Pathways to PTSD, Part I: Children With Burns
Abstract
OBJECTIVE: The goal of this study was to develop a model of risk factors for posttraumatic stress disorder (PTSD) in a group of acutely burned children. METHOD: Seventy-two children between the ages of 7 and 17 who were admitted to the hospital for an acute burn were eligible for study. Members of families who consented completed the Child PTSD Reaction Index, the Multidimensional Anxiety Scale for Children, and other self-report measures of psychopathology and environmental stress both during the hospitalization and 3 months following the burn. A path analytic strategy was used to build a model of risk factors for PTSD. RESULTS: Two pathways to PTSD were discerned: 1) from the size of the burn and level of pain following the burn to the child’s level of acute separation anxiety, and then to PTSD, and 2) from the size of the burn to the child’s level of acute dissociation following the burn, and then to PTSD. Together these pathways accounted for almost 60% of the variance in PTSD symptoms and constituted a model with excellent fit indices. CONCLUSIONS: These findings support a model of complex etiology for childhood PTSD in which two independent pathways may be mediated by different biobehavioral systems.
Approximately 1.25 million individuals received burn injuries in the United States in 1992 (1). Fire is the third leading cause of unintentional injuries in children (2). Not surprisingly, burns were among the first types of trauma identified as leading to traumatic stress reactions in adults, and early burn research contributed to the original classification of posttraumatic stress disorder (PTSD) in DSM-III (3–5). Early studies of burned children alerted researchers and clinicians to the importance of attending to their psychiatric needs (6, 7). In one of the first studies of the prevalence of psychiatric diagnoses, 30% of the children interviewed more than 6 months after a severe burn had met the DSM-III criteria for PTSD at some point after their burn. These authors also reported higher prevalences of overanxious disorder, phobias, and enuresis in the children with burns than in a nonburn comparison group (8, 9). However, as little is known about the etiology of PTSD in children with burns, there is a great need for risk factor studies. Further, as burned children are accessible for study shortly after their trauma and, by virtue of their ongoing need for medical and surgical care, can be readily followed over time, they are ideally suited to prospective, longitudinal research designs. Such designs are necessary for the advancement of the understanding of risk factors for PTSD (10). In this study we attempted to build a model of risk factors for PTSD symptoms in burned children by assessing them shortly after the burn and then 3 months following this assessment.
Research has focused on the anxiety/arousal and the dissociative symptoms expressed in the acute aftermath of a trauma. The importance of these symptom clusters is formalized in DSM-IV with the addition of acute stress disorder. Acute stress disorder is the psychopathological response in the immediate aftermath of a traumatic event that occurs until 1 month following the trauma and includes both anxiety and dissociative symptoms as necessary components of this diagnosis. Daviss and colleagues (11) and Koplin Winston and colleagues (12) reported a broad range of acute stress disorder symptoms in separate cohorts of injured children. Numerous studies have documented the higher prevalence of PTSD in those initially diagnosed with acute stress disorder (13–15).
There is, however, considerable controversy over which symptom cluster, anxiety or dissociation, is more predictive of PTSD and, regarding the diagnosis of acute stress disorder, whether dissociation should be included as a distinct symptom cluster at all. If dissociative symptoms are required in the diagnosis of acute stress disorder, many individuals who suffer from only anxiety symptoms may not receive adequate attention (16, 17). Further, it has been argued that dissociative symptoms are not necessarily more predictive of PTSD than are anxiety symptoms (16). On the other hand, evidence suggests that individuals who dissociate around the time of trauma are at high risk of developing PTSD (18–21). The controversy over the relative importance of anxiety and dissociative symptoms is also important for another reason: these two groupings of symptoms may be the phenotypes of different biobehavioral systems related to PTSD (22, 23). Clarity regarding the relationship between these groups of symptoms and their biological underpinnings may be critical for identifying children at risk and refining immediate interventions following a trauma.
Of the anxiety symptoms, we regard separation anxiety as particularly important for the population of children hospitalized with burns. The nature of burn injury and its long and stressful hospital course frequently mean separations of the child and the parents at a time when the child has a great need for their help and comfort.
