Effect of Acute Antidepressant Administration on Negative Affective Bias in Depressed Patients
Abstract
Objective: Acute administration of an antidepressant increases positive affective processing in healthy volunteers, an effect that may be relevant to the therapeutic actions of these medications. The authors investigated whether this effect is apparent in depressed patients early in treatment, prior to changes in mood and symptoms. Method: In a double-blind, placebo-controlled, between-groups randomized design, the authors examined the effect of a single 4-mg dose of the norepinephrine reuptake inhibitor reboxetine on emotional processing. Thirty-three depressed patients were recruited through primary care clinics and the community and matched to 31 healthy comparison subjects. Three hours after dosing, participants were given a battery of emotional processing tasks comprising facial expression recognition, emotional categorization, and memory. Ratings of mood, anxiety, and side effects were also obtained before and after treatment. Results: Depressed patients who received placebo showed reduced recognition of positive facial expressions, decreased speed in responding to positive self-relevant personality adjectives, and reduced memory for this positive information compared to healthy volunteers receiving placebo. However, this effect was reversed in patients who received a single dose of reboxetine, despite the absence of changes in subjective ratings of mood or anxiety. Conclusions: Antidepressant drug administration modulates emotional processing in depressed patients very early in treatment, before changes occur in mood and symptoms. This effect may ameliorate the negative biases in information processing that characterize mood and anxiety disorders. It also suggests a mechanism of action compatible with cognitive theories of depression.
Cognitive psychological models of depression emphasize the importance of negative biases in information processing in the etiology and maintenance of depressive disorders (1) . Experimental evidence suggests that depressed patients are more likely to remember negative than positive emotional information in self-relevant tasks (2 , 3) and to interpret key social signals, such as facial expressions of emotion, as either more negative or less positive than do matched healthy volunteers (4 – 6) . Such effects have been linked to increased risk of relapse (4) and are thought to fuel negative thinking and low mood in depression (1) .
We recently hypothesized (7) that antidepressant drug treatments may produce their ultimate clinical effects by normalizing these negative biases in information processing. Indeed, healthy volunteers show early effects of antidepressants on emotional processing even in the absence of subjective changes in mood. For example, a single dose of the norepinephrine reuptake inhibitor reboxetine was found to increase the recognition of happy facial expressions, speed responses to positive self-referent information, and facilitate memory for these positive personality characteristics (8) . Similar effects on the recognition of happy facial expressions have been seen with acute administration of both the serotonin reuptake inhibitor citalopram (9 , 10) and the serotonin and norepinephrine reuptake inhibitor duloxetine (11) , which suggests that such changes in emotional processing may be a common effect of pharmacological treatments effective in the management of depression. Early effects of antidepressants on emotional processing may contribute to later changes in mood and symptoms as the patient learns to respond to this new and more positive intra- and interpersonal environment.
The early effects of antidepressant treatment on emotional processing have been characterized in healthy volunteer samples. However, it is not known whether these early changes in emotional processing also occur during the treatment of acutely depressed patients, and if so, whether they are of a magnitude similar to those seen in healthy volunteers. In this study, we examined the effect of a single dose of reboxetine compared to placebo on emotional processing in a sample of unmedicated patients with major depression and matched healthy comparison subjects. The same three measures of emotional processing found to be affected by antidepressant administration in healthy volunteers were used here (8 , 12) . We hypothesized that acutely depressed patients would show negative biases on these measures compared to healthy volunteers when receiving placebo. This would be manifested as lower recognition of happy facial expressions, lower speed in identifying positive versus negative self-descriptors, and lower recall for positive personality descriptors. Administration of reboxetine was predicted to reverse these effects and lead to increased positive emotional processing on these same measures in the absence of changes in mood.
Method
Participants and Study Design
We studied 33 acutely depressed patients (mean age, 37 years [SD=12.0, range=18–61], 15 of them male) and 31 age- and gender-matched healthy volunteers (mean age, 37 years [SD=12.5, range=20–64], 15 of them male). All patients had been medication free for at least 3 months. Participants were screened with the Structured Clinical Interview for DSM-IV (13) . Patients were recruited through primary care clinics and through advertisements in the local area. The healthy volunteers were recruited through the same advertisement process. The depressed patients all met criteria for a primary DSM-IV diagnosis of major depressive disorder. None of the healthy volunteers met criteria for a current diagnosis or a history of any axis I disorder. The study was approved by the Oxford Research Ethics Committee, and all participants gave written informed consent.
