National Trends in Hospitalization of Youth With Intentional Self-Inflicted Injuries
Abstract
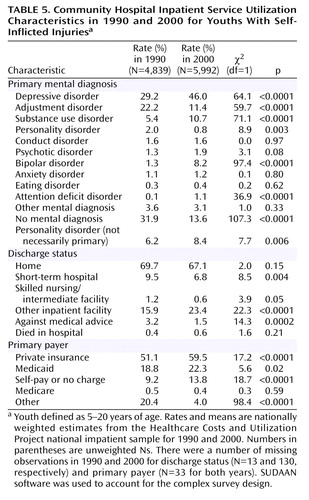
OBJECTIVE: The authors examined national trends from 1990 to 2000 in the utilization of community hospital inpatient services by young people (5–20 years of age) with intentional self-inflicted injuries. METHOD: Discharge abstracts from a nationally representative sample of community hospitals were analyzed, with a focus on youth discharges (N=10,831) with a diagnosis of intentional self-inflicted injury (ICD-9-CM: E950–E959). Census data were used to derive national population-based rates of self-inflicted injuries requiring inpatient treatment. Overall population-based trends in hospitalizations for self-inflicted injury were calculated and stratified by gender and age. Among youths hospitalized with a self-inflicted injury, trends were also calculated for length of stay, inpatient costs, method of injury, and associated mental disorder diagnoses. RESULTS: The annual hospitalization rate of youths with self-inflicted injuries declined from 49.1 per 100,000 in 1990 to 44.9 per 100,000 in 2000, and the mean length of inpatient stay significantly declined from 3.6 days to 2.7 days. Among the hospitalized patients, there were increases in the rate of cutting (4.3% to 13.2%) and ingestion of acetaminophen (22.1% to 26.9%), antidepressants (10.0% to 14.0%), and opiates (2.3% to 3.3%) as a cause of injury, whereas there were decreases in the ingestion of salicylates (14.9% to 10.2%) and barbiturates (1.5% to 0.7%). There were significant increases in the proportion of subjects with primary mental disorder discharge diagnoses of depressive disorder (29.2% to 46.0%), bipolar disorder (1.3% to 8.2%), and substance use disorder (5.4% to 10.7%) and significant decreases in the rate of adjustment disorders (22.2% to 11.4%) and nonmental disorders (31.9% to 13.6%). After excluding cutting, which may be more closely related to self-mutilation than suicidal self-injury, the annual hospitalization rate of youths with self-inflicted injuries declined from 47.2 per 100,000 in 1990 to 39.4 per 100,000 in 2000. CONCLUSIONS: Over the decade of study, young people admitted to community hospitals with self-inflicted injuries tended to have more severe psychiatric diagnoses and to be treated during shorter inpatient stays. These trends suggest that the role of youth inpatient care has narrowed, becoming focused on those with severe psychiatric disorders.
Considerable controversy surrounds the proper role of short-term inpatient psychiatric treatment for the acute care of young people following an intentional self-injury (1). Whereas some clinical researchers have questioned the necessity and usefulness of admitting acutely self-injurious youth for inpatient psychiatric treatment for other than medical reasons (2), others have developed specific psychiatric indications for admitting suicidal youth to the hospital (3). In practice, emergency room clinicians must grapple with determining whether acutely self-injurious children and adolescents can be safely managed from a medical and psychiatric perspective in treatment settings that are less restrictive and disruptive than hospital care. A wide range of clinical considerations—including medical severity of the attempt, child risk factors, availability of family support and community resources, cost and reimbursement issues, and concerns over adherence with follow-up treatment plans—influence the clinical decision of whether to admit a young person for inpatient care following a self-inflicted injury (4, 5).
Over the last several years, a variety of cost-containment mechanisms have been developed to encourage the substitution of less costly outpatient care for more expensive inpatient services. Between 1987 and 1997, the proportion of total national mental health service expenditures devoted to inpatient psychiatric treatment declined from 40.5% in 1987 to 29.6% in 1997 (6). During this period, many managed care plans developed specific privately held criteria for approving inpatient treatment of suicidal patients (7). For patients admitted to the hospital, managed care utilization management techniques also sought to reduce the length and costs of inpatient care (8, 9). At the same time, the number of families covered by managed behavioral health plans increased (8).
In the current study, we examine national trends from 1990 to 2000 in community hospital admissions of young people 5–20 years of age with intentional self-inflicted injuries. Using nationally representative data, we describe changes in the rates at which young people were admitted to community hospitals with such injuries and characterize changes in the method of injury, clinical diagnoses received, length of inpatient stay, discharge status, inpatient costs, and primary payer. As a result of changes in the managed care environment, we anticipated that there would be a decline in the rate of youths hospitalized with self-inflicted injuries, a decrease in their length of stay, and an increase in the proportion diagnosed with high-risk conditions, such as mood and substance use disorders, strongly associated with youth suicide.