In the current study we used path analytic techniques to evaluate the ways in which pretrauma variables, trauma characteristics, and reactions in the immediate aftermath of a trauma are related to later PTSD symptoms. As described, anxiety and dissociative reactions in the wake of a trauma have frequently been identified as important components of the acute trauma response, although there is considerable controversy over which is more strongly related to deleterious long-term outcomes. Consequently, a main goal of the current study was to assess the relative importance of anxiety and dissociation in the immediate aftermath of a burn.
Method
Participants
The participants were drawn from a group of children admitted to Shriners Burns Hospital in Boston for an acute burn. All children ages 7 to 17 years were eligible to participate unless they or their parents did not speak sufficient English to complete the study instruments. Of 116 eligible children, 72 (62%) participated. Of the 44 children who did not, 26 had families that declined to participate and 18 were discharged before we were able to obtain consent. The mean age of the participants was 11.20 years (SD=3.51); 24 were girls and 48 were boys. The average length of stay was 25 days (SD=23). The mean amount of body surface area burned was 17.58% (range=1%–85%). The children were interviewed an average of 10 days after admission (range=2–26 days).
Procedures
Within 3 days of hospitalization or when the child was considered medically stable (e.g., did not have a delirium, did not have an active infection, and was not receiving mechanical ventilation), the child and his or her parents were approached by one of the investigators (C.L.) and introduced to the study. After complete description of the study, written informed consent and assent were obtained from the parents and child, respectively. On the same day that consent and assent were obtained, the child was interviewed and answered questions about his or her traumatic stress responses and the child’s primary nurse answered questions about the child’s dissociative symptoms (interview and questionnaires are described in the following).
Follow-up assessments consisting of the same interviews and questionnaires were completed by a trained research associate (N.C. or E.H.) at the participant’s home 3 months later.
Measures
Child measures
The Child PTSD Reaction Index (24) is a 20-item semistructured interview that assesses posttraumatic symptoms in children. Its interrater reliability is high (Cohen’s kappa=0.88). Its validity is supported by the finding that children who are known to have PTSD have much higher scores on this instrument (24). The score on the Child PTSD Reaction Index was the main dependent variable in this study.
The Multidimensional Anxiety Scale for Children (25) is a 39-item self-report measure of pediatric anxiety symptoms. In a psychometric study of the scale, the mean intraclass correlation coefficients at 3 weeks and 3 months were 0.79 and 0.93, respectively, demonstrating satisfactory to excellent test-retest reliability (25). Factor analytic studies of the scale have shown a variety of independent scales, including “harm avoidance,” “separation anxiety,” and “physical symptoms.” The separation anxiety scale of the Multidimensional Anxiety Scale for Children was our index of separation anxiety.
The Colored Analogue Pain Scale (26) is a pocket-sized visual analogue instrument on which the child slides a marker along a 10-cm line that shows an increasing intensity of red color corresponding to increased intensity of current pain. This instrument has been used with many groups of children who have pain. Children with more painful syndromes score higher on this instrument than do children with less painful syndromes. The Colored Analogue Pain Scale has been found to be easier to administer than other visual analogue scales.
Nurse measures
The numbing and dissociation scale of the Child Stress Disorders Checklist (27) is a measure of acute dissociative symptoms based on observer report. This 8-item scale assesses the dissociative dimension of the child’s acute and posttraumatic stress response. Internal consistency was found to be 0.75 (Cronbach’s alpha). Test-retest reliability, calculated by correlating scores reported by the parents 2 days apart, was found to be 0.72 (intraclass correlation). In the current study, the child’s primary nurse completed the Child Stress Disorders Checklist in regard to the child’s dissociative symptoms.
The total body surface area burned was the percentage recorded by the attending surgeon in the child’s medical record.