All participants completed the neuroticism subscale of the Eysenck Personality Questionnaire–Revised (14) , the Liebowitz Social Anxiety Scale (15) , and the trait measure of the State-Trait Anxiety Inventory (STAI; 16 ) at screening to characterize the sample. On the test day, mood and anxiety were measured with the Beck Depression Inventory (BDI; 17 ), the Hamilton Depression Rating Scale (HAM-D; 18 ), the Befindlichkeits Scale of Mood and Energy (19) , and the STAI. These were given before administration of medication, and the STAI and Befindlichkeits Scale were repeated 3 hours later. The Befindlichkeits Scale is a self-report measure that is sensitive to both normal and clinical variation in mood. Participants are presented with 56 pairs of adjectives and asked to choose the one that best describes their current mood (e.g., desperate versus hopeful; lively versus lifeless). It is suitable for repeated administration and can be used meaningfully in both depressed and nondepressed individuals.
Participants were stratified for gender and randomly allocated to one of two treatment conditions in a double-blind design: reboxetine given as a single oral 4-mg dose or matched placebo. Testing began 3 hours after medication administration. At the completion of the study, patients were referred back to the care of their general practitioner. If, however, there was concern over their clinical condition or if it was felt that they would benefit from longer-term specialist care, they were referred to an appropriate service within the Oxfordshire Mental Health Trust.
Facial Expression Recognition
The facial expression recognition task featured six basic emotions—happiness, surprise, sadness, fear, anger, and disgust—taken from 10 individual characters from the Pictures of Facial Affect series (20) , which had been morphed between each prototype and neutral (21) . Briefly, this procedure involved taking a variable percentage of the shape and texture differences between the two standard images—0% (neutral) and 100% (full emotion)—in 10% steps. Four examples of each emotion at each intensity were presented (6 emotions × 10 intensities × 4 examples = 240 stimuli). Each face was also presented in a neutral expression (10 stimuli), giving a total of 250 stimulus presentations. The facial stimuli were presented in random order on a computer screen for 500 msec and replaced by a blank screen. Participants made their responses by pressing one of seven labeled keys on the keyboard. Participants were asked to respond as quickly and as accurately as possible. To prevent fatigue, a break of 1–2 minutes was given halfway through the task (after 125 face presentations). Recognition threshold (the intensity level required for successful recognition of each emotion) was designated as the level of emotional intensity at which participants correctly identified 75% or more of the facial expressions of emotion for four consecutive intensities. Reaction times (in msec) for correct responses were also measured in this task.
Emotional Categorization and Memory
Emotional categorization task
Sixty personality characteristics selected to be disagreeable (e.g., domineering, untidy, and hostile) or agreeable (e.g., cheerful, honest, and optimistic) (taken from reference 22) were presented on the computer screen for 500 msec each. These words were matched in terms of word length, ratings of usage frequency, and meaningfulness. Volunteers were asked to categorize these personality traits as likable or dislikable as quickly and as accurately as possible. Specifically, they were asked to imagine whether they would be pleased or upset if they overheard someone else referring to them as possessing this characteristic, so that the judgment was in part self-referring. Classifications and reaction times for correct identifications were computed for this task.
Emotional memory
Fifteen minutes after completion of the emotional categorization task, participants were asked to recall as many of the personality traits as possible. This task allowed the assessment of incidental memory for positive and negative characteristics. The numbers of positive and negative words recalled were computed and analyzed for both hits (correct responses) and intrusions (false responses).
Statistical Analysis
To establish the effects of depression per se, each task was first analyzed for the placebo-treated participants alone by group (depressed patients versus comparison subjects) as the between-subjects factor. For performance in the emotional categorization task and memory, valence (positive or negative) was an additional within-subjects factor. Next, the effects of the drug manipulation were assessed using analysis of variance with drug treatment (reboxetine or placebo) and group (depressed patients or comparison subjects) as between-subjects factors and emotion (positive or negative) as the within-subjects factor, as above. Statistically significant interactions were followed up with simple analyses for group differences.
