Developments in the Epidemiology of Drug Use and Drug Use Disorders
Abstract
The past 30 years of research on the epidemiology of drug use, drug use disorders, and related conditions, such as HIV, has provided major insight into these conditions. Drug use peaked in the late 1970s, decreased across the 1980s, increased in the 1990s, and has remained stable during the past few years. Within this broad pattern, specific epidemics of crack cocaine, amphetamines, club drugs (such as Ecstasy), heroin, and prescription opioids and associated epidemics of HIV and other infectious diseases have been identified and tracked. Besides major accomplishments in surveillance, the epidemiology of drug use and drug use disorders has traditionally focused on identifying risk factors at the individual (genetic factors, high-risk behaviors), family (child abuse), neighborhood (high availability of drugs), and societal (policies and laws) levels as domains of influence, not as components of interrelated processes. Research includes careful cross-sectional and longitudinal observational studies as well as clinical epidemiological experiments in which prevention interventions test specific etiological theories. Building on this background, the next challenges for the epidemiology of drug use and drug use disorders will be to link individual vulnerabilities with specific environmental factors by using multilevel methodological approaches. For example, what are the environmental factors that interact with individual vulnerabilities to produce drug addictions and drug consequences such as HIV? Research in genetic epidemiology has demonstrated the potential for studies of interactions of genetic and environmental factors. The field needs to focus on linking science with epidemiology to make progress in understanding these complex health conditions.
The future of epidemiology of drug use and drug use disorders depends on the successful application of integrated approaches to studying complex human behaviors. Such a goal of studying multifactorial models is consistent with current trends in epidemiology (1) and builds on the rich history of the epidemiology of drug use and drug use disorders by incorporating perspectives from molecular genetics and neuroscience into individual and social epidemiology. By integrating these diverse transdisciplinary approaches, both prevention and treatment of drug use and drug use disorders may be enhanced (2).
Progress in the epidemiology of drug use and drug use disorders over the past several decades has been substantial, and a comprehensive review is beyond the scope of this article. The selected major accomplishments reviewed here center around the systematic and regular monitoring of large-scale shifts in the landscape of drug use, the prevalence and timing of the onset of illicit drug use, the estimation of drug use disorders in the United States, the identification of substantial comorbidity between drug use and drug use disorders with mental disorders, and the linking of drug use, especially injection drug use and high-risk sexual behaviors, to the spread of HIV. Furthermore, this article highlights some underused research approaches that, when embedded within epidemiological studies, hold promise of making major advances in our understanding of the complex nature of drug use and drug use disorders.
Background
The purpose of epidemiology, broadly stated, is the “study of the distribution and determinants of health-related states or events in specified populations, and the application of this study to control of health problems” (3). When this definition has been applied to drug use and drug use disorders, epidemiology has historically served as a foundation for understanding the nature and extent of drug use, abuse, and dependence in the population; for informing basic, clinical, treatment, and services research; and for developing prevention strategies. Over the past several decades, the epidemiology of drug use and drug use disorders has developed within two major veins: descriptive and analytic. Descriptive studies characterize and describe the distribution of drug use and drug use disorders according to time, place, person, and groups of people. Analytic studies test specific hypotheses linking drug use and drug use disorders to putative causes, such as exposure to drugs, opportunities for drug use, social-environmental risk factors, and individual characteristics, including genetic and biological factors.
Observations about the overall United States from the general population National Survey on Drug Use and Health (formerly called the National Household Survey on Drug Abuse) and the Monitoring the Future Study’s survey of students indicate shifts in the landscape of illicit drug use over the past 30 years (4, 5). Illicit drug use in the United States escalated in the 1970s, decreased in the 1980s, increased again around 1992, reached a relative peak around 1997, and has subsequently leveled off or, in some cases, declined. This overall trend is most typical for marijuana because, as the most commonly used drug, changes in its prevalence tend to drive the trends for the “any illicit drug” index. The Monitoring the Future Study has also documented an association between beliefs about drugs and the use of drugs. For example, beliefs about the harmfulness of marijuana are inversely related to the prevalence of use of the substance (Figure 1). Documenting and describing the relationship among these variables is one of the goals of the Monitoring the Future Study.
Although the major national surveys document, in the most general sense, similar trends in drug use across the last decades, important distinctions between the surveys and discrepancies in their findings demonstrate certain principles in epidemiology (as in all of science), namely, that multiple methods and approaches to a problem may be needed to obtain a full view. One major issue is the very sampling frame. Whereas the Monitoring the Future Study surveys only youth who attend school and are in grades 8, 10, or 12, the National Survey on Drug Use and Health includes only the civilian population ages 12 and older who are housed in residences and noninstitutional group quarters. Among youth, the Monitoring the Future Study routinely yields higher estimates of tobacco, alcohol, and illicit drug use than the National Survey on Drug Use and Health, a difference attributed largely to data collection in schools rather than in households. In addition, methodological differences in the way that questions are asked of respondents may play a role in the differences between them (6). What are we to make of these differences? How does a clinician or a scientist make sense of the inconsistencies? In fact, just such inconsistencies argue for the use of different sources of information. The weaknesses of school-based methods are that these surveys can only adequately cover a certain age range and only youth attending school. For the household surveys, coverage of the full range of ages is possible, but some of the populations of most interest are not included, such as homeless or incarcerated people. Additional studies of these other populations are needed for a complete picture of drug use.