Data Analysis
We used a path analytic strategy similar to that used by Shalev et al. (20) in another prospective study of acutely traumatized individuals. As this strategy is based on a prospective longitudinal method, the directionality of many of the paths was constrained by the time at which the variables were assessed. Accordingly, we divided variables into the following: 1) PTSD symptoms (our main dependent variable, derived from the Child PTSD Reaction Index), 2) posttraumatic variables (variables assessed at the 3-month follow-up), 3) peritraumatic variables (variables assessed shortly after the trauma), 4) trauma exposure variable (percentage of body surface area burned), and 5) pretrauma variables (variables related to the child or family from before the trauma).
A series of hierarchically nested ordinary least squares multiple regression analyses were used to estimate direct and indirect effects among variables. The first step was to predict the dependent variable (PTSD symptoms). From the remaining variables, we chose combinations of variables that accounted for a high percentage of the variance in PTSD symptoms (high R2 value), guided by our theoretical model of PTSD and constrained by the strength of bivariate relationships (all bivariate relationships with r>0.30 and p<0.01). Accordingly, we chose two primary variables (i.e., separation anxiety and dissociative symptoms measured in the hospital) that together accounted for 59% of the variance of PTSD (R2=0.59). Once these two variables were chosen, antecedent variables could be identified in order to place separation anxiety and dissociation in the roles of mediators. Again, we were guided by theory and the strength of the bivariate relationships, and we were further constrained by temporal relationships. The direction of the relationships chosen had to make temporal sense (e.g., peritraumatic dissociation could not lead to the size of the burn). In this way we generated a network of associations among variables that, as we will discuss, adds important understanding to the unfolding of PTSD over time.
Problems related to missing data can reduce the number of subjects for a particular analysis to a less than optimal level. We employed the statistical package M Plus 2.1 (28) with full information maximum likelihood estimation to retain the full number of subjects for each analysis. M Plus is preferred since it is able to use the full information maximum likelihood procedure in concert with the Satorra-Bentler correction for nonnormal data. (See the work of McArdle [29] and Graham et al. [30] for discussions of the advantages of maximum-likelihood-based methods for incomplete data over more traditional listwise and pairwise deletion procedures.)
Results
Table 1 presents the mean values and standard deviations for the variables used in our path analysis, and Table 2 presents a correlation matrix of these variables.
Figure 1 illustrates the network of associations among variables. The results of the path analysis indicate two direct pathways to PTSD. These pathways are from 1) acute separation anxiety (beta=0.68) and 2) acute dissociation (beta=0.26). In addition, separation anxiety served as a mediator between the age of the child and PTSD and between pain measured shortly after the burn and PTSD. Moreover, both separation anxiety and dissociation mediated the relationship between total burn area and PTSD. Together these pathways account for 59% of the variance in PTSD. The overall model yielded strong fit indices (χ2=2.0, df=6, p=0.92; comparative fit index=1.00; Tucker-Lewis index=1.00; and root mean square error of approximation=0.00).
Discussion
Two pathways to PTSD symptoms were found. One pathway was mediated by separation anxiety, the other by acute dissociative responses. The magnitude of the trauma, measured by the size of the burn, was not related to PTSD directly but exerted its influence indirectly through both pathways. The pathway mediated by separation anxiety was influenced by the acute pain response. This pathway was also influenced by the size of the burn and was inversely related to the age of the child. The pathway mediated by the acute dissociative response was influenced only by the size of the burn.
The independence of the anxiety and dissociation pathways to PTSD suggests the possibility that different biobehavioral systems contribute to PTSD. A number of researchers have drawn connections between the arousal/anxiety symptoms and the sympathetically mediated fight-or-flight response and between the symptoms of dissociation and the parasympathetically mediated “freeze” or “immobilization” response (22, 23, 31, 32). For example, Perry and colleagues have described the hierarchical response to threat in biological theories of children’s responses to trauma (22, 23). They described the initial fight-or-flight hyperarousal response in a child faced with an immediate threat and the following freeze-or-surrender immobilized response when the child cannot diminish the threat by means of the fight-or-flight response. The authors suggested that this freeze-or-surrender response occurs when a child is confronted by extreme threat and is helpless to respond. This response is phenotypically observed as dissociative symptoms (22). The fight-or-flight response is controlled by the sympathetic/HPA axis system, and the freeze/immobilization response is controlled by the parasympathetic nervous system (33). Porges has described the evolutionary foundations of this sequentially overwhelmed autonomic nervous system (33). Further, Bowlby (34, 35) has noted the critical interpersonal components of this threat response system in humans and nonhuman primates.
