Long-Term Menstrual and Reproductive Function in Patients With Bulimia Nervosa
Abstract
OBJECTIVE: Menstrual dysfunction occurs frequently in patients with bulimia nervosa. Whether this is associated with diminished fertility is unknown. This study examined menstrual and reproductive function in bulimia nervosa patients retrospectively, with 10–15-year follow-ups. METHOD: A total of 173 women with bulimia nervosa were interviewed an average of 11.5 years (SD=1.9) after initial assessment with the Structured Clinical Interview for DSM-IV and a questionnaire about menstruation, pregnancy, and eating disorder symptoms. RESULTS: At baseline assessment, 38.2% of the subjects reported regular menses, and 4.6% reported amenorrhea. At follow-up, the rate of amenorrhea was 16.8% (2.9% because of pregnancy). At baseline, 34.7% of the subjects had experienced at least one pregnancy. At follow-up, 74.6% had been pregnant at least once, and 1.7% reported an inability to conceive. CONCLUSIONS: These results suggest that while menstrual irregularities are common, bulimia nervosa appears to have little impact on later ability to achieve pregnancy.
Menstrual dysfunction was identified as a complication of bulimia nervosa in the earliest description of that illness (1). Menstrual dysfunction may diminish over time (2, 3), but little is known about the impact of bulimia nervosa on fertility. Bulimic symptoms may decrease during pregnancy itself (4, 5); however, spontaneous abortion and low birth weight may also be more common for individuals with bulimia nervosa (4).
Information about the long-term course of menstrual dysfunction and fertility in patients with bulimia nervosa is of considerable clinical relevance. Patients with bulimia nervosa often ask whether their eating disorder will affect their future ability to conceive. Also, amenorrhea combined with malnutrition might put these patients at increasing risk for bone mineral loss.
This study examined menstrual function and fertility over 10–15 years in women with bulimia nervosa. We hypothesized that the rate of amenorrhea would decrease over time and that active symptoms of bulimia nervosa would predict difficulty achieving pregnancy.
Method
Women (N=173) who participated in a long-term outcome study of patients with bulimia nervosa completed assessments of menstrual and reproductive function. The ascertainment (90.1%) and participation (80.5%) rates for this study were very high (6). After complete description of the study to the subjects, written informed consent was obtained. Interviews were conducted either in person at a research office or at the subject’s home (54%) or over the telephone (46%). The Eating Disorders Questionnaire (7) was completed at baseline and follow-up examinations. At follow-up, the Structured Clinical Interview for DSM-IV Axis I Disorders (8) was also conducted. Additionally, all subjects completed a questionnaire that was developed for this study (available on request from the Dr. Crow) that assessed menstrual and reproductive history over their lifetime. The subjects’ weights were obtained either by self-report or, for subjects interviewed in person, by using a scale.
Time to pregnancy was calculated for all planned pregnancies. Chi-square statistics were calculated for categorical data. Analyses of variance were computed to examine group differences on continuous variables, and Pearson’s correlation coefficients were used to examine associations between continuous variables.
Results
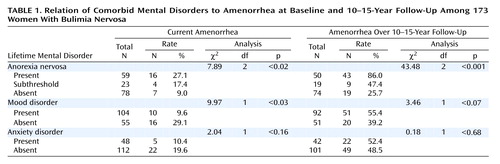
The mean time to follow-up was 11.5 years (SD=1.9), and the mean age at follow-up was 35.3 years (SD=5.1). The mean body mass index of the subjects was 21.2 (SD=2.7) at baseline and 22.0 (SD=3.6) at follow-up. At baseline, 38.2% (N=66) of the subjects reported regular menses. Irregular menses were reported by 29.5% (N=51) of the subjects, very irregular menses by 27.7% (N=48), and amenorrhea by 4.6% (N=8). At the follow-up assessment, 83.2% (N=144) of the subjects reported current menstruation, 2.9% (N=5) were pregnant, and 13.9% (N=24) had amenorrhea unrelated to pregnancy. Current amenorrhea was not associated with outcome of the eating disorder (17.1% [19 of 111] of the subjects in remission and 16.0% [8 of 50] of the subjects with current illness) (χ2=0.78, df=1, p=0.68). The relationships between amenorrhea and lifetime anorexia nervosa, mood, and anxiety disorders are shown in Table 1.
Amenorrhea outside of pregnancy was associated with a lower body mass index at follow-up (21.4) than was amenorrhea with pregnancy (23.1) (F=7.18, df=1, 128, p=0.008), but it was not associated with body mass index at baseline (21.0 versus 21.7, respectively) (F=2.80, df=1, 139, p<0.10). At baseline, 34.7% (N=60) of the subjects had had at least one pregnancy. At follow-up, this number had risen to 74.6% (N=129). Of the subjects who had never been pregnant (N=44, 25.4%), only 6.8% (N=3), or 1.7% of the total study group, had tried to conceive but were unable to. The mean number of months required to conceive for planned pregnancies was 3.7 (SD=7.8).
Two subjects who had experienced substantially longer times to conceive (36 and 60 months) represented outliers and were dropped from further analyses of time to conceive. Time to conceive was not significantly associated with lifetime histories of anorexia nervosa, anxiety disorder, mood disorder, or amenorrhea or with baseline body mass index. The likelihood of pregnancy did not differ in the subjects with (73.5% [36 of 49]) or without (76.1% [86 of 113]) a lifetime anxiety disorder (χ2=0.13, df=1, p=0.21) or in those with (73.6% [78 of 106]) or without (80.0% [44 of 55]) a lifetime mood disorder (χ2=0.81, df=1, p<0.37). However, the likelihood of pregnancy for those with a lifetime history of subthreshold anorexia nervosa (52.2% [12 of 23]) was significantly lower than that for subjects with lifetime history of full anorexia nervosa (78.3% [47 of 60]) or no history of anorexia nervosa (79.7% [63 of 79]) (χ2=7.75, df=2, p<0.03).