Despite variance in the absolute rates found in the major surveys, systematic monitoring of drug use in the United States indicates that illicit drug use is very common and typically begins during adolescence. The 2002 National Survey on Drug Use and Health data indicate that approximately 46%—an estimated 108 million individuals—have tried an illicit drug at least once in their lives, 40% have used marijuana, and 30% have used other illicit drugs (5). Reflecting the emergence of substance use in adolescence, the 2003 Monitoring the Future Study found that 23% have tried an illicit drug by the eighth grade, 41% by the 10th grade, and 51% by the 12th grade (4). Marijuana is by far the most commonly used illicit drug, with 18% of eighth-graders, 36% of 10th-graders, and 46% of 12th-graders reporting having ever tried marijuana (4). A nearly universal finding is that drug use increases from adolescence to young adulthood then gradually declines. Thus, adolescence marks a period of risk for the onset of drug use.
Another key finding derived from the surveillance studies is that the number of illicit users of prescription drugs has been increasing in recent years (5). In particular, the past few years have seen a marked increase in the use of opioid medications (such as oxycodone and hydrocodone) but an even greater increase in problems associated with such use (7). Other changes of concern in recent years have included an increase in marijuana abuse and dependence (especially among younger black and Hispanic people), possibly related to an increase in marijuana’s potency (8), an increased availability of high-purity heroin, an increase in heroin use by smoking and other noninjection routes (9), an increase in initial use of 3,4-methylenedioxymethamphetamine (MDMA or Ecstasy) (5), an expansion of the use of “club drugs” other than Ecstasy, including ketamine and gamma-hydroxybutyrate (9), a decline in the use of LSD (4), and stabilization and some signs of decline in the use of cocaine (4).
One of the major goals of descriptive epidemiology is to document the distribution of disease across groups to inform policy and research. For example, as shown in Figure 2, drug use and drug use disorders are distributed across the major race/ethnic groups in approximately the same proportions as these groups are represented in household populations. However, when some of the most serious consequences of drug use are examined—namely, imprisonment and AIDS among injection drug users—African American and Hispanic populations are markedly overrepresented. Epidemiology can draw attention both to similar rates of drug use and disorders among different groups and to the major health disparity issue of overrepresentation of certain minority populations in criminal justice settings and among injection drug users with AIDS. In response to these high rates, both research and policy are being modified (12, 13).
Comorbidity
Large-scale epidemiological surveys have also shown that drug use disorders—drug abuse or drug dependence—are prevalent and characterized by substantial comorbidity with mental disorders. Most recently, by using the criteria of DSM-IV, the National Epidemiological Survey on Alcohol and Related Conditions showed that 10.3% of the adult U.S. population (ages 18 and over) had a lifetime history of any drug use disorder, with 7.7% and 2.6% having drug abuse and drug dependence, respectively (14). In addition to demonstrating high prevalence, two decades of epidemiological research on drug use disorders provides consistent and overwhelming evidence of comorbidity with diverse forms of psychopathology. Findings from the Epidemiologic Catchments Area (ECA) study (15), the National Comorbidity Survey (16), the National Longitudinal Alcohol Epidemiologic Survey (17), the International Consortium in Psychiatric Epidemiology (18), and the National Epidemiologic Survey on Alcohol and Related Conditions (19) have each shown that mood, anxiety, and personality disorders are strongly associated with drug use disorders.
Moreover, epidemiological studies of various types converge to suggest that the association between psychiatric and drug disorders is etiologically meaningful. Epidemiological surveys of adults have consistently shown that anxiety, mood, and antisocial personality disorders are more strongly associated with drug dependence than drug abuse (20–22). Recent reports from the National Epidemiologic Survey on Alcohol and Related Conditions (unpublished study by K.P. Conway et al.; reference 23) found, for example, that the odds ratio between lifetime psychiatric and drug use disorders was higher for drug dependence than drug abuse for any anxiety disorder (4.9 and 1.7, respectively), any mood disorder (7.1 and 2.3, respectively), and antisocial personality disorder (16.7 and 5.4, respectively). Retrospective accounts of information of age at onset from such surveys have informed the temporal ordering of some of these associations. Analyses from the ECA show that the risk of substance abuse in adulthood increases with each conduct problem endorsed before age 15 (24), thereby suggesting a dose-dependent relation. Longitudinal epidemiological studies have been particularly informative by tracing the development of psychopathology and drug involvement over time. Lewinsohn and colleagues (25) reported that adolescents classified as former or current daily smokers, compared to smokers who never smoked on a daily basis, were more likely to have a history of major depression (odds ratio=2.5) or conduct/oppositional defiant disorder (odds ratio=3.9). Breslau and colleagues (26) found that both current and past smoking were associated with an onset of major depression in people ages 15 and older, whereas only current smoking was associated with an onset of panic disorder, agoraphobia, and substance use disorders. Findings from the Pittsburgh Youth Study (27) indicate that higher levels of attention deficit hyperactivity disorder and conduct disorder predict higher levels of marijuana use from ages 13 to 18.
Clinical Epidemiology
Epidemiological findings such as these have helped construct an empirical basis for randomized field trials designed to test hypothesized mechanisms of association in prevention studies designed as experimental or clinical epidemiology. For example, prevention studies might test ideas about possible mechanisms behind “gateway” relationships—the observation that when individuals try cigarettes or alcohol, a portion of them subsequently use marijuana, and some of those who have used marijuana then go on to use other drugs, such as hallucinogens, cocaine, or heroin (28, 29). Consistent with this observation, the average ages at first use among initiates in 2000 were 16.0 years for cigarettes, 16.2 years for alcohol, 16.6 years for marijuana, and 20.4 years for cocaine (5). The question is whether use of “harder” drugs is caused by the use of so-called “gateway substances” or merely reflects the manifestation of an underlying tendency to use drugs of all sorts, as evidenced in the use of the gateway substance. In fact, whether gateway drugs cause the later drug use remains a controversial hypothesis with mixed empirical support (30, 31).
