In This Issue
Bipolar Depression: If Antidepressants Work, Stick With Them
For an acute episode of depression in people with bipolar disorder, current guidelines recommend that antidepressant treatment be stopped 3-6 months after symptom remission to avoid induction of mania or rapid cycling of mood states. Findings from a prospective study by Altshuler et al. (p. 1252) raise questions about those guidelines. Among patients with bipolar depression who responded to 60 days of antidepressants and remained stable for 6 weeks, those who continued antidepressant treatment for 6 additional months had a substantially lower rate of relapse (36%) during the 1 year after response than those who stopped taking antidepressants (70%). Paradoxically, the rate of manic episodes was also lower, 13% versus 29%. These findings suggest that the guidelines for maintenance treatment of unipolar depression may ultimately extend to patients with bipolar disorder whose depressive episodes respond to antidepressants.
Divvying Up Treatment Dollars for Bipolar Disorder
Bipolar mood disorder affects approximately 1% of the U.S. population, but studies of insurance claims indicate much lower rates of treatment. Likewise, Peele et al. (p. 1286) found that 0.2% of people covered by 911 employer insurance plans, received services for bipolar disorder in 1996. Although they were 3% of the patients who were treated for psychiatric problems (including substance use disorders), they accounted for 12% of the nondrug expenses. The high cost was driven by disproportionate use of inpatient care: 21% of bipolar patients were hospitalized for psychiatric reasons during the year, making bipolar disorder the most expensive psychiatric diagnosis. In addition, these patients also had a higher rate of nonpsychiatric hospitalizations. Improved management of bipolar disorder is needed to reduce costs and improve patient functioning and well-being.
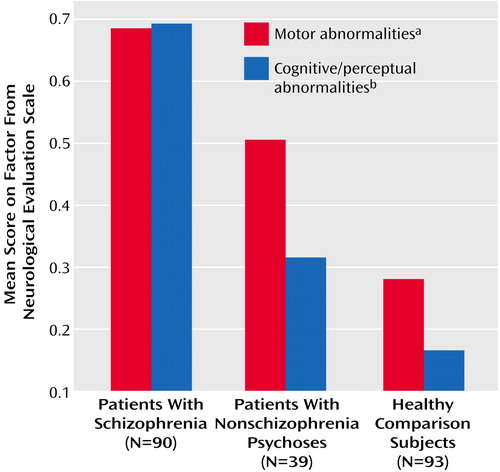
Possible Bedside Measures of Schizophrenia
Neurologic abnormalities in patients with schizophrenia have been called “soft signs” because they do not necessarily correspond to one type of psychotic disorder or to specific brain locations. Further, such findings could stem from antipsychotic medications or long-term illness. Keshavan et al. (p. 1298) studied neurologic abnormalities in patients with first-episode schizophrenia, healthy subjects, and patients with other psychotic disorders. The only tasks differentiating the schizophrenia patients from the other psychotic patients and the healthy subjects engaged cognitive functions and perception—memory, audiovisual integration, and recognition of face and hand stimuli. Among the schizophrenia patients but not the other groups, cognitive-perceptual performance correlated with volume of the cerebellum and left heteromodal association cortex, a composite reflecting a network of structures showing abnormalities in schizophrenia. If cognitive-perceptual soft signs are specific to schizophrenia and certain neuroanatomical locations, they may be useful as an inexpensive, quick part of neuropsychiatric assessments.
Dealing With Cocaine Craving: What Works?
For several abused substances, craving is an indicator of future use. A key goal of substance abuse treatment is to help patients abstain from drug use despite craving. How well do such treatments work? Weiss et al. (p. 1320) examined the relationship between craving and subsequent use among patients receiving one of four treatments for cocaine dependence. Each treatment included group drug counseling, but three added another type: individual drug counseling, supportive-expressive psychodynamic therapy, or cognitive therapy. Patients receiving individual drug counseling plus group counseling had the best cocaine use outcomes. In addition, this treatment combination attenuated the link between craving and use, i.e., greater craving was not associated with as much additional cocaine use. Individual drug counseling is more prescriptive than the other treatments (e.g., “Avoid places where you used to use drugs”), and this straightforward behavioral approach may help patients to abstain despite craving.
Binge Eating Less Common in Black Women
Large, epidemiologic studies of eating disorders have focused only on white women. Striegel-Moore et al. (p. 1326) did telephone interviews of 2,374 black and white young women ages 19–24. Subjects identified by telephone as having past or current eating disorders were interviewed in person. Among the more than 1,000 black women, no cases of anorexia nervosa were detected. Also, bulimia nervosa was only one-sixth as common in black women as among white women. Black women were significantly more likely to be obese, but fewer received diagnoses of binge eating disorder (1.4% versus 2.7%), which includes discrete episodes of overeating and psychological distress. Treatment for eating disorders was uncommon for white women (28.1% of those diagnosed) and even more so for black women (5.3%). This disparity points up the need for health care professionals to be alert to the possibility of eating disorders in black women.
Delusional Self-Portrait
Images in Psychiatry (p. 1251)

Delusional Self-Portrait