Results
Group Matching and Subjective State
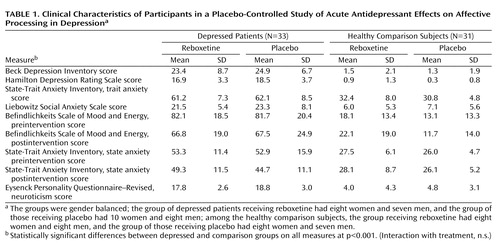
The depressed patients and healthy volunteers did not differ in terms of age, years of education, or gender. As expected, patients scored higher than healthy volunteers on the subjective ratings of depression, low mood, and anxiety, but there were no differences between patients assigned to receive reboxetine and those assigned to receive placebo ( Table 1 ).
Acute administration of reboxetine had no effect on mood or anxiety in either the patients or the healthy volunteers after 3 hours ( Table 1 ).
Facial Expression Recognition
Effects of depression
Depressed patients showed reduced perception of facial expressions of happiness (F=4.8, df=1, 31, p=0.036) and surprise (F=4.7, df=1, 31, p=0.037) compared to the healthy volunteers in the absence of differences in the recognition of the other emotions ( Figure 1 , left panel, and Table 2 ). There was also no effect of depression on speed of correct responses (all p values >0.1), which suggests that differences in recognition of positive facial expressions could not be accounted for by speed-accuracy trade-offs.

a Recognition of happiness (y-axis) is measured in terms of accuracy scores, which reflect the threshold to detect each emotion, presented here as 100 minus the threshold value, so that a higher score indicates better performance. Comparison of depressed patients receiving placebo and comparison subjects receiving placebo significant at p<0.05; comparison of depressed patients receiving placebo and depressed patients receiving reboxetine significant at p<0.01.
Effects of drug
Reboxetine facilitated the recognition of happy facial expressions across the depressed patient and comparison groups (main effect of drug: F=8.0, df=1, 60, p=0.006; drug-by-group: F=2.0, df=1, 60, p=0.2). This effect of reboxetine was apparent when considering the depressed patients alone ( Figure 1 , right panel; F=8.4, df=1, 31, p=0.007), which supports early effects of antidepressant drug administration in this group. There was no effect of drug on the recognition of the other facial expressions or on reaction times of correct responses (all p values >0.16) ( Table 2 ).
Emotional Categorization
Data for two participants (one volunteer and one patient) were missing for this task because of a technical error.
Effects of depression
As expected, the depressed patients took longer to respond specifically to the positive self-referent items in this task compared to the healthy volunteers ( Figure 2 ), confirming the presence of negative bias in this task (group-by-emotion: F=5.9, df=1, 29, p=0.021; speed to identify positive items: t=3.3, df=29, p=0.003).

a Comparison of reaction time to positive stimuli between depressed patients and comparison subjects receiving placebo significant at p<0.01; comparison between depressed patients receiving placebo and those receiving reboxetine significant at p<0.05 (emotion × group interaction).
Effects of drug
Reboxetine decreased time to respond to the positive versus negative self-referent items in this task (drug-by-emotion, F=3.9, df=1, 58, p=0.05) in both the depressed patients and healthy volunteers (interaction with patient group across all comparisons not significant). This effect of reboxetine was still apparent when the depressed group was considered alone (F=10.3, df=1, 30, p=0.003), again confirming that this group is sensitive to acute administration of reboxetine ( Figure 2 ).
Emotional Memory
Effects of depression
Depressed patients showed worse recall of personality descriptors in this task (main effect of group: F= 5.3, df=5, 29, p=0.029; group-by-emotion: F=3.1, df=1, 29, p=0.09), which was particularly evident for the recall of positive items (positive recall: t=2.7, df=29, p=0.01; negative recall: t=0.9, df=29, p=0.4) ( Figure 3 ).
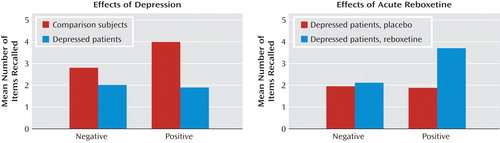
a Comparison for positive stimuli between depressed patients and comparison subjects receiving placebo significant at p<0.05; comparison for positive stimuli between depressed patients receiving placebo and those receiving reboxetine significant at p<0.01.