On the other hand, another major theory concerning the relationship of early problem behaviors to later drug use has been empirically supported by prevention trials in which early childhood interventions were associated with attenuated onset of adolescent drug use. In one such study, Kellam and Anthony (32) found that boys who were assigned to a 2-year behavior-improving classroom program, compared to boys assigned to usual classroom environments, were less likely to begin smoking cigarettes in early adolescence. In another study, Hawkins and colleagues (33) showed that an intervention focusing on school and family bonding in early childhood can have a long-lasting salutary effect on the onset of drug use. Although more research is required, particularly of a longitudinal nature, to determine the effects of such interventions on the progression to drug use disorders (34), these studies simultaneously provide potentially useful prevention interventions and rigorous tests of etiological hypotheses about drug use risk factors.
Genetic Epidemiology
One major subdiscipline of epidemiology is genetic epidemiology, a field that seeks to identify genetic and environmental influences on disease. Indeed, of the various risk factors for drug use disorders, family history has been identified as the most potent and consistent. Results from family studies show that drug use disorders are prevalent in families (35, 36), and twin and adoption studies demonstrate that much of the familial clustering of drug use disorders can be explained by genetic factors (37, 38). Several controlled family studies demonstrate that substance abuse or dependence in probands (i.e., the index case in genetically informative designs) is associated with a substantial increase in risk for these disorders among first-degree adult relatives (37) and among offspring (39), as well as on premorbid risk factors believed to be predictive of the development of substance abuse (40, 41). Furthermore, risk is conferred both generally across the various classes of illicit drugs and by particular drug classes (42, 43). Of importance, genetic epidemiological studies of drug use disorders have yielded results that are compelling in terms of consistency, magnitude of relative risk, and coherence of the message that drug use disorders have genetic and environmental underpinnings in need of further explication. For example, genetic factors appear to be more strongly associated with drug use disorders than drug use (44). This finding has implications for the prevention of onset of use of drugs compared to the prevention of progression from use to addiction in that genetics may be important for the identification of people at risk for drug use disorders, whereas the prevention of onset of drug use is much more likely to be based on environmental manipulation. No matter the implications, missing from our studies is information on the specific genes and their distribution in populations of interest. Because we have not yet been successful in determining the specific genes involved in the transmission of drug use disorders, the usual epidemiological measures of prevalence and distribution cannot yet be calculated.
What is apparent is that drug use disorders are genetically and phenotypically complex disorders that result from the interplay between underlying genetic susceptibility and environmental risk. Like many other relatively common human diseases, drug use disorders are now believed to arise from multiple genes exerting small effects, gene-by-gene interactions, gene-by-environment interactions, and/or a host of environmental factors and risk-conferring behaviors (45). Because the identification of gene-by-environment interactions is likely to prove key to understanding the etiology of complex disorders (46, 47), advances in this important area will benefit from large prospective genetically informative studies drawn from community sources.
Social Epidemiology
Despite the multifactorial etiology of drug use and drug use disorders conceptualized in several broad theories, research on drug use and drug use disorders has focused largely on individual risk factors at the expense of an understanding of the interaction of broader and interrelated factors. When multiple contributive factors have been considered, the emphasis has commonly been on additive models of predispositional factors, and these models have typically concentrated on factors from a single domain—i.e., the biological, the behavioral, or the environmental. Comprehensive reviews have been written to identify empirically derived risk and protective factors for drug problems (48). There is also evidence linking the number of risk factors with the magnitude of risk, whether additively (49), multiplicatively (50), or interactively (51).
To better understand the epidemiology of drug use and its consequences within and across populations, research must focus on the influence of social and cultural factors on the initiation and progression of drug use among population groups. Novel conceptualization and measurement of social and cultural contexts within theoretically grounded research are suggested because increased understanding of how genetic, biological, social, and contextual phenomena interact to influence behavior will inform prevention and treatment for individuals at risk for drug use and drug use disorders (52). For instance, parent drug use may influence child development through direct and indirect pathways. Direct pathways include genetic transmission of vulnerability to drug use disorders and environmental exposure to drugs either in utero or in the home. Indirect pathways include child abuse and neglect or other stressful environments caused by the drug-using lifestyle. Many of these factors emanate from or are reinforced by norms and behaviors of family members and other significant people (including peers, authority figures, public figures, etc.), intervening processes, such as collective socialization and peer-group influence, as well as social and institutional processes (49, 53–55). Neighborhood and community-level variables also may serve as risk or protective factors—i.e., residential instability, collective efficacy, social cohesion, or other aspects of locally shared environments as contributors to drug-abusing behaviors (56, 57).
In other words, the social environment is something of a sphere that encompasses the many factors interacting with individual characteristics (58, 59), and research targeted at understanding the interactions of individual and social environmental influences with community-level factors requires particular attention. For example, why certain population groups and communities have particularly high rates of drug use and related disorders is a key question. Therefore, further studies of drug use and drug use disorders should examine the interaction of individual and social environmental factors on drug use, abuse, and dependence, including both immediate and cumulative (life course and transgenerational) effects.
