Strong Inverse Association Between Height and Suicide in a Large Cohort of Swedish Men: Evidence of Early Life Origins of Suicidal Behavior?
Abstract
OBJECTIVE: Previous studies have found associations between poor fetal and infant growth and the risk of suicide. The authors’ goal was to investigate the association between height—a measure of childhood growth—and suicide risk. METHOD: The authors conducted a record linkage study of the birth, conscription, mortality, family, and census register data of 1,299,177 Swedish men followed from age 18 to a maximum of age 49. RESULTS: There were 3,075 suicides over an average follow-up period of 15 years. There was a strong inverse association between height and suicide risk. In fully adjusted models, a 5-cm increase in height was associated with a 9% decrease in suicide risk. CONCLUSIONS: The strong inverse association between height and suicide may signify the importance of childhood exposure in the etiology of adult mental disorder or reflect stigmatization or discrimination encountered by short men in their adult lives.
Height is a marker of postnatal development as well as factors, including genes, that influence growth. Associations of several adult chronic diseases with height are thought to indicate the importance of the postnatal environment on disease risk (1). Few previous prospective studies have investigated the association of height with suicide. A Swedish study (2) found some evidence of a greater risk among the shortest 10% of men studied, but possible socioeconomic confounding factors were not taken into account. The other study, from South Korea (3), documented a twofold greater risk of suicide in the shortest compared with the tallest men, but this association was attenuated after the authors controlled for socioeconomic factors. A further investigation reported inverse associations between height and hospital admission for self-harm (4). In the current article, we examine the relationship between height and suicide in a large cohort of Swedish men.
Method
Swedish-born males born 1950–1981 for whom information on their biological parents was available (N=1,654,668) were identified in the Swedish Multi-Generation Register; 1,442,923 (87.2%) of these individuals had a record in the Military Service Conscription Register 1968–1999. These records were linked with the Medical Birth Register, the Cause of Death Register 1968–1999, and the Population and Housing Censuses 1970–2000.
Height measurements at age 18–19 years were obtained from the Military Service Conscription Register. The following possible confounding factors were assessed: maternal and paternal educational level (six categories); the highest socioeconomic index of either parent (four categories); body mass index; date of birth; and conscription center (six centers). Information on marital status at age 30–35 years was available for a subgroup born before 1960. For men born after 1973, information on birth weight, birth length, and gestational age were obtained from the Medical Birth Register.
Altogether, complete information was available on all variables described above for 1,299,177 (90%) of the subjects. Individuals excluded due to incomplete information were shorter (mean height=178.6 cm) than those included (mean height=179.3 cm) (t=37.05, df=1,442,921, p<0.0001) and had a higher suicide rate (age- and birth-year-adjusted hazard ratio=1.15, p<0.01).
Suicide deaths occurring between age 18 and 49 years were identified by using ICD-8 and ICD-9 codes E950–E959 or ICD-10 codes X60–X84. Associations were also investigated with 1) undetermined deaths (ICD-8 and ICD-9 codes E980–E989 or ICD-10 codes Y10–Y34) and 2) alcohol-related deaths (ICD-8 and ICD-9 codes 291, 303, 571, and E860 or ICD-10 codes F10, K70, T51, X45, X65).
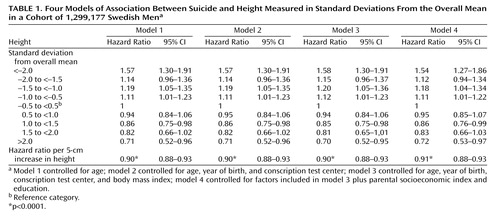
We used Cox’s proportional hazards models, with age as the time axis, to investigate associations between height and suicide. Subjects were censored at their date of death, emigration, or the end of follow-up (Dec. 31, 1999). We categorized subjects into nine groups on the basis of the number of standard deviations their height was from the overall mean (<2.0, –2 to <–1.5, –1.5 to <–1.0, –1.0 to <–0.5, –0.5 to <0.5, 0.5 to <1.0, 1.0 to <1.5, 1.5 to 2.0 and >2.0 standard deviations). We also estimated hazard ratios for 5-cm increments in height.
Results
The mean height of the 1,299,177 conscripts was 1.79 m; 711,949 (54.8%) came from white-collar families; and 3,075 (0.24%) died by suicide. Taller men had a much lower risk of suicide than shorter men (Table 1). The association was linear. A 5-cm increase in height was associated with a 9% (95% confidence interval [CI]=7%–12%) decrease in suicide risk. The effect of height changed little after adjustment for parental socioeconomic index or the participant’s body mass index.
To assess whether secular increases in height may account for the observed associations, we repeated the analysis using year of birth as the time axis. The associations were unchanged: the hazard ratio per 5-cm change in height was 0.90 (95% CI=0.88–0.93) (Table 1).
Compared with height-suicide associations, height was more strongly related to undetermined deaths (hazard ratio per 5-cm increase in height=0.86, 95% CI=0.81–0.90), and alcohol-related deaths (hazard ratio=0.77, 95% CI=0.71–0.83).
In the subgroup born 1950–1965 and alive in 1990, who had had the opportunity to complete their education, the height-suicide association was only weakly attenuated—from 0.91 (95% CI=0.86–0.95) to 0.92 (95% CI=0.88–0.97)—after we controlled for education. Information on marital status at age 30–35 years was available for men born before 1960, and the fully adjusted hazard ratio in this subgroup—0.93 (95% CI=0.88–0.98)—was only weakly attenuated after adjustment for marital status—0.94 (95% CI=0.89–0.99). In the subgroup of men with birth weight data, the hazard ratio for suicide was unchanged after we controlled for birth weight, gestational age, and birth length (data not shown).