Method
Data were drawn from the 1990 and 2000 nationwide inpatient samples of the Healthcare Costs and Utilization Project (10). The project is sponsored by the Agency for Healthcare Research and Quality and includes over 100 clinical and nonclinical variables. The Healthcare Costs and Utilization Project consisted of 6,268,515 computerized discharge reports from a geographically diverse sample of 882 community hospitals in 1990 and 7,450,992 discharge reports from a diverse sample of 994 hospitals in 2000. Community hospitals include nonfederal short-term general hospitals and academic medical centers but not specialized psychiatric hospitals. Each year the Healthcare Costs and Utilization Project approximates a 20% stratified sample of U.S. community hospitals. Selection into the sample is based on a stratified probability selection of short-stay nonfederal general hospitals. Weights were constructed on the basis of the reciprocal probability of sampling to approximate national estimates. All percentages in this report are weighted to adjust for the sampling probability.
We limited the analysis to data from youths 5–20 years of age who were admitted to the hospital on an urgent or emergent basis and had a discharge diagnosis for intentional self-inflicted injury (ICD-9-CM: E950.0–E959.9). To estimate population rates of hospitalization for self-inflicted injury, population data were culled from the 1990 and 2000 United States Bureau of the Census (11).
Our first goal was to describe the method of injury, primary mental disorder diagnosis, length of stay, and discharge status of youth by gender and age group in 2000. We then described trends in the hospitalization rate of youths with intentional self-injury between 1990 and 2000. We determined rates of intentional self-injury per 100,000 population, both overall and stratified by age and gender. Substantial missing race/ethnicity data and changes in the federal classification of race/ethnicity categories during the study period prevented a meaningful analysis of these variables.
We then examined trends in the distribution of self-injury method. Injuries were first classified by major category: drug ingestion (E950), hanging/suffocating (E953), firearm (E955), gas asphyxiation (E951, E952), cutting (E956), and a residual group of other types of injury (E954, E957, E958, E959). Psychotropic drug ingestion was subsequently subclassified on the basis of discharge diagnosis codes: anxiolytics/sedatives (barbiturates, benzodiazepines, and others), antidepressants, antipsychotics, opiates, and other/unspecified psychotropic drugs. Nonpsychotropic ingestion was subclassified as analgesics (acetaminophen, salicylates, and other/unspecified) and other nonpsychotropic substances.
We then examined trends for mean length of stay, discharge status, primary payer, and primary mental disorder diagnoses among youth admissions with intentional self-injuries. Primary mental disorder was defined as the first-listed diagnosis that was a mental disorder (ICD-9-CM: 219–320). Mental disorders were classified into depressive disorders (ICD-9-CM: 296.2, 296.3, 298.0, 300.4, 311), adjustment disorders (309), substance use disorders (291, 292, 303, 304, 305), personality disorders (301), conduct disorder (312, 313.81), psychotic disorders (295, 297–299), bipolar disorder (296.0, 296.1, 296.4–296.9), anxiety disorders (300.0, 300.2, 300.3, 308.3, 309.21, 309.81, 313.0), eating disorders (307.1, 307.5), attention deficit hyperactivity disorder (314), and other mental disorders. A separate category was constructed for discharges with no mental disorder diagnosis.
Because cutting or self-mutilation is rarely associated with completed suicide in young people (12) and tends to be less lethal than other forms of self-injury (13), we also examined overall trends in hospitalization of youths with intentional self-injury excluding cutting (E956). Finally, total inpatient expenditures were calculated for all youths admitted with self-inflicted injuries in 1990 and 2000 and for all admissions excluding self-injury by cutting. The Consumer Price Index for medical care was used to inflate 1990 to 2000 dollars (14).
We used the SUDAAN statistical software package (15) to accommodate the complex sampling design and weights from the Healthcare Costs and Utilization Project when calculating means and corresponding standard errors and to calculate 95% confidence intervals (CIs) for the rate estimates.