Drug use disorders are particularly clear examples of human disorders that pose great challenges because they are familial and heritable but do not follow Mendelian patterns of inheritance (60, 61). And while the quest persists for the reliable detection of risk-conferring genes for drug use disorders, success in this endeavor and in the identification of gene-by-environment interactions will hinge, in part, on the systematic conceptualization and categorization of the environment and by linking developmental psychology, genetic epidemiology, and neuroscience (61). Social epidemiology should be added to the list of essential disciplines that can enrich this critical discussion. In many ways, the guiding principles of social epidemiology naturally complement the methods of genetic epidemiology, particularly family studies that extend across multiple generations.
Future Directions
Although epidemiological studies have proven to be very valuable for describing drug use patterns across person, place, and time; for identifying factors associated with increased (or decreased) risk for drug use and drug use disorders; and for testing specific hypotheses regarding putative causes, the specific processes through which such factors confer risk remain unclear. Thus, many fundamental questions remain unanswered. For example, although early drug use signals poor prognosis for many individuals, it remains uncertain why some drug users desist while others persist in greater drug involvement and drug addiction. Second, despite decades of research documenting comorbidity between psychiatric and drug use disorders, there is a pressing need for research into the specific mechanisms that underlie comorbidity. Third, despite an overwhelming consistency of results showing that drug use disorders are familial and, at least in part, genetically influenced, little has been learned about how and under which conditions such liability manifests itself.
To address these needs, large-scale epidemiological studies are uniquely capable of advancing research through the “nesting and testing” of hypothesized measures of causal mechanisms within ongoing epidemiological studies. At present, laboratory and clinical research are often conducted in isolation from epidemiological research, and epidemiological evidence is often not incorporated into laboratory and clinical research. Since much of what we know about liability to drug use and drug use disorders is based on clinical samples, a significant potential exists for selection bias, with resulting reduction in the generalizability of findings. Epidemiological studies offer unique, powerful, and efficient opportunities for addressing this concern by embedding (“nesting”) hypothesized measures of causal mechanisms into existing studies and substudies. In addition, epidemiological evidence can be used to inform the selection of participants for laboratory-based research. Study designs that efficiently combine the advantages of epidemiological samples with more intensive laboratory-based and biological measures are also cost-efficient.
Clearly, one of the key challenges for epidemiology will be to harness selected measures from neurobiology that can be applied in general population studies. For example, given a focus on adolescence as the key period of risk for drug use and drug use disorders, measures of gonadarche, adrenarche, and pubertal growth can be assessed (62). In addition, through study in representative samples, the relationship of brain development during adolescence to cognitive and emotional development and to the onset of drug use and drug use disorders may be examined (63). Such work will require conceptual integration of epidemiological studies, with basic science studies of animal brain development where certain details can be examined that cannot be examined in humans. In addition, measures that are already appropriate for epidemiological studies on select subsets of subjects include neuroimaging, serum samples for metabolic studies (63), and biological specimens for genetic association studies. For example, as the technology for obtaining genetic material through mouthwashes and/or cheek swabs improves, applying such techniques at reasonable costs in broad samples is possible (64).
Further advances in the epidemiology of drug use and drug use disorders will also require the development and application of innovative methods in statistical, epidemiological, sociological, and genetic epidemiological study designs. Promising new techniques include ecological momentary assessment tools that capture information nearly at the time of its occurrence with novel recording devices, such as personal digital assistants or cell phones (65). Statistical innovations are needed to maximize the use of longitudinal, prospective, multidisciplinary studies because they must account for the interactions among biological (including genetic), psychosocial, and contextual factors. Statistical innovations, such as the recently developed growth mixture modeling (66), should address transitions in the stages and trajectories of drug use, as well as drug use over the life course and the intergenerational transmission of drug use and its consequences. Of note, increases in the numbers of older persons and possible increases in drug use and drug use disorders in these populations may necessitate new work on elderly populations (67). Innovative analytic approaches will be required to identify homogeneous subgroups of drug users that emerge from the complex variety of indicators (68). Moving into the study of interactions across domains of factors—genetic/environment, individual susceptibility/social environment, neighborhood environment as an effect modifier—provides great promise for the next generation of research on drug use and drug use disorders.
In focusing on environmental influences, emphasis should be placed on augmenting existing population studies, both cross-sectional and longitudinal. For example, whereas national surveys can provide important information about trends in the prevalence of drug use, they provide limited information about factors that lead to differences in drug use outcomes across communities (69). Typical survey studies, such as the National Survey on Drug Use and Health (5), the Monitoring the Future Study (4), the Youth Risk Behavior Survey (70), and the National Epidemiologic Survey on Alcohol and Related Conditions (19) might be augmented with or compared to community-level research to examine relatively rare drug use (e.g., heroin), regional variations, pockets of drug use, emerging trends in drug use, and certain high-risk groups not living in permanent households.
Conclusions
Epidemiology provides a foundation for much research on drug use and drug use disorders by demonstrating on whom, through what agents, and where drugs exert their effects. Through population-based studies, key clues are identified for detailed exploration in analytic epidemiological studies and in nonepidemiological studies. There are, however, limitations to epidemiological research. Large sample sizes can pose difficulties in terms of resources to obtain the needed intensive and detailed measures, particularly over extended periods. Also, the observational nature of much epidemiological research limits experimental control and manipulation of the variables under study. Thus, epidemiological studies have the maximum impact when linked with basic science and clinical experimental studies in a thoughtful program of investigation.