Anxiety/Arousal Pathway to PTSD
Bowlby stated, “Of the many fear arousing situations that a child, or older person, can foresee, none is likely to be more frightening than the possibility that an attachment figure will be absent or…unavailable when needed” (35, p. 201). In this study, the child’s level of acute separation anxiety was directly related to PTSD symptoms. Separation anxiety was influenced by the child’s age, the size of the burn, and the degree of pain experienced. As described, the nature of burn injury and the prolonged recovery process during hospitalization mandate stressful separations between the child and parents at a time when the child has a great need for their help and comfort. Thus, the children who experienced the most anxiety on separations were more likely to develop posttraumatic symptoms. Separation anxiety in children may be related to the evolutionarily driven reaction to the anticipated loss of the mother and of her protective function (36). As survival is a frequent concern of children on burn units, the need for soothing and reassurance from a parent is felt intensely by most burned children. This extreme arousal response to being burned, in pain, and alone is consistent with our data.
It is noteworthy that burn trauma has been considered a relatively impersonal trauma, as it is often not caused by another person. The importance of separation anxiety in the development of PTSD suggests that burn trauma has a significant interpersonal component. Specifically, burn trauma and the emotional distress underlying the question “Who will help me?” are integrally connected. This evidence thereby supports the notion that all trauma has an interpersonal element.
Dissociative Pathway to PTSD
Krystal has stated, “The switch from anxiety to the catatonoid response is the subjective evaluation of impending danger as one that cannot be avoided or modified. With the perception of fatal helplessness in the face of destructive danger, one surrenders to it” (37, pp. 114–115). In this study, the degree of dissociative symptoms measured shortly after the burn was found to be a direct predictor of PTSD symptoms. This replicates the results of many studies (18, 19), but we believe that it is the first to document this effect in children with burns. The independence of dissociation from separation anxiety is consistent with the hypotheses of Perry and others that the anxiety/arousal component of PTSD may be a phenotype of the sympathetically mediated fight-or-flight response, whereas the dissociative symptoms may be a phenotype of the parasympathetically mediated immobilization or freezing response. This response is described as phylogenetically very old and is characterized by the lack of vagal tone, bradycardia, and shutting down of responses, in order to conserve resources to maximize the chance of survival during situations of extreme threat. This type of response is thought to occur after exhaustion of other defensive behaviors, such as the fight-or-flight response, which is mediated by the sympathetic nervous system (33, 38, 39). Changes in vagal tone, a well-accepted marker of parasympathetic activity, have been associated with PTSD (40–42). It may be that situations of extreme life threat lead to the parasympathetically mediated shutting down of emotional responses, phenotypically observed as dissociative symptoms and prospectively related to PTSD. Parasympathetic nervous system activation was not, however, directly measured in this study.
It is notable that no direct relationship between separation anxiety and dissociation was found in our model. In fact, the bivariate association (Table 2) was negligible (r=0.13). As dissociative responses are hypothesized to follow anxiety/arousal responses when the fight-or-flight approach is ineffective, it would follow that anxiety would lead to dissociation. This dependence of dissociation on anxiety/arousal, but not vice versa, is reported in the accompanying article in this issue of the Journal(43). It is possible that variables that were not assessed (such as psychophysiology) may be mediating this relationship.
Regarding the controversy of whether acute anxiety or dissociation is the more important predictor of PTSD, our data suggest that both anxiety and dissociative symptoms independently contribute to the risk for PTSD.
Limitations
This study is limited by a relatively small number of subjects and a short longitudinal follow-up. The findings of two independent pathways to PTSD, and our interpretation that they suggest discrete biobehavioral systems, can be illuminated by studies that include psychophysiological and neuroendocrine measures.
