New Findings Relevant to Substance Use Disorders
Substance use disorders are highly prevalent and frequently comorbid with other psychiatric illnesses. Despite this, these disorders are commonly underdiagnosed and ineffectively treated. To update our readers and bring attention to their importance, this issue of the Journal focuses on the latest findings related to substance use disorders—their developmental consequences, genetic underpinnings, neuroimaging correlates, and treatment. Three editorials accompany the primary research articles, including one by Dr. Kathleen Brady, an expert in substance abuse and comorbid psychiatric disorders and a new Deputy Editor of the Journal.
From a developmental perspective, we learn from one study about the long-term negative cognitive consequences of cannabis use during adolescence. In highlighting this study, Dr. Philip Harvey, an expert on cognition and functioning in psychiatric illnesses, provides an in-depth look at the importance and public health concerns of the effects of cannabis on cognition. We also learn from a study in this issue that pregnancy may be a factor that protects women from developing an alcohol use disorder.
Two studies featured in this issue address the genetic and molecular underpinnings of substance use disorders. In the first, we are presented with a molecular mechanism that involves variation in a specific gene that partially underlies the stress-associated risks for substance abuse. In the second, we learn that there may be differences in the genetic underpinnings of alcohol consumption compared with those for problematic drinking, and that problematic drinking has shared genetics with such psychopathologies as schizophrenia, bipolar disorder, major depressive disorder, and attention deficit hyperactivity disorder. Dr. Jonathan Pollock, who leads the Genetics, Epigenetics, and Developmental Neuroscience Branch at the National Institute on Drug Abuse, provides an instructional piece focused on these findings while more broadly considering the fundamentals of the genetic and epigenetic mechanisms underlying alcohol use disorders.
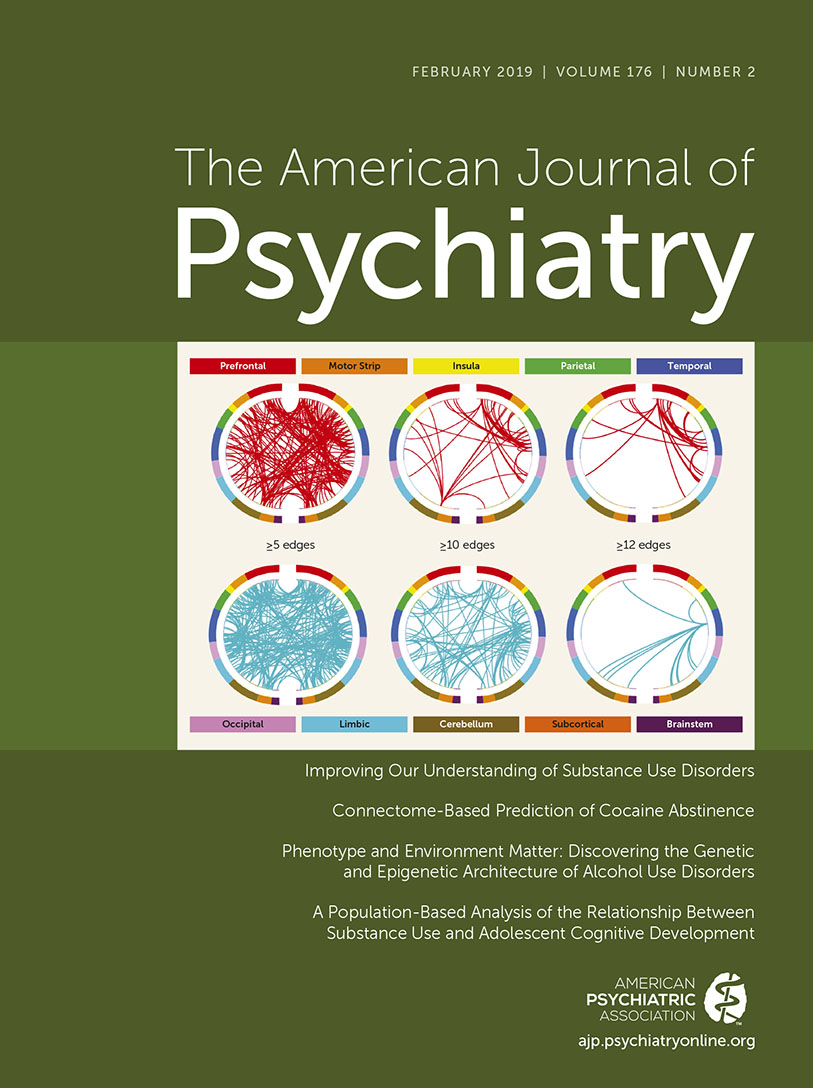
This issue also features three studies that employ imaging methods to address neural issues relevant to substance abuse. First, a “mega-analysis” defined alterations in gray matter volume both in general and also specific to different substances. Insula and medial orbitofrontal cortical volumes appeared to be affected across all substances that were assessed. In the second, functional connectivity neuroimaging along with machine learning found that connectivity within and between networks involving executive control and reward responsiveness predicted treatment-related cocaine abstinence. The third study addresses important pragmatic treatment issues in relation to opioid use disorder: a randomized clinical trial found that in combination with behavioral therapy, significantly enhanced treatment retention was reported for individuals taking extended-release injectable naltrexone compared with oral administration.
Taken together, the articles in this issue represent novel and potentially important findings relevant to the understanding and treatment of substance use disorders. Our intention is to use the Journal to continue to emphasize new findings and treatment-related developments in relation to addictions and substance use disorders. It is our hope that this information will provide neuroscientific rationales for researchers and clinicians as they work to reduce the suffering that results from these potentially devastating disorders.