It is clear that the future of the epidemiology of drug use and drug use disorders holds great promise. First, because of strong environmental effects, drug use requires monitoring on a reasonably frequent basis, with additional efforts to identify emerging trends or new drugs. But such monitoring is only one purpose of epidemiology. The second main activity is to test hypotheses and rule in or out certain plausible hypotheses. Once the epidemiological studies have been conducted, more detailed methods can then be applied.
In both of these areas, clinical implications are profound. Regarding descriptive factors, the preexisting rates of drug use and disorders in certain populations change the differential diagnoses in clinical settings. For example, paranoid psychosis may increase in the face of phencyclidine use in a particular community. This implies that clinicians need to be aware of the local trends in their area as well as the particular subgroups with unusually high rates of specific substances. For clinicians, the second goal of epidemiology, testing etiological hypotheses, also has clinical implications. For example, as we have learned that adolescence is a key period of risk for the onset of drug use and drug disorders, adolescent treatment is being expanded (71). In addition, the relationship of family function to drug use and drug use disorders serves as the underpinnings to successful family-based interventions for adolescent drug use disorders (72, 73).
As the field of epidemiology moves into an integrative era (1), the epidemiology of drug use and drug use disorders can be at the forefront. The goal is to determine how social factors, exogenous agents, and individual factors are linked across time to produce illness. Achieving this goal will require refinement of existing methods and development of new techniques for classifying the individual and the environment. The knowledge obtained from studies of these topics will improve the nation’s public health by promoting integrated approaches to understanding and addressing interactions between individuals and environments that contribute to the continuum of problems related to drug use. The goal is to marry elements of sampling methods, biological measures, and qualitative analysis of social networks to better explain the dynamics of disease transmission. These approaches will allow us to develop scientific knowledge with clear application to practice and public policy.
Presented in part at the 157th annual meeting of the American Psychiatric Association, New York, May 1–6, 2004. Received Sept. 15, 2004; revision received Dec. 9, 2004; accepted Dec. 28, 2004. From the Division of Epidemiology, Services, and Prevention Research, National Institute on Drug Abuse, NIH; and the Office of Applied Statistics, Substance Abuse, and Mental Health Services Administration, Department of Health and Human Services, Bethesda, Md. Address correspondence and reprint requests to Dr. Compton, Division of Epidemiology, Services, and Prevention Research, National Institute on Drug Abuse, 6001 Executive Blvd., MSC 9589, Bethesda, MD 20892–9589; [email protected] (e-mail). The views and opinions expressed in this report are those of the authors and should not necessarily be construed to represent the views of any of the sponsoring agencies or the U.S. government.
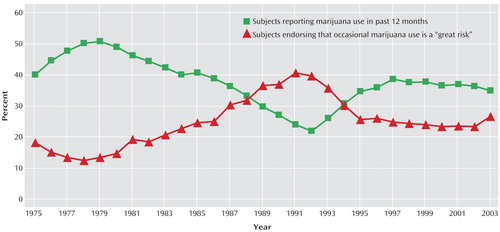
Figure 1. Past Year Marijuana Use by 12th-Graders Versus Perceived Risk of Occasional Marijuana Use in the Monitoring the Future Study, 1975–2003a
aData from Johnston et al. (4).
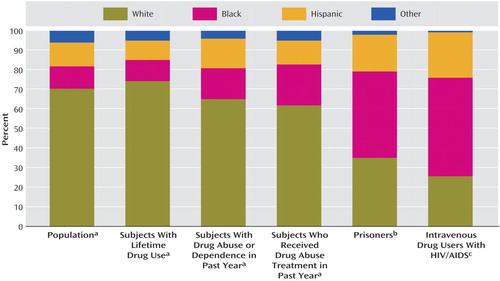
Figure 2. Distribution of Selected Variables Related to Drug Use by Race/Ethnicity
aData from 2002 National Survey on Drug Use and Health (5): Population by Race/Ethnicity in 2002, Percent of Persons 12+ Reporting Any Illicit Drug Use in Lifetime by Race/Ethnicity in 2002, Percent of Persons 12+ Meeting Criteria for Drug Abuse or Dependence in Past Year by Race/Ethnicity in 2002, and Percent of Persons 12+ Reporting They Received Drug Abuse Treatment in the Past Year by Race/Ethnicity in 2002.
bData from Bureau of Justice Statistics Bulletin (10).
cData from Centers for Disease Control and Prevention (11).