Effects of drug
Reboxetine improved memory for positive items in this task, but this was apparent only in the depressed patient group (emotion-by-group-by-drug group: F=5.4, df=1, 58, p=0.028; emotion-by-drug for depressed patients: F=4.6, df=1, 30, p=0.03; emotion-by-drug for comparison subjects: F=1.3, df=1, 28, p=0.3) ( Figure 3 ).
Discussion
Our findings indicate that acute administration of an antidepressant can modify emotional processing in acutely depressed patients. Under placebo conditions, the depressed patients showed reduced recognition of positive facial expressions, decreased speed to respond to positive self-relevant personality adjectives, and reduced memory for this positive information compared to matched healthy volunteers. However, a single dose of reboxetine reversed these effects in the absence of changes in subjective ratings of mood or anxiety. The magnitude of the effects of reboxetine on emotional processing was either similar or larger in the depressed patients relative to the healthy volunteers. These results therefore validate our previous findings from healthy volunteer groups (8 – 12) and suggest that the same effects are seen in depression early on in treatment with antidepressant drugs.
The reduced positive affective processing seen here in unmedicated depressed patients is consistent with cognitive theories that emphasize the role of such biases in underlying etiology (1 , 23) . Similar to the results we present here, previous studies have also reported reduced recognition of positive facial expressions and/or increased recognition of aversive facial expressions in depressed patients, as well as negative biases in self-referent emotional memory (for a review, see reference 24 ). This replication indicates that our emotional processing tasks are sensitive to the negative emotional biases that are characteristic of the depressed state. It is remarkable that the effects of reboxetine were almost exactly the converse of the effects of depression, suggesting that antidepressants could work by targeting the negative and often implicit biases in emotional processing that are believed to characterize and maintain the disorder.
The therapeutic effect of antidepressant treatment requires time and repeated administration to become clinically apparent. This is often taken to prove that the key neurobiological change may also be delayed in some way. In fact, this interpretation of clinical trial data and clinical experience may be less soundly based than is often assumed. The rate of improvement in depressive symptoms over the first week of treatment with a selective serotonin reuptake inhibitor (SSRI) is at least as great as in subsequent phases of treatment (25) . This could imply that the causal change takes place immediately and sets in train a process with a fixed time course. It is therefore striking that effects of antidepressant treatment on emotional processing in depressed patients can be seen even with a single administration of half the daily dose recommended for treatment. We have hypothesized that the critical time lag in antidepressant drug action does not result solely from a delay in relevant neuropharmacological actions, such as desensitization of autoreceptors or the requirement for neurogenesis (7) . Instead, we suggest that there is an inherent delay between the effects of antidepressants on emotional processing and the subsequent effects on mood. According to this view, effects of antidepressants on emotional bias are seen rapidly, but the translation of these changes into improved subjective mood takes time as the patient learns to respond to this new, more positive social and emotional perspective of the world (7) . An increased tendency to interpret social signals as positive may not immediately lead to improved mood but could reinforce social participation and social functioning, which over repeated experience improve mood and the other symptoms of depression. This does not exclude a critical role for delayed neuropharmacological effects, but the therapeutic delay before clinical benefit does not prove their existence, as is often assumed.
Negative biases in information processing in depression and anxiety are the explicit target for psychological treatments such as cognitive-behavioral therapy (CBT) (1) . The actions of antidepressant treatment are not usually explored in a psychological framework, and reductions of biases toward aversive information following antidepressant treatment are often attributed to mood improvement. However, our results show that antidepressants change emotional processing and memory in depression very early on in treatment and in the absence of a measurable change in subjective mood. These results therefore suggest that cognitive theories of depression may also be relevant to antidepressant drug action, with different treatments having the potential to affect similar underlying processes. Indeed, researchers have reported overlapping as well as distinct effects of CBT and antidepressant drug treatment on cerebral blood flow in neuroimaging studies (26 , 27) , which supports the idea that there may be some commonalities in their neural mechanisms of action. The challenge now remains to explore such effects early on in treatment to help us understand to what extent these approaches are similar prior to the induction of clinical changes in mood state.