Results
Gender and Age Distribution of Admissions in 2000
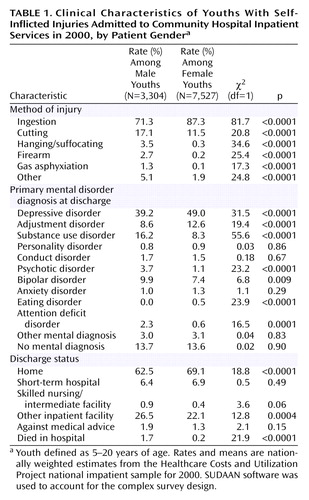
In 2000, several gender differences were evident in the method of injury, primary mental disorder diagnosis, and discharge status of youths admitted with self-inflicted injuries (Table 1). Relative to male subjects, female subjects were significantly more likely to be admitted because of harmful ingesting but less likely to be admitted following self-inflicted injuries due to cutting, hanging/suffocating, firearms, or gas asphyxiation. Female subjects were also significantly more likely to be discharged with a primary mental disorder diagnosis of depressive disorder, adjustment disorder, or an eating disorder but were less likely to be discharged with a diagnosis of substance use disorder, psychotic disorder, or attention deficit disorder. In addition, female subjects were significantly more likely than male subjects to be discharged to home and less likely to die in the hospital or be discharged to an inpatient facility other than a short-term hospital or skilled nursing or intermediate care facility. There was no difference in the number of inpatient days in the community hospital between male (mean=2.9, SE=0.1) and female (mean=2.6, SE=0.1) patients.
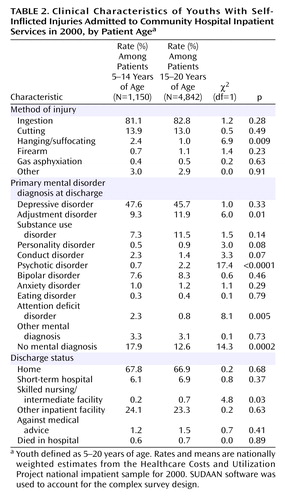
The pattern of youth admissions for self-inflicted injuries in 2000 also varied by patient age (Table 2). As compared with younger children (5–14 years of age), the older youth were significantly less likely to be admitted following a self-inflicted hanging/suffocating injury. The older youth were more likely than their younger counterparts to be discharged with a primary mental disorder diagnosis of adjustment disorder or a psychotic disorder but less likely to be discharged with an attention deficit disorder diagnosis or no mental disorder diagnosis. Older youth also tended to have a shorter length of inpatient stay (mean=2.7 days, SD=0.1) than younger youth (mean=3.0 days, SD=0.2) (t=2.3, df=5990, p=0.02).
National 10-Year Hospitalization Trends for Self-Injuring Youth
Rate of hospitalization
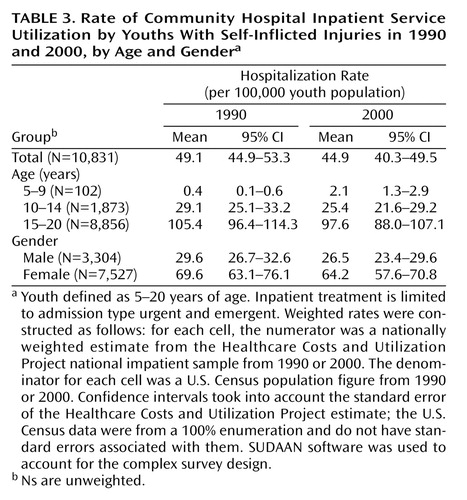
The overall rate of community hospital inpatient admissions due to self-injury among youths did not significantly change between 1990 (49 per 100,000 youth population) and 2000 (45 per 100,000 youth population) (Table 3). However, the rate of admissions significantly increased for children 5–9 years of age from 0.4 to 2.1 per 100,000 children (z=−3.96, p<0.0001). After excluding admissions for cutting, the overall rate of inpatient care for youth with intentional self-injuries significantly decreased from 47.2 per 100,000 youth population in 1990 to 39.4 per 100,000 youth population in 2000 (z=2.83, p=0.0047).
Method of injury
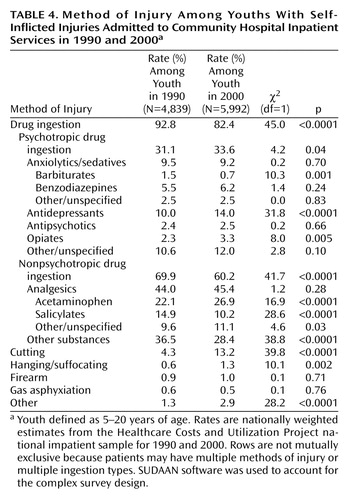
There was a significant decrease in the proportion of hospitalizations involving drug ingestion over the 10-year period. Significant decreases were specifically observed in the proportion of hospitalizations associated with barbiturates, salicylates, and unspecified nonpsychotropic drugs. During the same period, significant increases were evident in the proportion of hospitalizations associated with ingestions of antidepressant medications, opiates, and acetaminophen (Table 4). There was also a significant increase in the proportion of hospitalizations that involved cutting and hanging/suffocating.