1. Susser E, Bresnahan M: Origins of epidemiology. Ann NY Acad Sci 2001; 954:6–18Crossref, Medline, Google Scholar
2. Fishbein D: The importance of neurobiological research to the prevention of psychopathology. Prev Sci 2000; 1:89–106Crossref, Medline, Google Scholar
3. Last JM (ed): A Dictionary of Epidemiology, 4th ed. New York, Oxford University Press, 2001Google Scholar
4. Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE: Monitoring the Future: National Survey Results on Drug Use, 1975–2003, vol I: Secondary School Students: NIH Publication 04–5507. Bethesda, Md, National Institute on Drug Abuse, 2004Google Scholar
5. Results From the 2002 National Survey on Drug Use and Health: National Findings: NHSDA Series H-22: DHHS Publication SMA 03–3836. Rockville, Md, Substance Abuse and Mental Health Services Administration, Office of Applied Studies, 2003Google Scholar
6. Gfroerer J, Wright D, Kopstein A: Prevalence of youth substance use: the impact of methodological differences between two national surveys. Drug Alcohol Depend 1997; 47:19–30Crossref, Medline, Google Scholar
7. Zacny J, Bigelow G, Compton P, Foley K, Iguchi M, Sannerud C: College on Problems of Drug Dependence Task Force on Prescription Opioid Non-Medical Use and Abuse position statement. Drug Alcohol Depend 2003; 69:215–232Crossref, Medline, Google Scholar
8. Compton WM, Grant BF, Colliver JD, Glantz MD, Stinson FS: Prevalence of marijuana use disorders in the United States: 1991–1992 and 2001–2002. JAMA 2004; 291:2114–2121Crossref, Medline, Google Scholar
9. Epidemiological Trends in Drug Abuse: NIH Publication 04–5364A. Washington, DC, National Institute on Drug Abuse, Community Epidemiology Work Group, 2004Google Scholar
10. Harrison PM, Beck AJ: Prisoners in 2003. Bureau of Justice Statistics Bulletin, Nov 2004, US Department of Justice, Office of Justice Programs. http://www.ojp.usdoj.gov/bjs/pub/pdf/p03.pdfGoogle Scholar
11. Percent of Persons Living with AIDS Contracted Through Intravenous Drug Use, by Race/Ethnicity at End of 2002: HIV/AIDS Surveillance Report. Atlanta, Centers for Disease Control and Prevention, 2002Google Scholar
12. Eliminating Racial and Ethnic Health Disparities. Atlanta, Centers for Disease Control and Prevention, 2004. http://www.cdc. gov/omh/AboutUs/disparities.htmGoogle Scholar
13. Strategic Plan for Reducing Health Disparities. Washington, DC, National Institute on Drug Abuse, 2004. http://www.drugabuse. gov/StrategicPlan/HealthStratPlan.htmlGoogle Scholar
14. Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton WM, Pickering RP, Kaplan K: Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry 2004; 61:807–816Crossref, Medline, Google Scholar
15. Regier DA, Farmer ME, Rae DS, Locke BZ, Keith SJ, Judd LL: Comorbidity of mental disorders with alcohol and other drug abuse: results from the Epidemiologic Catchment Area (ECA) study. JAMA 1990; 262:2511–2518Crossref, Google Scholar
16. Warner LA, Kessler RC, Hughes M, Anthony JC, Nelson CB: Prevalence and correlates of drug use and dependence in the United States: results from the National Comorbidity Survey. Arch Gen Psychiatry 1995; 52:219–229Crossref, Medline, Google Scholar
17. Grant BF: Comorbidity between DSM-IV drug use disorders and major depression: results of a national survey of adults. J Subst Abuse 1995; 7:481–497Crossref, Medline, Google Scholar
18. Kessler RC, Aguilar-Gaxiola S, Andrade L, Bijl R, Borges G, Caraveo-Anduaga JJ, DeWit DJ, Kolody B, Merikangas KR, Molnar BE, Vega WA, Walters EE, Wittchen H-U, Ustun TB: Mental-substance comorbidities in the ICPE surveys. Psychiatr Fenn 2001; 32:62–79Google Scholar
19. Grant BF, Stinson FS, Dawson DA, Chou SP, Ruan WJ, Pickering RP: Co-occurrence of 12-month alcohol and drug use disorders and personality disorders in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry 2004; 61:361–368Crossref, Medline, Google Scholar
20. Merikangas KR, Mehta RL, Molnar BE, Walters EE, Swendsen JD, Aguilar-Gaxiola S, Bijl RV, Borges G, Caraveo-Anduaga JJ, DeWit DJ, Kolody B, Vega WA, Wittchen HU, Kessler RC: Comorbidity of substance use disorders with mood and anxiety disorders: results of the International Consortium in Psychiatric Epidemiology. Addict Behav 1998; 23:893–907Crossref, Medline, Google Scholar
21. Swendsen JD, Merikangas KR: The comorbidity of depression and substance use disorders. Clin Psychol Rev 2000; 20:173–189Crossref, Medline, Google Scholar
22. Kessler RC, Nelson CB, McGonagle KA, Edlund MJ, Frank RG, Leaf PJ: The epidemiology of co-occurring addictive and mental disorders: implications for prevention and service utilization. Am J Orthopsychiatry 1996; 66:17–31Crossref, Medline, Google Scholar
23. Compton W, Conway KP, Stinson FS, Colliver JD, Grant BF: Prevalence and comorbidity of DSM-IV antisocial personality syndromes and specific substance use disorders in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry (in press)Google Scholar
24. Robins LN, McEvoy LT: Conduct problems as predictors of substance abuse, in Straight and Deviant Pathways From Childhood to Adulthood. Edited by Robins LN, Rutter M. New York, Cambridge University Press, 1990, pp 182–204Google Scholar
