Applying Functional Imaging to Clinical Practice: Are We Making Progress Toward Its Promise?
With the introduction in 1919 of pneumoencephalography, brain imaging promised to change how we manage neurologic and psychiatric disease. Fortunately, better, less invasive, and less painful imaging methods were developed, moving psychiatric imaging through X-ray, computed tomography, single-photon emission computed tomography, positron emission tomography, and especially, in the past three decades, magnetic resonance imaging. In particular, the advent of increasingly sophisticated MRI techniques led many investigators, including me, to predict more than two decades ago that these technologies would change how we practice (1). We posited that MRI and other imaging techniques would finally provide objective measures of psychiatric conditions (diagnoses), would define the underlying neuropathology causing the illness (etiology), and establish measures to predict and personalize treatment. These promises have not been realized (2).
Nonetheless, there are hints at progress. In many common conditions, neuroimaging is producing functional neuroanatomic models of psychiatric illnesses that provide testable hypotheses toward etiology and diagnosis. In mood disorders, namely, major depressive and bipolar disorders, these models may represent useful endophenotypes for genetic and other analyses (3). Particularly in the past decade, MRI has been increasingly applied to identifying functional neuroanatomic associations with treatment response. Although results remain mixed and are rarely replicated, it is within this context that the article in this issue by Dunlop et al. (4) advances the field.
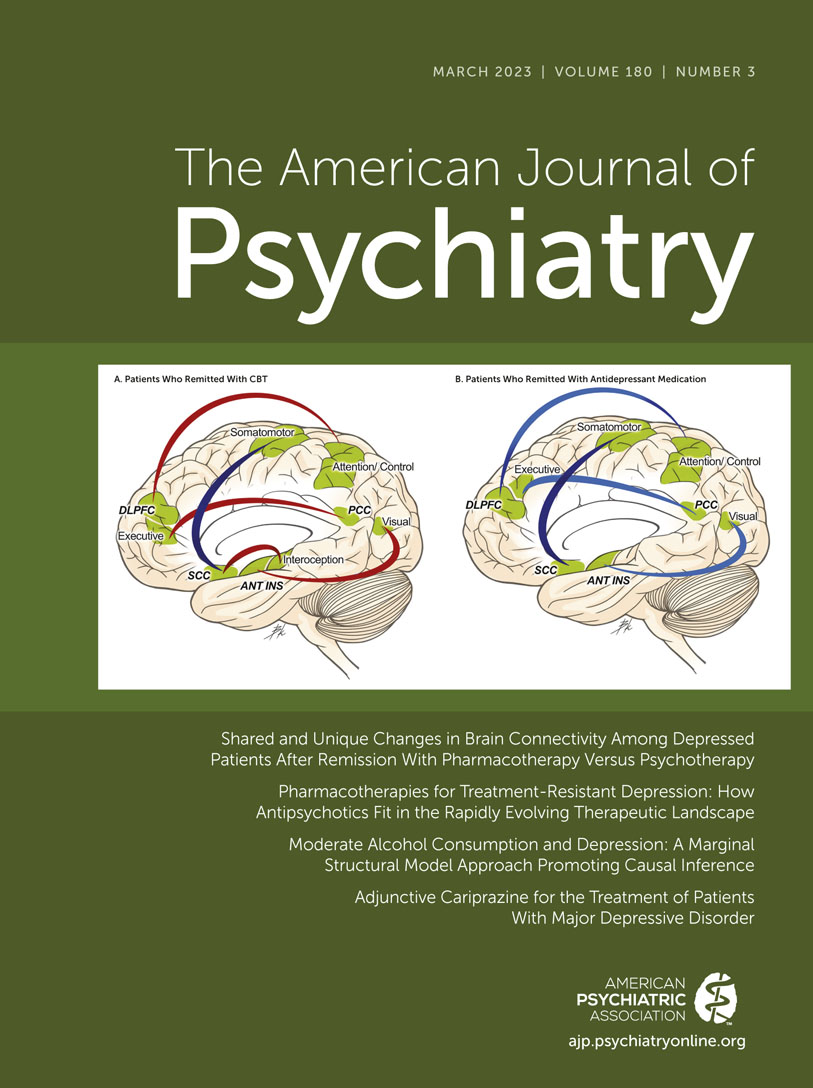
In their study, Dunlop and colleagues applied functional MRI (fMRI) techniques to explore how antidepressant medication and cognitive-behavioral therapy (CBT) altered functional connectivity, similarly and differently, within commonly described resting-state networks in individuals with major depression. Specifically, they focused on the default mode, executive control, salience, and anterior limbic networks, as these networks each have reports of associations with major depressive disorder. The study assessed changes during a 12-week treatment trial (PReDiCT) (5) of 40 participants who received CBT, 91 who received either duloxetine or citalopram, and 35 healthy comparison subjects. Concurrent with the treatment trial, baseline and end-of-treatment resting-state fMRI acquisitions were obtained to measure changes in functional connectivity from seed regions within these defined networks. The numbers of people assessed makes this study one of the larger within-subject treatment response investigations in major depressive disorder.
