Facial Expression Recognition in Adolescents With Mood and Anxiety Disorders
Abstract
OBJECTIVE: The authors examined facial expression recognition in adolescents with mood and anxiety disorders. METHOD: Standard facial emotion identification tests were given to youth with bipolar disorder (N=11) or DSM-IV anxiety disorders (N=10) and a group of healthy comparison subjects (N=25). RESULTS: Relative to the anxiety disorder and healthy comparison groups, the subjects with bipolar disorder made more emotion recognition errors when presented with faces of children. Unlike the anxious and comparison subjects, bipolar disorder youth were prone to misidentify faces as angry. No differences in emotion recognition errors were seen when the adolescents were presented with adult faces. CONCLUSIONS: A bias to misinterpret the facial expressions of peers as angry may characterize youth with bipolar disorder but not youth with anxiety disorders. This bias may relate to social impairment in youth with bipolar disorder.
Children with mood and anxiety disorders experience more peer rejection and social problems than healthy children (1). Research on adults suggests that misinterpretation of nonverbal cues such as facial expressions may contribute to such social impairment in patients with mood or anxiety disorders. Although findings are mixed, some studies suggest that adults with anxiety disorders or depression exhibit deficits or negative interpretive biases in facial expression identification (2–4). Additionally, manic adults identify facial expressions less accurately than do euthymic adults with bipolar disorder or healthy comparison subjects, and they may be biased to misinterpret them as positive (5, 6). Such findings have implications for research on social functioning and psychopathology as well as pathophysiology. For example, deficiencies or biases in facial emotion task performance may indicate psychopathology-related perturbations in the precisely mapped neural circuits engaged when viewing evocative facial displays (7).
Little is known about facial emotion recognition in youth with mood/anxiety disorders. Studies comparing anxious or depressed children to healthy children in terms of facial emotion recognition have found either poorer performance in affected children or no significant differences (8, 9). To our knowledge, no study has examined facial affect recognition in youth with bipolar disorder. Moreover, few studies have compared subjects’ performance when identifying emotions in peers versus adults.
We examined facial expression recognition in adolescents with anxiety disorders or bipolar disorder. We hypothesized that anxious and bipolar patients would perform more poorly than healthy comparison subjects, with bipolar patients, who are typically more impaired than anxiety patients, performing the most poorly.
Method
Eleven patients with bipolar disorder (mean age=13.73 years, SD=1.68) and 10 patients with DSM-IV anxiety disorders (mean age=12.9 years, SD=3.18) were diagnosed by using the Schedule for Affective Disorders and Schizophrenia for School-Age Children (K-SADS-PL) (10). The healthy comparison subjects consisted of 25 youth (mean age=13.52 years, SD=2.72) identified as being diagnosis-free according to the K-SADS-PL. Groups did not differ in terms of age or IQ. The bipolar disorder group consisted largely of boys (82%, N=9); fewer boys were in the anxious (50%, N=5) and comparison (40%, N=10) groups. Lifetime rates of attention deficit hyperactivity disorder were higher in the bipolar disorder group (82%, N=9) than in the anxiety (10%, N=1) or comparison (0%) groups. Lifetime oppositional defiant disorder was present in 36% of the bipolar disorder group (N=4) and 50% of the anxious group (N=5) and in none of the comparison subjects. Of the anxious group, 40% (N=4) had comorbid major depression; no other participants met major depression criteria. All anxious and comparison subjects were medication-free; all bipolar disorder subjects were receiving medication. The study was approved by the NIMH institutional review board; all subjects/parents provided written informed consent/assent.
Emotion identification skill was measured by using standardized photographs of children (N=24) and adults (N=24) displaying high- and low-intensity expressions of happiness, sadness, anger, or fear (11). Because of time constraints, only 44% (N=11) of the comparison subjects completed the adult faces task. Subjects also completed facial memory (12) and IQ (13) measures. Analysis of covariance was used to compare groups on continuous measures (alpha=0.05); performance on a facial memory task served as the covariate. Because the bipolar disorder group was largely male, analyses were rerun excluding girls. Because results were comparable with or without girls, only results including both genders are reported. Similarly, because analyses including only those comparison subjects who completed the adult faces task yielded similar results to those with the full study group, reported results on the child faces task are for the full study group.
Results
Groups did not differ in terms of facial memory performance (F=2.08, df=2, 43, p>0.05; eta2=0.09). However, because facial memory score correlated with errors in the recognition of emotional expressions in the faces of children (Pearson’s r=–0.34, df=44, p<0.03), facial memory score was included as a covariate.
No main effect of group was seen for recognition of emotional expressions in the faces of adults (F=1.52, df=2, 28, p>0.05; eta2=0.10). However, as seen in Figure 1, groups differed in their recognition of emotional expressions in the faces of children. Bipolar disorder subjects made more total errors (errors on faces with high and low emotional intensity combined) than did the other two groups. Bipolar disorder subjects’ poorer performance reflected a tendency to misidentify faces as angry. No anxious or comparison group members misidentified any face as angry, but 82% (N=9) of the bipolar disorder group made at least one such error.
A main effect of group also emerged for recognition of low-intensity emotional expressions in the faces of children (Figure 1). Again, the bipolar disorder group made more errors than other groups. Groups did not differ in their recognition of high-intensity emotional expressions (F=2.51, df=2, 42, p>0.05; eta2=0.11).