25. Lewinsohn PM, Brown RA, Seeley JR, Ramsey SE: Psychosocial correlates of cigarette smoking abstinence, experimentation, persistence and frequency during adolescence. Nicotine Tob Res 2000; 2:121–131Crossref, Medline, Google Scholar
26. Breslau N, Novak SP, Kessler RC: Daily smoking and the subsequent onset of psychiatric disorders. Psychol Med 2004; 34:323–333Crossref, Medline, Google Scholar
27. White HR, Xie M, Thompson W, Loeber R, Stouthamer-Loeber M: Psychopathology as a predictor of adolescent drug use trajectories. Psychol Addict Behav 2001; 15:210–218Crossref, Medline, Google Scholar
28. Kandel DB, Yamaguchi K: From beer to crack: Developmental patterns of drug involvement. Am J Public Health 1993; 83:851–855Crossref, Medline, Google Scholar
29. Lynskey MT, Health AC, Bucholz KK, Slutskey WS, Madden PA, Nelson EC, Stratham DJ, Martin NG: Escalation of drug use in early onset cannabis users vs co-twin controls. JAMA 2003; 289:427–433Crossref, Medline, Google Scholar
30. Morral AR, McCaffrey DF, Paddock SM: Reassessing the marijuana gateway effect. Addiction 2002; 97:1493–1504Crossref, Medline, Google Scholar
31. Agrawal A, Neale MC, Prescott CA, Kendler KS: Cannabis and other illicit drugs: comorbid use and abuse/dependence in males and females. Behav Genet 2004; 34:217–228; correction, 34:557Crossref, Medline, Google Scholar
32. Kellam SG, Anthony JC: Targeting early antecedents to prevent tobacco smoking: findings from an epidemiologically based randomized field trial. Am J Public Health 1998; 88:193–197Crossref, Medline, Google Scholar
33. Hawkins JD, Catalano RF, Kosterman R, Abbott R, Hill KG: Preventing adolescent health-risk behaviors by strengthening protection during childhood. Arch Pediatr Adolesc Med 1999; 153:226–234Crossref, Medline, Google Scholar
34. Ellickson PL, Martino SC, Collins RL: Marijuana use from adolescence to young adulthood: multiple developmental trajectories and their associated outcomes. Health Psychol 2004; 23:299–307Crossref, Medline, Google Scholar
35. Merikangas KR, Stolar M, Stevens DE, Goulet J, Priesig M, Fenton B, Rounsaville BJ: Familial transmission of substance use disorders. Arch Gen Psychiatry 1998; 55:973–979Crossref, Medline, Google Scholar
36. Bierut LJ, Dinwiddie SH, Begleiter H, Crowe RR, Hesselbrock V, Nurnberger JI Jr, Porjesz B, Schuckit MA, Reich T: Familial transmission of substance dependence: alcohol, marijuana, cocaine, and habitual smoking: a report from the Collaborative Study on the Genetics of Alcoholism. Arch Gen Psychiatry 1998; 55:982–988Crossref, Medline, Google Scholar
37. Langbehn DR, Cadoret RJ, Caspers K, Troughton EP, Yucuis R: Genetic and environmental risk factors for the onset of drug use and problems in adoptees. Drug Alcohol Depend 2003; 69:151–167Crossref, Medline, Google Scholar
38. Kendler KS, Prescott CA, Myers J, Neale MC: The structure of genetic and environmental risk factors for common psychiatric and substance use disorders in men and women. Arch Gen Psychiatry 2003; 60:929–937Crossref, Medline, Google Scholar
39. Chassin L, Pitts SC, Prost J: Binge drinking trajectories from adolescence to emerging adulthood in a high-risk sample: predictors and substance abuse outcomes. J Consult Clin Psychol 2002; 70:67–78Crossref, Medline, Google Scholar
40. Moss HB, Lynch KG, Hardie TL, Baron DA: Family functioning and peer affiliation in children of fathers with antisocial personality disorder and substance dependence: associations with problem behaviors. Am J Psychiatry 2002; 159:607–614Link, Google Scholar
41. Tarter RE, Kirisci L, Mezzich A, Cornelius JR, Pajer K, Vanyukov M, Gardner W, Blackson T, Clark D: Neurobehavioral disinhibition in childhood predicts early age at onset of substance use disorder. Am J Psychiatry 2003; 160:1078–1085Link, Google Scholar
42. Compton WM, Cottler LB, Ridenour TA, Ben-Abdallah A, Spitznagel EL: The specificity of family history of alcohol and drug abuse in cocaine abusers. Am J Addict 2002; 11:85–94Crossref, Medline, Google Scholar
43. Tsuang MT, Bar JL, Harley RM, Lyons MJ: The Harvard Twin Study of Substance Abuse: what we have learned. Harv Rev Psychiatry 2001; 9:267–279Crossref, Medline, Google Scholar
44. Kendler KS, Jacobson KC, Prescott CA, Neale MC: Specificity of genetic and environmental risk factors for use and abuse/dependence of cannabis, cocaine, hallucinogens, sedatives, stimulants, and opiates in male twins. Am J Psychiatry 2003; 160:687–695Link, Google Scholar
45. Tsuang MT, Tohen M (eds): Textbook in Psychiatric Epidemiology, 2nd ed. New York, Wiley-Liss, 2002Google Scholar
46. Caspi A, McClay J, Moffitt TE, Mill J, Martin J, Craig IW, Taylor A, Poulton R: Role of genotype in the cycle of violence in maltreated children. Science 2002; 297:851–854Crossref, Medline, Google Scholar
47. Foley DL, Eaves LJ, Wormley B, Silberg JL, Maes HH, Kuhn J, Riley B: Childhood adversity, monoamine oxidase a genotype, and risk for conduct disorder. Arch Gen Psychiatry 2004; 61:738–744Crossref, Medline, Google Scholar