As with all studies, several limitations must be considered when interpreting the results. The questions asked, and at times the analytic approach (e.g., whole brain voxel-wise analysis), are inherently exploratory (hypothesis generating) rather than hypothesis testing at the network level. Relatedly, the study assumes that a single small region-of-interest seed represents a broad network—for example, that a small portion of the posterior cingulate cortex represents uniquely and singularly the default mode network. It is unlikely that this assumption is completely correct (6). An alternative approach is to specifically examine multiple functional connectivities among predefined regions of interest within the putative network, in order to test specific hypotheses about network function. Such an approach is much more labor intensive, however, so less commonly used, yet it can produce network models of change. Nonetheless, these concerns are typical in clinical human imaging research; they largely reflect the state of the art, in which exploratory study designs and analytic approaches continue to dominate the field. Only by altering this approach can exploratory findings lead to improvements in clinical practice and in our understanding of the pathophysiology of major depression.
In the Dunlop et al. study, the changes observed within the executive control network that were associated with improvement during CBT were the most robust findings. These results supported the study’s hypothesis, have significant face validity linked to the putative mechanisms of CBT, showed significant associations with symptom changes, and fit within existing functional neuroanatomic models of major depressive disorder, especially as related to dorsolateral prefrontal cortical function (7). These results provide a strong substrate for further hypothesis refinement and testing in future CBT-neuroimaging investigations in major depression. In contrast, the findings associated with medication therapy were much less robust, and did not support the study’s hypothesis that antidepressant treatment would lead to reduced default mode network connectivity, and so they provide unclear directions for next steps. Finally, the finding that treatment to remission overall (across groups) is “only” significantly linked to changes in functional connectivity between nonoverlapping (across treatments) regions of the subcallosal cingulate cortex and a limited region of motor cortex is difficult to interpret. This nonintuitive finding highlights the limits of voxel-wise whole-brain exploratory analyses. Specifically, it remains poorly defined how best to provide sufficient statistical power while adequately controlling for multiple comparisons, not just within each individual brain, but across and within subjects. Consequently, the likelihood of “significant” spurious findings that are not replicable remains high. Indeed, if this association is truly the “most important” functional change in the treatment of major depression, then existing models require substantial revision. This finding, then, must be interpreted cautiously.
Nonetheless, the robust findings linked to CBT are particularly notable given the wide age range of the participants, which crossed several critical neurodevelopmental periods that likely impact resting-state network connectivities (8), and the inherent heterogeneity of major depression. Major depression is a ubiquitous condition that may represent a psychiatric “end state” in response to a wide range of etiologies. As my colleagues and I discussed previously (9), nearly any event that impacts brain function is associated with an elevated risk of depression, including nearly all, if not all, psychiatric conditions, most neurologic conditions, many drugs that cross the blood-brain barrier, a wide variety of medical conditions, and especially childhood trauma (10). Since these many etiologies likely contribute to depression risk through multiple and separate neural pathways, the relatively specific CBT findings of the Dunlop et al. study suggest that this treatment works broadly on the depressive “end state” to change individuals’ functional neuroanatomy to relieve symptoms.
