issue ( 11 ). Separate county-level need estimates were developed for prescribers and nonprescribers, for each of two county subpopulations: adults with and without serious mental illness. County prevalence of serious mental illness was developed with the use of a synthetic estimation procedure ( 11 , 15 , 16 ). These provider need estimates were based on utilization data from the National Comorbidity Survey Replication ( 15 ) and the Medical Expenditure Panel Survey ( 17 ). For people with serious mental illness, need was measured on the basis of actual utilization among users; for those without serious mental illness, need was measured on the basis of actual utilization by the entire population. Utilization was recorded in terms of outpatient visit minutes, which were translated into provider full-time equivalents. Need estimates were deflated to adjust for the portion of need met by primary care providers, which was based on county-level area scores indicating shortage of primary care health professionals; these scores were proposed recently to the Health Resources and Services Administration (HRSA) ( 18 ). This deflation adjustment ensures that the need estimates reflect need for mental health professionals only. In summary, need estimates reflect adult need for visits to mental health professionals for every U.S. county and account for the different levels of need among people with and without serious mental illness.
Supply was estimated as provider full-time equivalents available in each county (N=3,140). Details are provided in a companion article in this issue ( 12 ). As with measures of need, separate estimates of visit minutes available were developed for prescribers (psychiatrists) and nonprescribers (psychologists, social workers, advanced practice psychiatric nurses, marriage and family therapists, and professional counselors). The data were compiled from professional associations, state licensure boards, and national certification boards in order to count all mental health professionals in both the public and private sectors for every county. Provider counts were translated into full-time equivalents based on professional practice patterns. In summary, the supply estimates reflect the full volume of met need for mental health professional visits with prescribers and nonprescribers for each U.S. county.
Each county-level need and supply estimate was adjusted with a smoothing technique to account for travel across county boundaries for mental health services. The maximum amount of time that people travel for care is about 60 minutes ( 19 , 20 ). Therefore, for a given index county, the need and supply estimates of counties within a 60-minute radius were weighted and added to the estimates for the index county. The weights were generated with an exponential distance decay function e β d , such that a county zero minutes from the index county would receive a weight of 1, and a county 60 minutes from the index county would receive a weight close to 0 (.1). Travel times were measured on the intercounty distance matrix developed at the Oak Ridge National Laboratories, which estimates the travel times between county population centroids ( 21 ). Once weighted, the estimates were further scaled so that the national need and supply totals for prescribers and nonprescribers were unchanged by the smoothing process. The choice of an hour's travel time is supported by the literature and minimizes masking of shortage (which would occur with a larger radius).
Each county's unmet need was calculated as the difference between its need and supply estimates. The shortage score represents unmet need as a proportion of total need in a county. Three scores were calculated: for prescribers, nonprescribers, and both groups combined. Prescriber and nonprescriber scores could be negative, indicating a surplus. The overall shortage score was based on the sum of positive prescriber and nonprescriber shortages. To describe the distribution of shortages across the United States, ordinary least-squares regression of overall shortage was estimated as a function of county characteristics.
Results
Over three-quarters (77%) of U.S. counties had a severe shortage of mental health prescribers or nonprescribers, with over half their need unmet. Eight percent of U.S. counties had a severe shortage of nonprescribers, with over half of their need unmet. Almost one in five counties (18%) in the nation had at least some unmet need for nonprescribers. Seventy-seven percent of U.S. counties had a severe shortage of prescribers, with over half of their need unmet. Nearly every county (96%) had at least some unmet need for prescribers. Table 1 provides statistics on the percentage of need unmet at the county level. Ordinary least-squares regression of the percentage of county overall need unmet as a function of county characteristics indicated that rurality and per capita income were the best predictors of unmet need (R 2 =.34). A 1-point increase in rurality on the 9-point Rural-Urban Continuum Code corresponded to an increase in unmet need of 3.3 percentage points. A $1,000 increase in per capita income corresponded to a decrease in unmet need of 1.3 percentage points.
 |
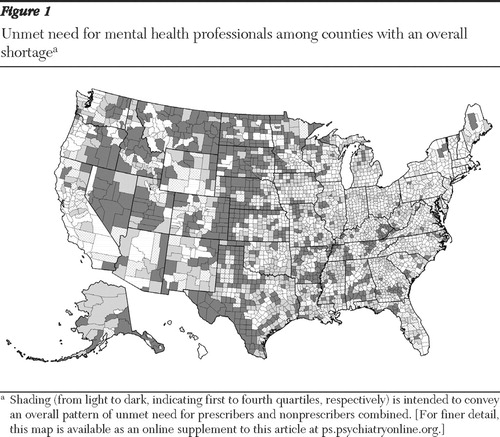
Figure 1 shows the distribution of counties with unmet need across the United States. [The map can be viewed in closer detail as an online supplement to this article at ps.psychiatryonline.org .] The percentage of need that was unmet for prescribers, nonprescribers, and overall mental health professional workforce, respectively, was grouped into quartiles. As shown, counties with a high percentage of unmet need (darkest shading) are most pronounced in a north-south strip down the middle of the country and on the eastern side of the Rocky Mountains.