Mental disorder diagnosis
In both study years, mental disorders were the primary discharge diagnosis for most youths hospitalized because of self-injury. Significant increases were specifically observed in the proportion of discharges with depressive disorder, substance use disorder, bipolar disorder, and attention deficit disorder (Table 5). There was also a significant increase in the proportion of discharges with a personality disorder listed as a secondary diagnosis.
Clinical service characteristics
In both 1990 and 2000, the majority of youths admitted because of intentional self-inflicted injuries were discharged to home (Table 5). Although transfer to short-term hospitals became significantly less common, transfers to other inpatient facilities became more common. Comparatively few young people died in the hospital or left the hospital against medical advice in either year. Also in both years, private insurance was the primary payer in a majority of the hospitalizations. Medicaid, which increased as a percentage of youth hospitalizations with intentional self-injury, was the second most common primary payer. The mean length of stay for the hospitalizations significantly declined from 3.6 days (SE=0.2) in 1990 to 2.7 days (SE=0.1) in 2000 (t=15.8, df=10,829, p=0.0001).
Inpatient expenditures
Total estimated inpatient costs in inflation-adjusted 2000 dollars for youth admissions with intentional self-injuries were $167.5 million in 1990 (95% CI=147.3–187.9) and $168.2 million (95% CI=147.2–187.8) in 2000. After excluding admissions for self-injury due to cutting, the respective estimates were $160.8 million (95% CI=141.4–180.2) in 1990 and $149.7 million (95% CI=130.3–169.1) in 2000 in inflation-adjusted 2000 dollars.
Discussion
Between 1990 and 2000, there was a statistically nonsignificant decrease in the annual rate of community hospital inpatient service utilization among youths admitted following intentional self-injury (from approximately 49 per 100,000 in 1990 to 45 per 100,000). This trend roughly parallels the national decline in suicides among youths 15–19 years of age, from 11.1 per 100,000 in 1990 to 8.2 per 100,000 in 2000 (12).
The trend in hospital admissions may portray important changes in the care of young people who intentionally injure themselves. During the period from 1991 to 2001, the Youth Risk Behavior Survey reported a substantial increase in the rate of injurious suicide attempts by students in grades 9 through 12, from 1.7% to 2.6% (16, 17). In the context of increasing base rates of self-injurious behavior, a slight decline in inpatient admissions of youths with intentional self-inflicted injuries suggests that the proportion of suicide attempts resulting in inpatient care has substantially declined.
In line with previous epidemiological (18) and clinical research (19), hospitalization as a result of self-inflicted injury was more common among female than male youths. Male youths were less likely than female youths to have a depressive disorder (20) or an eating disorder (21) but were more likely to have substance use disorder (22). Male youths were also proportionately more likely than female youths to use more highly lethal methods of self-injury (23) and to die in the hospital.
For young children ages 5 to 9 years, the rate of hospitalization with self-inflicted injuries, although still comparatively low, significantly increased during the study period. This trend should alert clinicians to the risks of suicidal behavior in young children. While the cause of this increase remains unknown, some evidence links child exposure to video games and movie violence to violent attitudes (24) and behavior (25). One small study has suggested that younger children who attempt suicide report many of the same depressive symptoms common to suicidal adolescents (26). The recent increase of inpatient admissions of young children with intentional self-inflicted injuries highlights the importance of prevention and early intervention programs that target preschool (27) or early grade school (28, 29) children at risk for mental health problems.
The changing diagnostic profile of young people admitted to the hospital following intentional self-injury could indicate a more focused approach for especially high-risk youth. Between 1990 and 2000, the proportion of discharges in which a mood disorder or substance use disorder was the first listed mental disorder significantly increased, whereas the proportion of adjustment disorder or no mental disorder discharges significantly declined. Psychological autopsy studies reveal that mood disorders occur in approximately two-thirds of youth suicides (30–32) and that substance use disorders occur in up to two-thirds of older boys who complete suicide (30, 32). By contrast, young people with adjustment disorders or no mental disorder are considerably less common among youth suicides (30, 32).
A trend toward more severe mental disorder diagnoses among inpatient youth discharges suggests the importance of developing rapid and efficient diagnostic procedures to identify young people with high-risk conditions (33). In one recent study, a school-based program for high school students that focused on depression and suicide risk was associated with a reduction in suicide attempts (34).