Clinical Implications
These data have important implications for PTSD treatment and prevention. If symptoms of separation anxiety, pain, and dissociation can be identified in the acute aftermath of a trauma and strongly contribute to the risk of PTSD, then it is critical to assess these symptoms and to intervene accordingly. There are well-described psychosocial and biological interventions for anxiety, pain, and dissociation. Given the particular importance of separation anxiety, burn hospitals (and all pediatric intensive care units) must make every effort to keep parents and children together and to work with parents to increase their capacity to comfort their children. It is noteworthy that opiates are among the strongest inhibitors of the distress cry in young animals upon separation from mothers (35, 44). We have previously reported that the dose of morphine received by burned children in the hospital diminishes PTSD symptoms over time (45). It is possible that one mechanism for the diminution of PTSD over time in these children is the effect of the morphine on separation anxiety, as well as pain. If so, it would be a very specific intervention for one of our two pathways to PTSD.
 |
 |
Presented at the 18th annual meeting of the International Society for Traumatic Stress Studies, Baltimore, Nov. 7–10, 2002. Received Dec. 12, 2003; revision received July 20, 2004; accepted Aug. 2, 2004. From the Department of Child and Adolescent Psychiatry, Boston University School of Medicine; the Department of Psychiatry, Shriners Burns Hospital, Boston; and the Department of Psychiatry, Bronx VA Medical Center, Bronx, N.Y. Address correspondence and reprint requests to Dr. Saxe, Department of Child and Adolescent Psychiatry, Boston University School of Medicine, Dowling 1 North, 1 Boston Medical Center Place, Boston, MA 02118; [email protected] (e-mail). Supported by NIMH grant R01 MH-57370 and by Substance Abuse and Mental Health Services Administration grant U79 SM-54305 (Dr. Saxe).
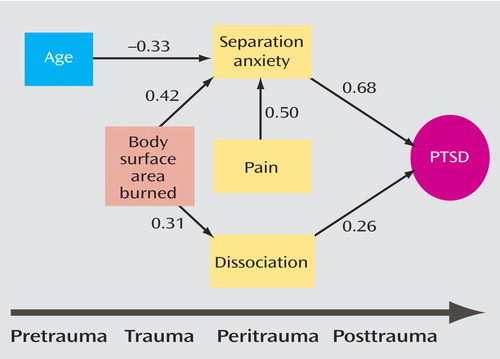
Figure 1. Path Analytic Model for the Development of PTSD in 72 Children With an Acute Burna
aThe values in the model are partial correlation coefficients (beta weights). R2=0.59.
1. Brigham PA, McLoughlin E: Burn incidence and medical care use in the United States: estimates, trends, and data sources. J Burn Care Rehabil 1996; 17:95–107Crossref, Medline, Google Scholar
2. Health and the American Child: Risks, Trends, and Priorities for the 21st Century. Washington, DC, Public Health Policy Advisory Board, 1999, p 25Google Scholar
3. Andreasen NJ: Neuropsychiatric complications in burn patients. Int J Psychiatry Med 1974; 5:161–171Crossref, Medline, Google Scholar
4. Andreasen NJ, Noyes R Jr, Hartford CE: Factors influencing adjustment of burn patients during hospitalization. Psychosom Med 1972; 34:517–525Crossref, Medline, Google Scholar
5. Andreasen NJ, Hartford CE, Knott JR, Canter A: EEG changes associated with burn delirium. Dis Nerv Syst 1977; 38:27–31Medline, Google Scholar
6. Seligman R: A psychiatric classification system for burned children. Am J Psychiatry 1974; 131:41–46Link, Google Scholar
7. Seligman R, Macmillan BG, Carroll SS: The burned child: a neglected area of psychiatry. Am J Psychiatry 1971; 128:52–57Link, Google Scholar
8. Stoddard FJ: Care of infants, children, and adolescents with burn injuries, in Child and Adolescent Psychiatry: A Comprehensive Textbook. Edited by Lewis M. Baltimore, Williams & Wilkins, 1995, pp 1016–1037Google Scholar