Discussion
Limitations
A number of compromises had to be made in order to generate a national picture of mental health professional shortages. The HRSA, which funded this work, required a current and rational method to designate mental health professional shortage areas across the United States ( 22 ). Because of cost and time considerations, the method was based on currently available secondary data. The county-level percentage of need that is unmet provides a relative measure of shortage across counties that meets HRSA's need for a shortage designation method to target limited resources on a national level. Because our estimates of "minutes needed per person" were somewhat arbitrary and because unusual distributions can occur across dimensions other than geography (such as in residential areas and with community services), this measure of relative shortage is not well suited for measuring the absolute shortfall in a particular county.
The estimates of need were built from model-based estimates (not actual counts) of the number of people with and without serious mental illness in each county. The model predicting the prevalence of serious mental illness was derived from National Comorbidity Survey Replication (NCS-R) data ( 11 , 15 ). These data are the most current and in-depth data on mental disorders across the United States, but a number of refinements, such as a larger sample of individuals with serious mental illness and a broader sampling frame, would improve these estimates. This issue is discussed in more detail elsewhere ( 11 ). The estimates of need also rest on estimates of provider time needed by people with and without serious mental illness ( 11 ). Because standards quantifying the need for mental health treatment do not yet exist ( 23 ), the study goal was to identify a moderate standard of need for mental health services. Provider time needed was measured on the basis of utilization, and in an effort to avoid drastically underestimating time needed by individuals with serious mental illness, their need was measured on the basis of average use among service users (versus overall). Although not all people with serious mental illness require treatment at a given point in time, the estimate of provider time needed is still likely to be conservative because of suboptimal rates of service use in this group ( 24 ). The shortage measure is very sensitive to changes in the estimate of provider time needed, underscoring the importance of using shortage as a relative versus absolute measure among counties.
The supply data for mental health professionals constitute the most comprehensive, detailed, and up-to-date information on the mental health workforce of which we are aware ( 12 ). Numerous validity checks lend confidence that these data reflect the geographic distribution of mental health professionals. However, to the extent that the compilation of supply data failed to generate correct counts for counties, some counties may be ranked incorrectly in terms of unmet need. Also, it should be noted that the study excludes the fields of pastoral counseling, clinical sociology, and psychosocial rehabilitation. Many providers in these fields may be licensed in one of the included mental health professions, but some are not. Furthermore, the study was unable to distinguish providers who work only in inpatient psychiatric care. To the extent that the time of these providers is not available to community-based clients, the estimated unmet need will be too low.
The measures of unmet need are based on need and supply estimates that were smoothed with a 60-minute travel radius in order to account for travel of providers and consumers across county boundaries. A possible limitation of this smoothing technique is that it does not account for the fact that tertiary medical centers may draw people from a wider radius than other provider organizations. A larger travel radius might be more realistic in areas with such centers.
The study compromised detail for the sake of parsimony by collapsing the mental health professions into prescribers and nonprescribers. Clearly, each profession brings a unique philosophy and focus to the care and treatment of mental illness. Local treatment modalities—assertive community treatment, for example ( 25 )—can capitalize on the strengths of each profession in order to provide individualized multidisciplinary treatment. On a national scale, practice patterns and supply data are too fluid to allow the precise matching of roles with actors in each county. It is clear, however, that prescribers and nonprescribers are not functionally substitutable. This implies that need for a nonprescriber may be filled by any type of nonprescriber, whereas the need for prescribers cannot be filled by nonprescribers. In the overall measure of unmet need, prescribers and nonprescribers have equal weight, to reflect that each group plays an equally critical role in treatment. Refinements in standards of care as well as more extensive epidemiological and workforce data may shift our estimates of the relative shortages of prescribers and nonprescribers for each county and the country as a whole.