This study has a number of limitations. Although the depressed patients in our sample all met criteria for a current episode of DSM-IV depression, symptom severity fell within the mild to moderate range largely because of the need to recruit an unmedicated sample. The negative biases seen in these patients validates this approach, but further studies are required to replicate these effects in a larger and more severely affected group, also allowing for correlation analyses to be performed between clinical ratings and emotional processing performance. It is also unknown whether similar effects are seen early on in the treatment of depressed patients with other antidepressant drugs, including the more commonly used SSRIs. A recent meta-analysis suggests that reboxetine may be less effective in the treatment of depression than other second-generation antidepressants (28) , which may seem to contrast with the robust effects seen here in the experimental medicine model, although there is also evidence that such clinical observations with reboxetine are partly a consequence of poor tolerability and high dropout rates rather than reduced efficacy (29) . Further study is nonetheless required to assess whether this experimental medicine approach can discriminate between agents with different levels of efficacy early on in treatment and whether those agents that perform well in the clinic are also those with the strongest early effects on emotional processing measures.
The significant effects on emotional processing that we have seen in depressed patients after a single dose of reboxetine raise the possibility that models of emotional processing may be useful in drug development and screening. If acute effects in emotional processing measures are seen reliably with effective antidepressants in depressed patients, then performance in these models may be a useful way of screening novel candidate antidepressant agents before full-scale clinical trials are initiated (30) . It is also possible that individual effects on these measures could be used to predict eventual response in depressed patients starting treatment. Consistent with this, increased recognition of happy facial expressions after 1 week of treatment with citalopram in depressed patients predicted eventual therapeutic response after 6 weeks of continued treatment (31) . Such findings highlight a potentially critical role for early changes in emotional bias in therapeutic efficacy.
1. Beck AT, Rush AJ, Shaw BF, Emery G: Cognitive Therapy of Depression. New York, Guilford, 1979Google Scholar
2. Bradley BP, Mogg K, Williams R: Implicit and explicit memory for emotion-congruent information in clinical depression and anxiety. Behav Res Ther 1995; 33:755–770Google Scholar
3. Bradley B, Mathews A: Negative self-schemata in clinical depression. Br J Clin Psychol 1983; 22:173–181Google Scholar
4. Bouhuys AL, Geerts E, Gordijn MC: Depressed patients’ perceptions of facial emotions in depressed and remitted states are associated with relapse: a longitudinal study. J Nerv Ment Dis 1999; 187:595–602Google Scholar
5. Gur RC, Erwin RJ, Gur RE, Zwil AS, Heimberg C, Kraemer HC: Facial emotion discrimination, II: behavioral findings in depression. Psychiatry Res 1992; 42:241–251Google Scholar
6. Surguladze SA, Young AW, Senior C, Brebion G, Travis MJ, Phillips ML: Recognition accuracy and response bias to happy and sad facial expressions in patients with major depression. Neuropsychology 2004; 18:212–218Google Scholar
7. Harmer CJ: Serotonin and emotional processing: does it help explain antidepressant drug action? Neuropharmacology 2008; 55:1023–1028Google Scholar
8. Harmer CJ, Hill SA, Taylor MJ, Cowen PJ, Goodwin GM: Toward a neuropsychological theory of antidepressant drug action: increase in positive emotional bias after potentiation of norepinephrine activity. Am J Psychiatry 2003; 160:990–992Google Scholar
9. Harmer CJ, Bhagwagar Z, Perrett DI, Vollm BA, Cowen PJ, Goodwin GM: Acute SSRI administration affects the processing of social cues in healthy volunteers. Neuropsychopharmacology 2003; 28:148–152Google Scholar