9. Stoddard FJ, Norman DK, Murphy JM, Beardslee WR: Psychiatric outcome of burned children. J Am Acad Child Adolesc Psychiatry 1989; 28:589–595Crossref, Medline, Google Scholar
10. Yehuda R: Risk Factors for Posttraumatic Stress Disorder. Washington, DC, American Psychiatric Press, 1999Google Scholar
11. Daviss WB, Racusin R, Fleischer A, Mooney D, Ford JD, McHugo G: Acute stress disorder symptomology during hospitalization for pediatric injury. J Am Acad Child Adolesc Psychiatry 2000; 39:569–575Crossref, Medline, Google Scholar
12. Winston FK, Kassam-Adams N, Vivarelli-O’Neill C, Ford J, Newman E, Baxt C, Stafford P, Cnaan A: Acute stress disorder symptoms in children and their parents after pediatric traffic injury. Pediatrics 2002; 109:e90Google Scholar
13. Harvey AG, Bryant RA: Two-year prospective evaluation of the relationship between acute stress disorder and posttraumatic stress disorder following mild traumatic brain injury. Am J Psychiatry 2000; 157:626–628Link, Google Scholar
14. Bryant RA, Harvey AG, Guthrie R, Moulds M: A prospective study of acute psychophysiological arousal, acute stress disorder, and posttraumatic stress disorder. J Abnorm Psychol 2000; 109:341–344Crossref, Medline, Google Scholar
15. Holeva V, Tarrier N, Wells A: Prevalence and predictors of acute stress disorder and PTSD following road traffic accidents: thought control strategies and social support. Behav Ther 2001; 32:65–83Crossref, Google Scholar
16. Bryant RA, Harvey AG: Acute Stress Disorder: A Handbook of Theory, Assessment, and Treatment. Washington, DC, American Psychological Association, 2000Google Scholar
17. Marshall RD, Spitzer R, Liebowitz MR: Review and critique of the new DSM-IV diagnosis of acute stress disorder. Am J Psychiatry 1999; 156:1677–1685Abstract, Google Scholar
18. Marmar CR, Weiss DS, Schlenger WE, Fairbank JA, Jordan BK, Kulka RA, Hough RL: Peritraumatic dissociation and posttraumatic stress in male Vietnam theater veterans. Am J Psychiatry 1994; 151:902–907Link, Google Scholar
19. Koopman C, Classen C, Spiegel D: Predictors of posttraumatic stress symptoms among survivors of the Oakland/Berkeley, Calif, firestorm. Am J Psychiatry 1994; 151:888–894Link, Google Scholar
20. Shalev AY, Peri T, Canetti L, Schreiber S: Predictors of PTSD in injured trauma survivors: a prospective study. Am J Psychiatry 1996; 153:219–225Link, Google Scholar
21. Difide JA, Barocas DA, Eskra D, Jaffe A, Roberts J, Yurt RW: Acute stress disorder following burn injury, in 1997 Annual Meeting Syllabus and Proceedings Summary. Washington, DC, American Psychiatric Association, 1997, symposium 72Google Scholar
22. Perry BD, Pollard RA, Blakley TL, Baker WL, Vigilante D: Childhood trauma, the neurobiology of adaptation, and use-dependent development of the brain: how states become traits. Infant Ment Health J 1995; 16:271–291Crossref, Google Scholar
23. Perry BD: Incubated in terror: neurodevelopmental factors in the “cycle of violence,” in Children in a Violent Society. Edited by Osofsky J. New York, Guilford, 1997, pp 124–148Google Scholar
24. Nader KO: Assessing trauma in children: self-reports of DSM Criteria B-D symptoms, in Assessing Psychological Trauma and PTSD. Edited by Wilson JP, Keane TM. New York, Guilford, 1996, pp 513–537Google Scholar
25. March JS, Parker JDA, Sullivan K, Stallings P, Conners K: The Multidimensional Anxiety Scale for Children (MASC): factor structure, reliability, and validity. J Am Acad Child Adolesc Psychiatry 1997; 36:554–565Crossref, Medline, Google Scholar
26. McGrath PA, Brigham MC: The assessment of pain in children and adolescents, in Handbook of Pain Assessment. Edited by Turk DC, Melzack R. New York, Guilford, 1992, pp 295–314Google Scholar