It is important to consider several issues about the delivery of mental health services that were not addressed by the estimated shortage scores. First, the need estimates and provider counts do not distinguish between public-sector services (where the greatest impairment exists) and private practice (where many consumers have less serious disorders). It is likely that the actual shortages in the public sector are greater than those in the private sector. Second, the scores do not assess the extent to which an appropriate continuum of care exists for mental health or the degree to which other needs, such as housing, are being met. Third, simply comparing estimated need with estimated supply does not address the quality of care or the degree to which professional practice is evidence based. All of these issues are important in determining whether an area's mental health services are adequate to meet the needs of residents.
The regression of shortage as a function of county characteristics is subject to mild collinearity between the independent variables, because rural areas tend to have lower per capita income (r=-.49). The equation system is also subject to endogeneity because people with serious mental illness may be attracted to live in inexpensive areas (where other low earners live), but because people with serious mental illness have low employment rates and levels of earnings, they may also contribute to the low per capita earnings of an area. Although the regression results presented here make sense intuitively, these shortcomings should be addressed in future work that explores the factors leading to professional shortage.
Implications
These findings underscore the importance of the Annapolis Coalition's ( 7 , 8 ) call for workforce development. In particular, the widespread prescriber shortage and uneven distribution of nonprescribers identified here might be lessened by following the coalition's suggestions to strengthen the workforce through development of strategies to improve recruitment, retention, education, and leadership. The coalition has also discussed the need for better mental health professional workforce data that would improve shortage estimates and support evaluation of workforce development efforts.
Small-area management entities can use this shortage information to distinguish between service gaps arising from problems in system organization and those resulting from actual shortage. Quantifying mental health professional shortage should help small areas target resources to fill workforce gaps.
Quantifying mental health professional shortage should help states justify investing in efforts to alleviate shortage and distribution problems. States are already working on a number of fronts to address mental health professional shortage. For example, consumer-centered and peer-run care increases access, continuity of care, and satisfaction ( 26 ).
Telepsychiatry to support rural mental health providers in developing treatment plans, managing medications, and following best-practice guidelines has been shown to be a way to promote distance learning and to stretch the mental health workforce to better meet needs in shortage areas ( 27 ). Integrating mental health with primary care through colocation of providers, expansion of primary care provider treatment roles, and increased opportunities for consultations between primary care clinicians and psychiatrists can improve access to mental health services, continuity, and quality of care ( 28 ).
Expanded prescriptive authority for advanced practice psychiatric nurses or psychologists also enlarges the prescriber workforce ( 29 ). Psychiatric nurses can prescribe in many states; New Mexico and Louisiana have also extended prescribing privileges to psychologists. To date, the challenges involved in acquiring additional training, setting up an independent (likely rural) practice, and establishing referral linkages have limited the impact and spread of these policies.
Many states are trying to bridge gaps through existing Medicaid policy—for example, by authorizing home- and community-based services and rehabilitation waivers ( 30 , 31 ) or by initiating Medicaid reimbursement for care management and mental health consultations ( 32 ) that expand the scope of covered services for individuals with mental illness. States are also expanding Medicaid policy through Medicaid buy-in programs that allow working adults with mental illness or other disabilities to keep their Medicaid coverage even as their earnings grow ( 33 ). A major challenge of the buy-in programs is establishing and maintaining enrollment.
Next steps for future research
Future efforts to identify mental health professional shortages would benefit from improvements in assessing both the need and the supply sides. The measurement of need should address additional populations such as persons with co-occurring substance use disorders, children, homeless adults, and those who are linguistically isolated. The measurement of supply should address the expanded practice scope of nurses and psychologists and should include additional professions (such as psychosocial rehabilitation).
Although we recognize that data refinements come at a high cost, there are several that would greatly improve the data for use in generating shortage scores, even staying within the data framework currently available ( 11 , 12 ). The NCS-R data are the most current and in-depth data on mental disorders across the United States, but a number of refinements are desirable. These include a larger sample of individuals with serious mental illness, a broader sampling frame that includes people who are homeless or living in institutions, consistent handling of psychotic and other disorders, and a more thorough measurement of race and income. The supply data on mental health professionals constructed for this report represent the most comprehensive, detailed, and up-to-date information on the mental health workforce now available. Yet to the extent that the data compilation failed to generate correct counts for counties, some counties may receive inaccurate shortage scores. Better supply data would be comprehensive, consistent, and without duplication.
Conclusions
Three-quarters of U.S. counties were estimated to have a severe shortage of prescribers, with over half their need unmet, ten times the number with a severe shortage of nonprescribers. Nearly all (96%) U.S. counties were found to have at least some prescriber shortage, whereas only 18% were found to have any nonprescriber shortage. Comprehensive standards of care, more extensive epidemiological data, and investment in a national workforce database would greatly improve these shortage estimates. But the big challenge for future work is to progress from simply describing shortages to overcoming them.