10. Murphy S, Norbury R, O’Sullivan U, Cowen PJ, Harmer CJ: Effect of a single dose of citalopram on amygdala response to emotional faces. Br J Psychiatry 2009; 194:535–540Google Scholar
11. Harmer CJ, Heinzen J, O’Sullivan U, Ayres RA, Cowen PJ: Dissociable effects of acute antidepressant drug administration on subjective and emotional processing measures in healthy volunteers. Psychopharmacology (Berl) 2008; 199:495–502Google Scholar
12. Harmer CJ, Shelley NC, Cowen PJ, Goodwin GM: Increased positive versus negative affective perception and memory in healthy volunteers following selective serotonin and norepinephrine reuptake inhibition. Am J Psychiatry 2004; 161:1256–1263Google Scholar
13. Spitzer RL, Williams JBW, Gibbon M, First MB: Structured Clinical Interview for DSM-IV (SCID). New York, New York State Psychiatric Institute, Biometrics Research, 1995Google Scholar
14. Eysenck SBG, Eysenck HJ, Barrett P: A revised version of the psychoticism scale. Pers Individ Dif 1985; 6:21–29Google Scholar
15. Liebowitz MR: Social phobia. Mod Probl Pharmacopsychiatry 1987; 22:141–173Google Scholar
16. Spielberger CD, Gorsuch RL, Lushene RD: STAI Manual. Palo Alto, Calif, Consulting Psychologists Press, 1970Google Scholar
17. Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J: An inventory for measuring depression. Arch Gen Psychiatry 1961; 4:561–571Google Scholar
18. Hamilton M: A rating scale for depression. J Neurol Neurosurg Psychiatry 1960; 23:56–62Google Scholar
19. von Zerrsen D, Strian F, Schwarz D: Evaluation of depressive states, especially in longitudinal studies, in Psychological Measurements in Psychopharmacology. Edited by Pichit P. Basel, Switzerland, Karger, 1974, pp 189–202Google Scholar
20. Ekman P, Friesen WV: Pictures of Facial Affect. Palo Alto, Calif, Consulting Psychologists Press, 1976Google Scholar
21. Young AW, Rowland D, Calder AJ, Etcoff NL, Seth A, Perrett DI: Facial expression megamix: tests of dimensional and category accounts of emotion recognition. Cognition 1997; 63:271–313Google Scholar
22. Anderson NH: Likableness ratings of 555 personality trait words. J Pers Soc Psychol 1968; 9:272–279Google Scholar
23. Bower GH: Mood and memory. Am Psychol 1981; 36:129–148Google Scholar
24. Leppanen JM: Emotional information processing in mood disorders: a review of behavioral and neuroimaging findings. Curr Opin Psychiatry 2006; 19:34–39Google Scholar
25. Taylor MJ, Freemantle N, Geddes JR, Bhagwagar Z: Early onset of selective serotonin reuptake inhibitor antidepressant action: systematic review and meta-analysis. Arch Gen Psychiatry 2006; 63:1217–1223Google Scholar
26. Kennedy SH, Konarski JZ, Segal ZV, Lau MA, Bieling PJ, McIntyre RS, Mayberg HS: Differences in brain glucose metabolism between responders to CBT and venlafaxine in a 16-week randomized controlled trial. Am J Psychiatry 2007; 164:778–788Google Scholar
27. Goldapple K, Segal Z, Garson C, Lau M, Bieling P, Kennedy S, Mayberg H: Modulation of cortical-limbic pathways in major depression: treatment-specific effects of cognitive behavior therapy. Arch Gen Psychiatry 2004; 61:34–41Google Scholar
28. Cipriani A, Furukawa TA, Salanti G, Geddes JR, Higgins JP, Churchill R, Watanabe N, Nakagawa A, Omori IM, McGuire H, Tansella M, Barbui C: Comparative efficacy and acceptability of 12 new-generation antidepressants: a multiple-treatments meta-analysis. Lancet 2009; 373:746–758Google Scholar
29. Papakostas GI, Nelson JC, Kasper S, Möller HJ: A meta-analysis of clinical trials comparing reboxetine, a norepinephrine reuptake inhibitor, with selective serotonin reuptake inhibitors for the treatment of major depressive disorder. Eur Neuropsychopharmacol 2008; 18:122–127Google Scholar
30. Dawson GR, Goodwin G: Experimental medicine in psychiatry. J Psychopharmacol 2005; 19:565–566Google Scholar
31. Tranter R, Bell D, Gutting P, Harmer C, Healy D, Anderson IM: The effect of serotonergic and noradrenergic antidepressants on face emotion processing in depressed patients. J Affect Disord (Epub ahead of print, Feb 26, 2009)Google Scholar