48. Hawkins JD, Catalano RF, Miller JY: Risk and protective factors for alcohol and other drug problems in adolescence and early adulthood: implications for substance abuse prevention. Psychol Bull 1992; 112:64–105Crossref, Medline, Google Scholar
49. Bry BH, McKeon P, Pandina RJ: Extent of drug use as a function of number of risk factors. J Abnorm Psychol 1982; 91:273–279Crossref, Medline, Google Scholar
50. Newcomb MD, Maddahian E, Skager R, Bentler PM: Substance abuse and psychosocial risk factors among teenagers: associations with sex, age, ethnicity, and type of school. Am J Drug Alcohol Abuse 1987; 14:413–433Crossref, Google Scholar
51. Glantz MD, Weinberg NZ, Miner LL, Colliver JD: The etiology of drug abuse: mapping the paths, in Drug Abuse: Origins and Interventions. Edited by Glantz MD, Hartel CR. Washington, DC, American Psychological Association, 1999, pp 3–46Google Scholar
52. Galea S, Nandi A, Vlahov D: The social epidemiology of substance use. Epidemiol Rev 2004; 26:36–52Crossref, Medline, Google Scholar
53. Jenks C, Meyer S: The social consequences of growing up in a poor neighborhood, in Inner-City Poverty in the United States. Edited by Lynn LJ, McGeary MGH. Washington, DC, National Academy Press, 1990, pp 111–186Google Scholar
54. Burton LM, Jarett RL: In the mix, yet on the margins: the place of families in urban neighborhoods and child development research. J Marriage and the Family 2000; 62:1114–1135Crossref, Google Scholar
55. Sampson RJ, Morenoff JD, Gannon-Rowley T: Assessing “neighborhood effects”: social processes and new directions in research. Annu Rev Sociol 2002; 28:443–478Crossref, Google Scholar
56. Sampson RJ, Raudenbush SW, Earls F: Neighborhoods and violent crime: a multilevel study of collective efficacy. Science 1997; 27:918–924Crossref, Google Scholar
57. Petronis KR, Anthony JC: Perceived risk of cocaine use and experience with cocaine: do they cluster within US neighborhoods and cities? Drug Alcohol Depend 2000; 57:183–192Crossref, Medline, Google Scholar
58. Yen IH, Syme SL: The social environment and health: a discussion of the epidemiologic literature. Annu Rev Public Health 1999; 20:287–308Crossref, Medline, Google Scholar
59. Kaplan GA: What’s wrong with social epidemiology, and how can we make it better? Epidemiol Rev 2004; 26:124–135Crossref, Medline, Google Scholar
60. Peltonen L, McKusick VA: Genomics and medicine: dissecting human disease in the postgenomic era. Science 2003; 291:1224–1229Crossref, Google Scholar
61. Merikangas KR: Genetic epidemiology of substance-use disorders, in Textbook of Biological Psychiatry. Edited by D’haenen, Den Boer J, Willner P. New York, John Wiley & Sons, 2002, pp 537–546Google Scholar
62. Dahl RE, Spear LP (eds): Adolescent Brain Development: Vulnerabilities and Opportunities: Annals of the New York Academy of Science, vol 1021. New York, New York Academy of Sciences, 2004Google Scholar
63. Young EA, Breslau N: Cortisol and catecholamines in posttraumatic stress disorder: an epidemiologic community study. Arch Gen Psychiatry 2004; 61:394–401Crossref, Medline, Google Scholar
64. Cozier YC, Palmer JR, Rosenberg L: Comparison of methods for collection of DNA samples by mail in the black women’s health study. Ann Epidemiol 2004; 4:117–122Crossref, Google Scholar
65. Stone A, Shiffman S: Ecological momentary assessment (EMA) in behavioral medicine. Ann Behav Med 1994; 16:199–202Crossref, Google Scholar
66. Muthén BO: Second-generation structural equation modeling with a combination of categorical and continuous latent variables: new opportunities for latent class-latent growth modeling, in New Methods for the Analysis of Change. Edited by Collins LM, Sayer AG. Washington, DC, American Psychological Association, 2001, pp 291–322Google Scholar
67. Gfroerer J, Penne M, Pemberton M, Folsom R: Substance abuse treatment need among older adults in 2020: the impact of the aging baby-boom cohort. Drug Alcohol Depend 2003; 69:127–135Crossref, Medline, Google Scholar
68. Muthén BO: Latent variable mixture modeling, in New Developments and Techniques in Structural Equation Modeling. Edited by Marcoulides GA, Schumacker RE. Mahwah, NJ, Lawrence Erlbaum Associates, 2001, pp 1–33Google Scholar
69. Lynch JW, Kaplan GA, Salonen JT: Why do poor people behave poorly? variation in adult health behaviors and psychological characteristics by stages of the socioeconomic life course. Soc Sci Med 1997; 44:809–819Crossref, Medline, Google Scholar
70. Grunbaum JA, Kann L, Kinchen SA, Williams B, Ross JG, Lowry R, Kolbe L: Youth risk behavior surveillance—United States 2001. MMWR Surveill Summ 2002; 51:1–62Medline, Google Scholar
71. Substance Abuse and Mental Health Services Administration (SAMHSA): Notice of Funding Availability, Initial Funding Opportunity Number TI 05–006 State Adolescent Substance Abuse Treatment Coordination. http://www.samhsa.gov/grants/2005/nofa/ti05006_adolescents.aspxGoogle Scholar
72. Curtis N, Ronan K, Borduin C: Multisystemic treatment: a meta-analysis of outcome studies. J Fam Psychol 2004; 18:411–419Crossref, Medline, Google Scholar
73. Sexton T, Alexander J: Family-based empirically supported interventions. Couns Psychol 2002; 30:238–261Crossref, Google Scholar