Acknowledgments and disclosures
This work was supported by contract HHSH-230200532038C from the HRSA. The authors acknowledge the help of the project officer, Andy Jordan, M.S.P.H.; their advisory board, which included Michael Almog, Ph.D., David Bergman, J.D., Tim Dall, M.S., Sheron R. Finister, Ph.D., John C. Fortney, Ph.D., Nancy P. Hanrahan, Ph.D., R.N., Sharon M. Jackson, M.S.W., L.C.S.W., Nina Gail Levitt, Ed.D., Ronald W. Manderscheid, Ph.D., Noel A. Mazade, Ph.D., Bradley K. Powers, Psy.D., Richard M. Scheffler, Ph.D., Laura Schopp, Ph.D., Lynn Spector, M.P.A., Marvin S. Swartz, M.D., and Joshua E. Wilk, Ph.D.; and the following individuals: Rick Harwood, Marlene Wicherski, Jessica Kohout, Ph.D., Lynn Bufka, Ph.D., Becky Corbett, A.C.S.W., Charles Housen, Tracy Whitaker, Ph.D., Paul Wing, Ph.D., Jim Fitch, Scott Barstow, Emily Wisniewski, Mark Holmes, Ph.D., Tom Ricketts, Ph.D., Jennifer Groves, M.B.A., Randy Randolph, M.P.R., Olivia Silber Ashley, Dr.P.H., Bob Bray, Ph.D., J. Valley Rachal, Ph.D., Tina McRee, M.A., Harold Goldsmith, Ph.D., Barbara Van Horne, M.B.A., Ph.D, Edward Norton, Ph.D., Gary Koch, Ph.D., Robert McConville, Sarah Curtis, Ph.D., Bruce Peterson, M.S., Susan Shafer, M.Ed., Susanne Phillips, M.S.N., F.N.P., Linda Beeber, Ph.D., R.N., Victoria Soltis-Jarrett, Ph.D., A.P.R.N.-B.C., and Cheryl Jones, Ph.D., R.N. The views expressed in this report do not necessarily reflect the official policies of the U.S. Department of Health and Human Services, nor does mention of organizations imply endorsement by the U.S. Government.
The authors report no competing interests.
1. Moritz T: A state perspective on psychiatric manpower development. Hospital and Community Psychiatry 30:775–777, 1979Google Scholar
2. Tucker G, Turner J, Chapman R: Problems in attracting and retaining psychiatrists in rural areas. Hospital and Community Psychiatry 32:118–120, 1981Google Scholar
3. Sierles F, Taylor M: Decline of US medical student career choice of psychiatry and what to do about it. American Journal of Psychiatry 152:1416–1426, 1995Google Scholar
4. Goldman W: Is there a shortage of psychiatrists? Psychiatric Services 52:1587–1589, 2001Google Scholar
5. Achieving the Promise: Transforming Mental Health Care in America. Pub no SMA-03-3832. Rockville, Md, Department of Health and Human Services, President's New Freedom Commission on Mental Health, 2003Google Scholar
6. Institute of Medicine: Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC, National Academies Press, 2001Google Scholar
7. An Action Plan for Behavioral Health Workforce Development. Cincinnati, Ohio, Annapolis Coalition on the Behavioral Health Workforce, 2007. Available at www.annapoliscoalition.org Google Scholar
8. Hoge MA, Morris JA, Stuart GW, et al: A national action plan for workforce development in behavioral health. Psychiatric Services 60:883–887, 2009Google Scholar
9. Baldwin LM, Patanian MM, Larson EH, et al: Modeling the mental health workforce in Washington State: using state licensing data to examine provider supply in rural and urban areas. Journal of Rural Health 22:50–58, 2006Google Scholar
10. Holzer C, Goldsmith H, Ciarlo J: The availability of health and mental health providers by population density. Journal of the Washington Academy of Sciences 86:25–33, 2000Google Scholar
11. Konrad TR, Ellis AR, Thomas KC, et al: County-level estimates of need for mental health professionals in the United States. Psychiatric Services 60:1307–1314, 2009Google Scholar
12. Ellis AR, Konrad TR, Thomas KC, et al: County-level estimates of mental health professional supply in the United States. Psychiatric Services 60:1315–1322, 2009Google Scholar
13. Koppelman J: The provider system for children's mental health: workforce capacity and effective treatment. National Health Policy Forum Issue Brief 26:1–18, 2004Google Scholar
14. Thomas CR, Holzer CE: The continuing shortage of child and adolescent psychiatrists. Journal of the American Academy of Child and Adolescent Psychiatry 45:1023–1031, 2006Google Scholar