Exclusion of all conscripts with a psychiatric diagnosis at conscription (ICD-8 and ICD-9 codes 290–319) from the fully adjusted analysis did not affect the hazard ratio markedly—0.91 (95% CI=0.89–0.94). The height-suicide association was 0.94 (95% CI=0.87–1.00) among those excluded for this reason.
Discussion
We found a twofold higher risk of suicide in short men than tall men. The associations do not appear to be attributable to socioeconomic confounding or prenatal influences on growth (5). Stronger associations were seen with alcohol-related mortality, suggesting that substance misuse may contribute to the observed patterns.
A strength of our study is that it includes 79% of all men born in Sweden in 1950–1981. It has two main limitations. We were unable to fully assess the possible influence of unemployment, relationship breakdown, or mental illness on the height-suicide associations. Our findings cannot be generalized to women or older men. Nevertheless, in Sweden, the United States, and the United Kingdom, suicides in 18–49-year-old men account for almost half of all suicides.
There are several explanations for our findings. First, psychological stress and disrupted family life in childhood impair growth (6) and may increase susceptibility to mental illness and suicidal behavior in later life (7). Short stature may be associated with a greater risk of psychosis (8), which in turn influences suicide risk. However, associations were not attenuated by excluding subjects with psychiatric diagnoses at conscription. Short individuals are more likely to be in a low social class as adults, independent of their childhood social class (9). Low social class is associated with a greater risk of suicide (10). In a subset of subjects, however, we found that educational level, a marker of socioeconomic position, had little effect on the associations. Marriage protects against suicide (11), and short individuals may be less likely to marry than taller ones (12). Marital status only weakly confounded the associations. Low weight gain in infancy may also be a risk factor for suicide in adult life (13). Finally, short children tend to have lower levels of intelligence and may suffer stigmatization and discrimination (9, 14).
 |
Received Feb. 6, 2004; revisions received April 23 and July 15, 2004; accepted Aug. 11, 2004. From the Department of Genetics and Pathology, Rudbeck Laboratory, Uppsala University, Sweden; the Department of Social Medicine, University of Bristol, U.K.; and the Child and Adolescent Public Health Epidemiology Group, Department of Public Health Sciences, Karolinska Institute. Address correspondence and reprint requests to Associate Professor Rasmussen, Department of Public Health Sciences, Karolinska Institute, Norrbacka, SE-171 76, Stockholm, Sweden; [email protected] (e-mail).
1. Gunnell D: Commentary: can adult anthropometry be used as a “biomarker” for prenatal and childhood exposures? Int J Epidemiol 2002; 31:390–394Crossref, Medline, Google Scholar
2. Allebeck P, Bergh C: Height, body mass index and mortality: do social factors explain the association? Public Health 1992; 106:375–382Crossref, Medline, Google Scholar
3. Song YM, Smith GD, Sung J: Adult height and cause-specific mortality: a large prospective study of South Korean men. Am J Epidemiol 2003; 158:479–485Crossref, Medline, Google Scholar
4. Jiang GX, Rasmussen F, Wasserman D: Short stature and poor psychological performance: risk factors for attempted suicide among Swedish male conscripts. Acta Psychiatr Scand 1999; 100:433–440Crossref, Medline, Google Scholar
5. Thompson C, Syddall H, Rodin I, Osmond C, Barker DJ: Birth weight and the risk of depressive disorder in late life. Br J Psychiatry 2001; 179:450–455Crossref, Medline, Google Scholar
6. Wales JKH, Taitz LS: Patterns of growth in abused children, in Human Growth: Basic and Clinical Aspects. Edited by Hernández M. Amsterdam, Excerpta Medica, 1992, pp 151–159Google Scholar
7. Fergusson DM, Woodward LJ, Horwood LJ: Risk factors and life processes associated with the onset of suicidal behaviour during adolescence and early adulthood. Psychol Med 2000; 30:23–39Crossref, Medline, Google Scholar
8. Gunnell D, Rasmussen F, Fouskakis D, Tynelius P, Harrison G: Patterns of fetal and childhood growth and the development of psychosis in young males: a cohort study. Am J Epidemiol 2003; 158:291–300Crossref, Medline, Google Scholar
9. Nyström P: Childhood environment, intergenerational mobility, and adult health: evidence from Swedish data. J Epidemiol Community Health 1992; 46:71–74Crossref, Medline, Google Scholar
10. Drever F, Whitehead M: Health Inequalities. London, Her Majesty’s Stationery Office, 1997Google Scholar
11. Kreitman N: Suicide, age and marital status. Psychol Med 1988; 18:121–128Crossref, Medline, Google Scholar
12. Murray JE: Marital protection and marital selection: evidence from a historical-prospective sample of American men. Demography 2000; 37:511–521Crossref, Medline, Google Scholar
13. Barker DJP, Osmond C, Rodin I, Fall CHD, Winter PD: Low weight gain in infancy and suicide in adult life. BMJ 1995; 311:1203Crossref, Medline, Google Scholar
14. Downie AB, Mulligan J, Stratford RJ, Betts PR, Voss LD: Are short normal children at a disadvantage? the Wessex growth study. BMJ 1997; 314:97–100Crossref, Medline, Google Scholar