The trends in mental disorder diagnoses among youths hospitalized following self-inflicted injuries may reflect broad changes in diagnostic practices or clinical decision making in response to managed care restrictions on inpatient care for less severe mental disorders. To explore this possibility, we performed a set of post hoc Healthcare Costs and Utilization Project analyses. The trends observed among admissions with self-inflicted injuries were also apparent in the larger sample of youth admissions with a primary mental disorder diagnosis. For example, among youth admissions with primary mental disorder diagnoses, the proportion who were diagnosed with an adjustment disorder declined from 1990 (16.8%) to 2000 (6.5%), whereas increases were seen in depressive disorder (25.7% to 34.4%) and bipolar disorder (4.2% to 12.2%). Because similar trends were further observed among youth whose admissions were self-pay or not charged (adjustment disorder: 19.4% to 7.9%; depressive disorder: 18.4% to 31.1%; bipolar disorder: 2.0% to 9.6%), it is unlikely that the diagnostic trends are simply a coding response to restrictive utilization management policies.
During the decade under study, there was a particularly impressive increase in the proportion of hospitalizations in which bipolar disorder was the leading mental disorder diagnosis. Bipolar disorder in young people has been associated with an increased risk of suicide attempts (35) and completion (2, 36). In one case/control study of youth suicide, the odds ratio of suicide completion for bipolar disorder approached that for substance use disorders (36). However, manic or manic-like symptoms in young people may be difficult to distinguish from symptoms of ADHD (37, 38), and concern exists that there has been a trend toward overdiagnosis of youth bipolar disorder (39). From the available data, it is not possible to determine the extent to which the increase in discharges associated with bipolar disorder represents a true change in diagnostic composition as opposed to a change in diagnostic practices. Little attention has thus far been focused on early intervention in young people with bipolar disorder (40).
There was also a trend toward shorter hospitalizations for young people with self-inflicted injuries. Together with the trend toward limiting care to those with more severe diagnoses, the shortening of inpatient treatment may be placing inpatient staff under increased time pressures to locate appropriate outpatient care. Under these constraints, it is perhaps not surprising that an increasing proportion of inpatients were transferred to other inpatient facilities.
In the acute outpatient management of suicidal young people, encouraging results have been reported with rapid-response outpatient psychiatric teams (41), home-based interventions (42, 43), interpersonal problem-solving skills training (44), and brief cognitive behavior therapy for family members (45). It is not known whether access to these and other relevant outpatient mental health services has expanded to help compensate for the narrowing role of short-term hospitalization in the care of young people with intentional self-inflicted injuries.
Several changes occurred in the pattern of intentional self-injury methods. Methods associated with high case fatality rates, including gas asphyxiation, hanging/suffocating, and firearms (23), remained relatively uncommon, possibly because of deaths in the community or the emergency room before hospital admission. Although ingestions declined as a proportion of admissions for intentional self-injury, there were proportionate increases in ingestion of acetaminophen, antidepressants, and opiates. These proportionate increases, together with proportionate decreases in barbiturate and salicylate ingestions, may reflect changes in the general use of these substances (46). The increase in acetaminophen ingestion is especially noteworthy because it poses a serious risk of potentially fatal hepatic toxicity (47) that may not be appreciated by young people (48).
During the study period, there was also an increase in the inpatient treatment of intentional self-inflicted injury involving cutting. Self-mutilation in young people tends to have a very low potential for lethality (23). In the United States, six adolescents (age range: 15–19 years) committed suicide by injury with a sharp object in 2000 (12). As compared with other types of self-injury, self-mutilation is clinically associated with greater patient perceived likelihood of rescue (13), lower perceived certainty of death (13), and lower rates of mood disorders (49). When these presumably less clinically severe discharges were excluded from the analysis, there was a statistically significant decline in the rate of youths hospitalized with intentional self-injury: from 47.2 to 39.4 discharges per 100,000 youth.
This study has several limitations. First, diagnostic data are only a crude index of illness severity and risk of subsequent suicide. No information was available concerning several known suicide risk factors in young people including prior suicide attempts (50), precipitating stressful life events (51, 52), access to firearms (2), and family psychiatric history (51, 53). Second, no independent assessment was available of the clinical diagnostic codes. A growth in managed care and concepts of medical necessity (54) may have resulted in a tendency to code patients as having more severe psychiatric disorders to justify admission under precertification utilization management policies. Third, the data permit no means of distinguishing admissions primarily for medical care associated with attempted suicide from admissions primarily for treatment of the underlying psychiatric disturbance. Fourth, the reported rates measure the total number of hospitalizations rather than the individual persons hospitalized. It would be useful to quantify the extent and characteristics of repeat admissions for attempted suicide. Fifth, stigma associated with suicide attempts may have resulted in systematic underreporting of intentional self-injury. Last, the analysis was limited to admissions to short-term community hospitals and does not include the large number of young people admitted directly to other types of inpatient facilities (55).