The number of pregnancies reported by each subject who had been pregnant ranged from 1 to 9 (modal number=2). The reported outcome of pregnancies was as follows: full-term live birth: 60.2% (194 of 322), premature live birth: 5.0% (N=16), spontaneous abortion: 11.2% (N=36), or induced abortion: 23.6% (N=76).
Discussion
The major finding of this study is that over 10–15 years of follow-up, prior or current bulimia nervosa may not have a major impact on fertility. While a comparison group was not available for study, the frequency of inability to conceive for our subjects was similar to general population norms (9), as were the rates of premature births and induced and spontaneous abortions (10). Finally, the ability to conceive was not associated with outcome of the eating disorder, nor were lifetime histories of anorexia nervosa, mood disorder, or anxiety disorder.
Baseline rates of menstrual irregularity were high, but amenorrhea was uncommon. Amenorrhea became more frequent by the follow-up period. Because menstrual status was ascertained differently at baseline and follow-up, it is unclear whether the rates of irregular menses changed. The resumption of menses has implications for fertility and may also be pertinent to the restoration of bone mineral density. Previous work in anorexia nervosa has demonstrated that both weight restoration and resumption of menses are important for replacing lost bone mineral density (11).
One might predict difficulties achieving pregnancy for women with bulimia nervosa on the basis of lower levels of luteinizing hormone (LH) or smaller spikes in LH levels (12, 13). Of note, these abnormalities have been seen in subjects of relatively normal weight. Abnormal LH secretion may be related to current weight that is less than 85% of the highest lifetime weight rather than current low body weight per se.
There are a number of strengths to this study, including a large study group, a high rate of ascertainment, a long follow-up period, and rigorous diagnostic methods. There are also several weaknesses to this study. The data were retrospective. Very few data were collected on these pregnancies; the availability of birth weights and Apgar scores would have been desirable. Without those, it is possible that while fertility rates appear unaffected by bulimia nervosa, other perinatal outcomes may be affected. Also, the subjects who refused to participate in the study may have experienced worse pregnancy outcomes than our subjects. In conclusion, the long-term outcome of menstrual function and fertility in women with bulimia nervosa appears relatively positive.
 |
Received Nov. 21, 2000; revision received Nov. 27, 2001; accepted Jan. 11, 2002. From the Department of Psychiatry, University of Minnesota Medical School. Address reprint requests to Dr. Crow, Department of Psychiatry, University of Minnesota Medical School, F282/2A West, 2450 Riverside Ave., Minneapolis, MN 55454-1495; [email protected] (e-mail). Supported in part by grants from the Minnesota Obesity Center (P30DK50456) and the McKnight Foundation.
1. Russell GFM: Bulimia nervosa: an ominous variant of anorexia nervosa. Psychol Med 1979; 9:429-448Crossref, Medline, Google Scholar
2. Copeland PM, Sacks NR, Herzog DB: Longitudinal follow-up of amenorrhea in eating disorders. Psychosom Med 1995; 57:121-126Crossref, Medline, Google Scholar
3. Abraham S: Sexuality and reproduction in bulimia nervosa patients over 10 years. J Psychosom Res 1998; 44:491-502Crossref, Medline, Google Scholar
4. Mitchell JE, Seim HC, Glotter D, Soll EA, Pyle RL: A retrospective study of pregnancy in bulimia nervosa. Int J Eat Disord 1991; 10:209-214Crossref, Google Scholar
5. Blais MA, Becker AE, Burwell RA, Flores AT, Nussbaum KM, Greenwood DN, Ekeblad ER, Herzog DB: Pregnancy: outcome and impact on symptomatology in a cohort of eating-disordered women. Int J Eat Disord 2000; 27:140-149Crossref, Medline, Google Scholar
6. Keel PK, Mitchell JE, Miller KB, Davis TL, Crow SJ: Long-term outcome of bulimia nervosa. Arch Gen Psychiatry 1999, 56:63-69Google Scholar
7. Mitchell JE, Hatsukami D, Eckert ED, Pyle RL: Eating Disorders Questionnaire. Psychopharmacol Bull 1985; 21:1025-1043Google Scholar
8. First MB, Spitzer RL, Gibbon M, Williams JBW: Structured Clinical Interview for DSM-IV Axis I Disorders, Patient Edition (SCID-P), version 2. New York, New York State Psychiatric Institute, Biometrics Research, 1995Google Scholar
9. Chandra A, Stephen EH: Impaired fecundity in the United States: 1982-1995. Fam Plann Perspect 1998; 30:34-42Crossref, Medline, Google Scholar
10. National Vital Statistics Report. Hyattsville, Md, US Department of Health and Human Services, April 1999Google Scholar
11. Iketani T, Kiriike N, Nakanishi S, Nakasuji T: Effects of weight gain and resumption of menses on reduced bone density in patients with anorexia nervosa. Biol Psychiatry 1995; 37:521-552Crossref, Medline, Google Scholar
12. Devlin MJ, Walsh BT, Katz JL: Hypothalamic-pituitary-gonadal function in anorexia nervosa and bulimia. Psychiatry Res 1989; 28:11-24Crossref, Medline, Google Scholar
13. Weltzin TE, Cameron J, Berga S, Kaye WH: Prediction of reproductive status in women with bulimia nervosa by past high weight. Am J Psychiatry 1994; 151:136-138Link, Google Scholar