Discussion
Bipolar disorder youth performed worse than anxious adolescents and healthy comparison subjects on a facial emotion recognition task; comparison subjects and anxious subjects did not differ. Contrary to prior research with adults, no global positive or negative interpretive biases were evident for any group (2–6). However, bipolar patients were particularly likely to misinterpret the happy, sad, and fearful expressions of their peers—but not of adults—as angry. This pattern could relate to risk for negative peer interactions and may signal dysfunctional neural circuitry, a hypothesis amenable to testing by using neuroimaging techniques.
All bipolar subjects received medication because of ethical concerns, which complicates interpretations. This may have interfered with their emotion recognition performance, although it is unclear why medication might specifically impair identification of peer, but not adult, emotions. Additionally, more bipolar disorder subjects had comorbid behavior problems, which have been linked to hostile attribution biases (14).
Results indicate facial expression recognition deficits in bipolar youth, characterized by a bias to overperceive anger among peers. These findings suggest that biased interpretation of nonverbal cues as angry may relate to social difficulties in youth with bipolar disorder. Further study is needed to characterize interpersonal functioning in mood-disordered youth, especially those with bipolar disorder.
Received Sept. 6, 2002; revision received Nov. 20, 2002; accepted Dec. 27, 2002. From the National Institute of Mental Health, National Institutes of Health, Department of Health and Human Services. Address reprint requests to Dr. McClure, NIH NIMH/MAP, 15K North Dr., MSC 2670, Bethesda, MD 20892-2670; [email protected] (e-mail).
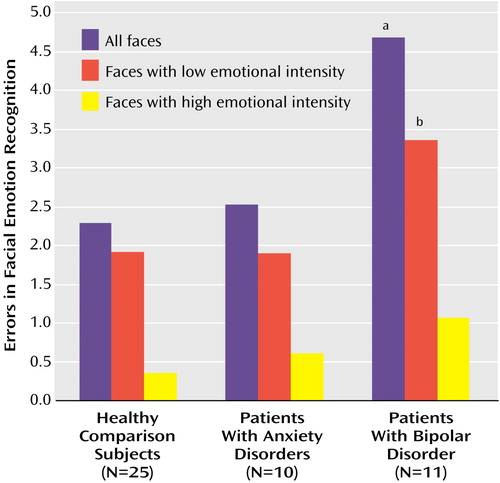
Figure 1. Recognition of Emotional Expressions in the Faces of Children by Healthy Comparison Subjects, Patients With Anxiety Disorder, and Patients With Bipolar Disorder
aSignificantly different from healthy and anxious subjects (F=5.96, df=2, 43, p<0.01; eta2=0.22).
bSignificantly different from healthy and anxious subjects (F=3.82, df=2, 42, p<0.05; eta2=0.15).
1. Rudolph KD, Hammen C, Burge D: Interpersonal functioning and depressive symptoms in childhood: addressing the issues of specificity and comorbidity. J Abnorm Child Psychol 1994; 22:355-371Crossref, Medline, Google Scholar
2. Feinberg TE, Rifkin A, Schaffer C, Walker E: Facial discrimination and emotional recognition in schizophrenia and affective disorders. Arch Gen Psychiatry 1986; 43:276-279Crossref, Medline, Google Scholar
3. Persad SM, Polivy J: Differences between depressed and nondepressed individuals in the recognition of and response to facial emotional cues. J Abnorm Psychol 1993; 102:358-368Crossref, Medline, Google Scholar
4. Veljaca KA, Rapee RM: Detection of negative and positive audience behaviours by socially anxious subjects. Behav Res Ther 1998; 36:311-321Crossref, Medline, Google Scholar
5. Lembke A, Ketter TA: Impaired recognition of facial emotion in mania. Am J Psychiatry 2002; 159:302-304Link, Google Scholar
6. Harmer CJ, Grayson L, Goodwin GM: Enhanced recognition of disgust in bipolar illness. Biol Psychiatry 2002; 51:298-304Crossref, Medline, Google Scholar
7. Haxby JV, Hoffman EA, Gobbini MI: Human neural systems for face recognition and social communication. Biol Psychiatry 2002; 51:59-67Crossref, Medline, Google Scholar
8. Lenti C, Giacobbe A, Pegna C: Recognition of emotional facial expressions in depressed children and adolescents. Percept Mot Skills 2000; 91:227-236Crossref, Medline, Google Scholar
9. Simonian SJ, Beidel DC, Turner SM, Berkes JL, Long JH: Recognition of facial affect by children and adolescents with social phobia. Child Psychiatry Hum Dev 2001; 32:137-145Crossref, Medline, Google Scholar
10. Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, Williamson D, Ryan N: Schedule for Affective Disorders and Schizophrenia for School-Age Children—Present and Lifetime Version (K-SADS-PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiatry 1997; 36:980-988Crossref, Medline, Google Scholar
11. Nowicki S, Duke MP: Individual differences in the nonverbal communication of affect: the Diagnostic Analysis of Nonverbal Accuracy Scale. J Nonverbal Behavior 1994; 18:9-35Crossref, Google Scholar
12. Reynolds CR, Bigler ED: Test of Memory and Learning. Austin, Tex, Pro-Ed, 1994Google Scholar
13. Wechsler D: Wechsler Abbreviated Scale of Intelligence. San Antonio, Tex, Psychological Corp, 1999Google Scholar
14. Dodge KA: Social cognition and children’s aggressive behavior. Child Dev 1980; 51:162-170Crossref, Medline, Google Scholar