Over the last several years, there has been little change in the overall rate of community hospital inpatient hospitalizations of children and adolescents with intentional self-inflicted injuries. However, the proportion of young self-injurious inpatients with high-risk conditions (including depressive, bipolar, and substance use disorders) has increased, and the length of their inpatient stays has declined. These changes, especially in light of increasing injurious youth suicide attempts in the community, indicate that inpatient care may have assumed a narrower and more limited role in the treatment of suicidal young people. As mental health care professionals have come to rely less extensively on inpatient treatment for the acute management of self-injurious young people, community service needs have likely increased for rapid-response, crisis-oriented outpatient care.
 |
 |
 |
 |
 |
Received Jan. 14, 2004; revision received June 9, 2004; accepted Aug. 11, 2004. From the New York State Psychiatric Institute/Department of Psychiatry, College of Physicians and Surgeons of Columbia University, New York; and the University of Pennsylvania School of Social Work, Philadelphia. Address correspondence and reprint requests to Dr. Olfson, New York State Psychiatric Institute/Department of Psychiatry, College of Physicians and Surgeons of Columbia University, 1051 Riverside Dr., New York, NY 10032; [email protected] (e-mail).
1. Safer DJ: A comparison of studies from the United States and Western Europe on psychiatric hospitalization referrals for youths exhibiting suicidal behavior. Ann Clin Psychiatry 1996; 8:161–168Crossref, Medline, Google Scholar
2. Brent DA, Kupfer DJ, Bromet EJ, Dew MA: The assessment and treatment of patients at risk for suicide, in American Psychiatric Press Review of Psychiatry, vol 7. Edited by Frances AJ, Hales RE. Washington, DC, American Psychiatric Press, 1988, pp 353–385Google Scholar
3. Stewart SE, Manion IG, Davidson S: Emergency management of the adolescent suicide attempter: a review of the literature. J Adolesc Health 2002; 30:312–325Crossref, Medline, Google Scholar
4. Greenhill LI, Waslick B: Management of suicidal behavior in children and adolescents. Psychiatr Clin North Am 1997; 20:641–666Crossref, Medline, Google Scholar
5. Morrissey RF, Dicker R, Abikoff H, Alvir JM, DeMarco A, Koplewicz HS: Hospitalizing the suicidal adolescent: an empirical investigation of decision-making criteria. J Am Acad Child Adolesc Psychiatry 1995; 34:902–911Crossref, Medline, Google Scholar
6. Mark TL, Coffey RM, King E, Harwood H, McKusick D, Genaurdi J, Dilonardo J, Buck JA: Spending on mental and substance abuse treatment, 1987–1997. Health Aff 2000; 19:108–120Crossref, Google Scholar
7. Hall RC, Platt DE, Hall RCW: Suicide risk assessment: a review of risk factors for suicide in 100 patients who made severe suicide attempts: evaluation of suicide risk in a time of managed care. Psychosomatics 1999; 40:18–27Crossref, Medline, Google Scholar
8. Martin A, Leslie D: Psychiatric inpatient, outpatient, and medication utilization and costs among privately insured youths, 1997–2000. Am J Psychiatry 2003; 160:757–764Link, Google Scholar
9. Rissmiller DJ, Steer R, Ranieri WF, Rissmiller F, Hogate P: Factors complicating cost containment in the treatment of suicidal patients. Hosp Community Psychiatry 1994; 45:782–788Abstract, Google Scholar
10. Overview of the HCUP Nationwide Inpatient Sample. Rockville, Md, Agency for Healthcare Research and Quality, May 2002Google Scholar
11. US Census Bureau: American FactFinder. http://factfinder.census.gov/Google Scholar
12. Centers for Disease Control: Wonder Mortality Data Request Screen. http://wonder.cdc.gov/mortICD9J.htmlGoogle Scholar
13. Stanley B, Gameroff MJ, Michalsen V, Mann JJ: Are suicide attempters who self-mutilate a unique population? Am J Psychiatry 2001; 158:427–432Link, Google Scholar
14. United States Department of Labor, Bureau of Labor Statistics, Consumer Price Index. http://www.bls.gov/cpi/home.htmGoogle Scholar
15. Shah BV, Barnwell BG, Bieler GS: SUDAAN User’s Manual, Release 7.5. Research Triangle Park, NC, Research Triangle Institute, 1997Google Scholar