As well described by Weinberger and Radulescu (2), resting-state fMRI studies have inherent limitations that complicate interpretability. The major concern is that it is difficult to ascertain what the individual (and the individual’s brain) is actually doing when instructed to simply stare at a fixation point or not think about anything or simply rest. Temporal correlations of activation measures in brain regions within putative resting-state networks are not rigidly fixed, so they likely change in response to a variety of circumstances that are hard to understand in the absence of behavioral measures. Meaningful differences within individuals over time, lost in group contrasts, have been described in resting-state research, raising additional questions about the meaning of group-averaged findings at any given time point (11). Consequently, within a specific individual the experiences of the day, expectations, fatigue levels, and other unknown factors all may impact the temporal relations underlying functional connectivity measures (2, 11). In the absence of behavioral measures to understand what might mediate functional connectivity changes and behavior (i.e., symptom expression), as used in task-based fMRI investigations, interpretation of group differences in resting-state measures to predict treatment response in an individual may be limited. The uptake of resting-state fMRI into the research community was rapid, and differences in resting-state networks have been observed between nearly all psychiatric groups and healthy subjects, although these findings have been difficult to replicate (2). Nonetheless, the relatively robust findings within the CBT treatment arm of the Dunlop et al. study further support this approach as a basis for next steps in understanding how CBT mediates changes to alleviate depressive symptoms.
The world of psychiatric neuroimaging is replete with exploratory studies and relatively few successful replications (2). Although the study by Dunlop et al. primarily adds to the former, unlike many previous reports, it provides a specific framework and findings that define specific hypothesis testing. For example, one possible next step might be to narrow the depressive phenotype (e.g., by age range or family depression history) and then use functional imaging not only to replicate these resting-state findings but to extend them by designing a study to specifically test a hypothesized role of the dorsolateral prefrontal cortex within the executive control network while measuring cognitive skills acquisition during the scan using task-based fMRI. This simple example could further improve models of major depression, help define subgroup differences across models, and clarify more directly how treatment impacts brain function. Dunlop et al. thus advance the field by moving us closer to using neuroimaging to help guide treatment decisions and predict treatment response while better understanding the neurobiology of major depression. As similar studies emerge from this work, we may finally realize the promise of neuroimaging in psychiatry for which many of us are waiting.
1. : Volumetric MRI studies of mood disorders: do they distinguish unipolar and bipolar disorder? Bipolar Disord 2002; 4:80–88Crossref, Medline, Google Scholar
2. : Finding the elusive psychiatric “lesion” with 21st-century neuroanatomy: a note of caution. Am J Psychiatry 2016; 173:27–33Link, Google Scholar
3. : Integration and consolidation: a neurophysiological model of bipolar disorder, in The Bipolar Brain: Integrating Neuroimaging and Genetics, 2nd ed. Edited by Strakowski SM. New York, Oxford University Press, 2022, pp 281–308 Google Scholar
4. : Shared and unique changes in brain connectivity among depressed patients after remission with pharmacotherapy versus psychotherapy. Am J Psychiatry 2023; 180:218–229Link, Google Scholar
5. : Predictors of Remission in Depression to Individual and Combined Treatments (PReDiCT): study protocol for a randomized controlled trial. Trials 2012; 13:106Crossref, Medline, Google Scholar
6. : A critical role for the right fronto-insular cortex in switching between central-executive and default-mode networks. Proc Natl Acad Sci U S A 2008; 105:12569–12574Crossref, Medline, Google Scholar
7. : Large-scale network dysfunction in major depressive disorder: a meta-analysis of resting-state functional connectivity. JAMA Psychiatry 2015; 72:603–611Crossref, Medline, Google Scholar
8. : The older adult brain is less modular, more integrated, and less efficient at rest: a systematic review of large-scale resting-state functional brain networks in aging. Psychophysiology 2023; 60:e14159Crossref, Medline, Google Scholar
9. : Is depression simply a nonspecific response to brain injury? Curr Psychiatry Rep 2013; 15:386Crossref, Medline, Google Scholar
10. : The devastating clinical consequences of child abuse and neglect: increased disease vulnerability and poor treatment response in mood disorders. Am J Psychiatry 2020; 177:20–36Link, Google Scholar
11. : Person-specific and precision neuroimaging: current methods and future directions. Neuroimage 2022; 263:119589Crossref, Medline, Google Scholar