27. Saxe G, Chawla N, Stoddard F, Kassam-Adams N, Courtney D, Cunningham K, Lopez C, Hall E, Sheridan R, King D, King L: Child Stress Disorders Checklist: a measure of ASD and PTSD in Children. J Am Acad Child Adolesc Psychiatry 2003; 42:972–978Crossref, Medline, Google Scholar
28. Muthen LK, Muthen BO: M Plus Statistical Analysis With Latent Variables: User’s Guide. Los Angeles, Muthen & Muthen, 1998Google Scholar
29. McArdle JJ: Structural factor analysis with incomplete data. Multivariate Behav Res 994; 29:409–454Google Scholar
30. Graham JW, Hofer SM, Donaldson SI, MacKinnon DP, Schafer JL: Analysis with missing data in prevention research, in The Science of Prevention: Methodological Advances From Alcohol and Substance Abuse Research. Edited by Bryant KJ, Windle M, West SG. Washington, DC, American Psychological Association, 1997, pp 325–366Google Scholar
31. Perry BD: The memories of states: how the brain stores and retrieves traumatic experience, in Splintered Reflections: Images of the Body in Trauma. Edited by Goodwin JM, Attias R. New York, Basic Books, 1999, pp 9–38Google Scholar
32. Scaer R: The neurophysiology of dissociation and chronic disease. Appl Psychophysiol Biofeedback 2001; 26:73–91Crossref, Medline, Google Scholar
33. Porges SW: Orienting in a defensive world: mammalian modifications of our evolutionary heritage: a polyvagal theory. Psychophysiology 1995; 32:301–318Crossref, Medline, Google Scholar
34. Bowlby J: Attachment and Loss, vol I: Attachment. New York, Basic Books, 1969Google Scholar
35. Bowlby J: Attachment and Loss, vol II: Separation: Anxiety and Anger. New York, Basic Books, 1973Google Scholar
36. Panksepp J: Loneliness and the social bond: the brain sources of sorrow and grief, in Affective Neuroscience: The Foundations of Human and Animal Emotions. Edited by Panksepp J. New York, Oxford University Press, 1998, pp 261–279Google Scholar
37. Krystal H: Integration and Self-Healing: Affect-Trauma-Alexithymia. Hillsdale, NJ, Analytic Press, 1988Google Scholar
38. Porges SW, Matthews KA, Pauls DL: The biobehavioral interface in behavioral pediatrics. Pediatrics 1992; 90(5, part 2):789–797Google Scholar
39. Porges SW: Emotion: an evolutionary by-product of the neural regulation of the autonomic nervous system. Ann NY Acad Sci 1997; 807:62–77Crossref, Medline, Google Scholar
40. Sahar T, Shalev AY, Porges SW: Vagal modulation of responses to mental challenge in posttraumatic stress disorder. Biol Psychiatry 2001; 49:637–643Crossref, Medline, Google Scholar
41. Cohen H, Kotler M, Matar MA, Kaplan Z, Loewenthal U, Miodownik H, Cassuto Y: Analysis of heart rate variability in posttraumatic stress disorder patients. Biol Psychiatry 1998; 44:1054–1059Crossref, Medline, Google Scholar
42. Cohen H, Kotler M, Matar MA, Kaplan Z, Miodownik H, Cassuto Y: Power spectral analysis of heart rate variability in posttraumatic stress disorder patients. Biol Psychiatry 1997; 41:627–629Crossref, Medline, Google Scholar
43. Kaplow JB, Dodge KA, Amaya-Jackson L, Saxe GN: Pathways to PTSD, part II: sexually abused children. Am J Psychiatry 2005; 162:1305–1310Link, Google Scholar
44. Herman BH, Panksepp J: Ascending endorphin inhibition of distress covalization. Science 1982; 211:1060–1062Crossref, Google Scholar
45. Saxe G, Stoddard F, Courtney D, Cunningham K, Chawla N, Sheridan R, King D, King L: Relationship between acute morphine and the course of PTSD in children with burns. J Am Acad Child Adolesc Psychiatry 2001; 40:915–921Crossref, Medline, Google Scholar