16. Grunbaum JA, Kann L, Kinchen SA, Williams B, Ross JG, Lowry R, Kolbe L: Youth risk behavior surveillance—United States, 2001. MMWR Surveill Summ 2002; 51:1–62Medline, Google Scholar
17. Brener ND, Krug EG, Simon T: Trends in suicide ideation and suicidal behavior among high school students in the United States, 1991–1997. Suicide Life Threat Behav 2000; 30:304–312Medline, Google Scholar
18. Lewinsohn PM, Rohde P, Seeley JR, Baldwin CL: Gender differences in suicide attempts from adolescence to young adulthood. J Am Acad Child Adolesc Psychiatry 2001; 40:427–434Crossref, Medline, Google Scholar
19. Hawton K, Hall S, Simkin B, Bale K, Bond A, Codd S, Stewart A: Deliberate self-harm in adolescents: a study of characteristics and trends in Oxford, 1990–2000. J Child Psychol Psychiatry 2003; 44:1191–1198Crossref, Medline, Google Scholar
20. Beautrais AL: Suicide and serious suicide attempts in youth: a multiple-group comparison study. Am J Psychiatry 2003; 160:1093–1099Link, Google Scholar
21. Wichstrom L, Rossow I: Explaining the gender difference in self-reported suicide attempts: a nationally representative study of Norwegian adolescents. Suicide Life Threat Behav 2002; 32:101–116Crossref, Medline, Google Scholar
22. Rancans E, Alka I, Renberg ES, Jacobsson L: Suicide attempts and serious suicide threats in the city of Riga and resulting contacts with medical services. Nord J Psychiatry 2001; 55:279–286Crossref, Medline, Google Scholar
23. Spicer RS, Miller TR: Suicide acts in 8 states: incidence and case fatality rates by demographics and method. Am J Public Health 2000; 90:1885–1891Crossref, Medline, Google Scholar
24. Funk JB, Baldacci HB, Pasold T, Baumgardner J: Violence exposure in real-life, video games, television, movies, and the internet: is there desensitization? J Adolesc 2004; 27:23–39Crossref, Medline, Google Scholar
25. Anderson CA: An update on the effects of playing violent video games. J Adolesc 2004; 27:113–122Crossref, Medline, Google Scholar
26. Nock MK, Kazdin AE: Examination of affective, cognitive, and behavioral factors and suicide-related outcomes in children and young adolescents. J Clin Child Adolesc Psychol 2002; 31:48–58Crossref, Medline, Google Scholar
27. Kaminiski RA, Stormshack EA, Good RH, Goodman MR: Prevention of substance abuse with rural head start children and families: results of project STAR. Psychol Addict Behav 2002; 16(4 suppl): S11-S26Google Scholar
28. Bierman KLL, Coie JD, Dodge KA, Greenberg MT, Lochman JE, McMahon RJ, Pinderhughes EE (Conduct Problems Prevention Research Group): Using the Fast Track Randomized Prevention Trial to test the early-starter model of the development of serious conduct problems. Dev Psychopathol 2002; 13:925–943Google Scholar
29. Flanagan KS, Bierman KL, Kam CM: Identifying at-risk children at school entry: the usefulness of multibehavioral problem profiles. J Clin Child Adolesc Psychol 2003; 32:396–407Crossref, Medline, Google Scholar
30. Brent DA, Baugher M, Bridge J, Chen T, Chiappetta L: Age- and sex-related risk factors for adolescent suicide. J Am Acad Child Adolesc Psychiatry 1999; 38:1497–1505Crossref, Medline, Google Scholar
31. Apter A, Bleich A, King RA, Kron S, Fluch A, Kotler M, Cohen DJ: Death without warning? a clinical postmortem study of suicide in 43 Israeli adolescent males. Arch Gen Psychiatry 1993; 50:138–142Crossref, Medline, Google Scholar
32. Shaffer D, Gould MS, Fisher P, Trautman P, Moreau D, Kleinman M, Flory M: Psychiatric diagnosis in child and adolescent suicide. Arch Gen Psychiatry 1996; 53:339–348Crossref, Medline, Google Scholar
33. Lucas CP, Zhang H, Fisher PW, Shaffer D, Riger DA, Narrow WE, Bourdon K, Dulcan MK, Canino G, Rubio-Stipec M, Lahey BB, Friman P: The DISC Predictive Scales (DPS): efficiently screening for diagnoses. J Am Acad Child Adolesc Psychiatry 2001; 40:443–449Crossref, Medline, Google Scholar
34. Aseltine RH, DeMartino R: An outcome evaluation of the SOS Suicide Prevention Program. Am J Public Health 2004; 94:446–451Crossref, Medline, Google Scholar
35. Lewinsohn PM, Seeley JR, Buckley ME, Klein DN: Bipolar disorder in adolescence and young adulthood. Child Adolesc Psychiatr Clin North Am 2002; 11:461–475Crossref, Medline, Google Scholar