15. Kessler RC, Berglund P, Chiu WT, et al: The US National Comorbidity Survey Replication (NCS-R): design and field procedures. International Journal of Methods in Psychiatric Research 13:69–92, 2004Google Scholar
16. Census 2000 Public Use Microdata Sample (PUMS). Washington, DC, US Census Bureau, 2003Google Scholar
17. Cohen J: Methodology Report #1: Design and Methods of the Medical Expenditure Panel Survey Household Component. Rockville, Md, Agency for Health Care Policy and Research, 1997. Available at www.meps.ahrq.gov/data_files/publications/mr1mr1.shtml Google Scholar
18. Ricketts TC, Goldsmith LJ, Holmes GM, et al: Designating places and populations as medically underserved: a proposal for a new approach. Journal of Health Care for the Poor and Underserved 18:567–589, 2007Google Scholar
19. Fortney JC, Owen R, Clothier J: Impact of travel distance on the disposition of patients presenting for emergency psychiatric care. Journal of Behavioral Health Services Research 26:104–108, 1999Google Scholar
20. Fortney J, Rost K, Zhang M, et al: The impact of geographic accessibility on the intensity and quality of depression treatment. Medical Care 37:884–893, 1999Google Scholar
21. County-to-County Distance Matrix. Oak Ridge, Tenn, Oak Ridge National Laboratory, Center for Transportation Analysis, 2006. Available at cta.ornl.gov/transnet/SkimTree.htm Google Scholar
22. Morrissey JP, Thomas KC, Ellis AR, et al: Development of a new method for designation of mental health professional shortage areas. Unpublished report prepared under contract HHSH-230200532038C with the Bureau of Health Professions, Health Resources and Services Administration, Department of Health and Human Services, 2007. Available at mh.shepscenter.unc.edu/publications/index.html#mhpsa Google Scholar
23. Kessler R, Berglund P, Glantz J, et al: Estimating the prevalence and correlates of serious mental illness in community epidemiological surveys; in Mental Health, United States, 2002. Edited by Manderscheid RW, Berry JT. DHHS pub no (SMA) 04-3938. Rockville, Md, Substance Abuse and Mental Health Services Administration, 2004Google Scholar
24. Kessler R, Berglund P, Bruce M, et al: The prevalence and correlates of untreated serious mental illness. Health Services Research 36:987–1007, 2001Google Scholar
25. Phillips S, Burns B, Edgar E, et al: Moving assertive community treatment into standard practice. Psychiatric Services 52:771–779, 2001Google Scholar
26. Davidson L, Chinman M, Kloos B, et al: Peer support among individuals with severe mental illness: a review of the evidence. Clinical Psychology: Science and Practice 6:165–187, 1999Google Scholar
27. O'Reilly R, Bishop J, Maddox K, et al: Is telepsychiatry equivalent to face-to-face psychiatry? Results from a randomized controlled equivalence trial. Psychiatric Services 58:836–843, 2007Google Scholar
28. Katon W, VonKorff M, Lin E, et al: Stepped collaborative care for primary care patients with persistent symptoms of depression: a randomized trial. Archives of General Psychiatry 56:1109–1115, 1999Google Scholar
29. Hartley D, Hart V, Hanrahan N, et al: Are Advanced Practice Psychiatric Nurses a Solution to Rural Mental Health Workforce Shortages? Working paper 31. Portland, Maine Rural Health Research Center, 2004. Available at muskie.usm.maine.edu Google Scholar
30. Daly R: Iowa Medicaid to cover skills training for disabled. Psychiatric News, May 18, 2007, p 17Google Scholar
31. Promising practices: using the Medicaid "Rehab Option" to serve working people with mental illness. National Consortium for Health Systems Development e-News, Mar 2005Google Scholar
32. Medicaid Service Definitions Approved by CMS: Changes to North Carolina's Medicaid Service Definitions for the "Enhanced Benefit Services for Mental Health and Substance Abuse" Public Policy Update. Raleigh, NC, Mental Health Association in North Carolina, Feb 3, 2006. Available at www.mha-nc.org/english/index.php/component/option,com_vfm/Itemid,92/dir,Public+Policy|Year+2006 Google Scholar
33. Ireys H, Davis S, Andrews K: The Interaction of Policy and Enrollment in the Medicaid Buy-In Program. Washington, DC, Mathematica Policy Research, 2007Google Scholar