36. Brent D, Perper J, Moritz G, Allman C, Friend A, Roth C, Schweers J, Friend A, Roth C, Schweers J, Balach L, Baughm M: Psychiatric risk factors for adolescent suicide: a case-control study. J Am Acad Child Adolesc Psychiatry 1993; 32:521–529Crossref, Medline, Google Scholar
37. State RC, Altshuler LL, Frye MA: Mania and attention deficit hyperactivity disorder in a prepubertal child: diagnostic and treatment challenges (case conf). Am J Psychiatry 2002; 159:918–925Link, Google Scholar
38. Kim EY, Miklowitz DJ: Childhood mania, attention deficit hyperactivity disorder and conduct disorder: a critical review of diagnostic dilemmas. Bipolar Disord 2002; 4:215–225Crossref, Medline, Google Scholar
39. Krasa NR, Tolbert HA: Adolescent bipolar disorder: a nine-year experience. J Affect Disord 1994; 30:175–184Crossref, Medline, Google Scholar
40. Conus P, McGorry PD: First-episode mania: a neglected priority for early intervention. Aust NZ J Psychiatry 2002; 36:158–172Crossref, Medline, Google Scholar
41. Greenfield B, Larson C, Hechtman L, Rousseau C, Platt R: A rapid-response outpatient model for reducing hospitalization rates among suicidal adolescents. Psychiatr Serv 2002; 53:1574–1579Link, Google Scholar
42. Harrington R, Kerfoot M, Dyer E, McNiven F, Gill F, Harrington V, Woodham A, Byford S: Randomized trial of a home-based family intervention for children who have deliberately poisoned themselves. J Am Acad Child Adolesc Psychiatry 1998; 37:512–518Crossref, Medline, Google Scholar
43. Kerfoot M, Harrington R, Dyer E: Brief home-based intervention with young suicide attempters and their families. J Adolesc 1995; 18:557–568Crossref, Google Scholar
44. McLeavey B, Daly R, Ludgate J, Murray CM: Interpersonal problem-solving skills training in the treatment of self-poisoning patients. Suicide Life Threat Behav 1994; 24:382–394Medline, Google Scholar
45. Piacentini J, Rotherman-Borus MJ, Gillis JR, Graae F, Trautman P, Cantwell C, Garcia-Leeds C, Shaffer D: Demographic predictors of treatment attendance among adolescent suicide attempters. J Consult Clin Psychol 1995; 63:469–473Crossref, Medline, Google Scholar
46. Malmstrom M, Sundquist J, Ekedahl A, Johansson SE: Prescribing patterns for analgesics in relation to underprivileged area (UPA) score, mortality, and suicide in 33 municipalities in the providence of Skane, southern Sweden. Soc Psychiatry Psychiatr Epidemiol 1999; 344:259–264Google Scholar
47. Schiodt FV, Rochling FA, Casey DL, Lee WM: Acetaminophen toxicity in an urban county hospital. N Engl J Med 1997; 337:1112–1117Crossref, Medline, Google Scholar
48. Myers WC, Otto TA, Harris E, Diaco D, Moreno A: Acetaminophen overdose as a suicidal gesture: a survey of adolescents’ knowledge of its potential for toxicity. J Am Acad Child Adolesc Psychiatry 1992; 31:686–690Crossref, Medline, Google Scholar
49. Fulwiler C, Forbes C, Santangelo SL, Folstein M: Self-mutilation and suicide attempt: distinguishing features in prisoners. J Am Acad Psychiatry Law 1997; 25:69–77Medline, Google Scholar
50. Renaud J, Brent DA, Birmaher B, Chiappetta L, Bridge J: Suicide in adolescents with disruptive disorders. J Am Acad Child Adolesc Psychiatry 1999; 38:846–851Crossref, Medline, Google Scholar
51. Gould MS, Fisher P, Parides M, Flory M, Shaffer D: Psychosocial risk factors of child and adolescent completed suicide. Arch Gen Psychiatry 1996; 53:1155–1162Crossref, Medline, Google Scholar
52. Marttunen MJ, Aro HM, Lonnqvist JK: Precipitant stressors in adolescent suicide. J Am Acad Child Adolesc Psychiatry 1993; 32:1178–1183Crossref, Medline, Google Scholar
53. Shafii M, Carrigan S, Whittinghill JR, Derrick A: Psychological autopsy of completed suicide in children and adolescents. Am J Psychiatry 1985; 142:1061–1064Link, Google Scholar
54. Dana RH, Conner MG, Allen J: Quality of care and cost-containment in managed mental health: policy, education, research, advocacy. Psychol Rep 1996; 79:1395–1422Crossref, Medline, Google Scholar
55. Manderscheid RW, Henderson MJ (eds): Mental Health, United States, 2000: DHHS Publication SMA 02–3537. Washington, DC, Center for Mental Health Services, 2001Google Scholar



