Childhood Adversity and the Endogenous Versus Nonendogenous Distinction in Women With Major Depression
Abstract
OBJECTIVE: Previous research has reported an association between childhood adversity and the nonendogenous subtype of depression. The present study sought to address this association by 1) investigating the relationship between depression subtype and different levels of childhood adversity and 2) examining the relative contribution of different types of childhood adversity to depression subtypes. METHOD: The authors conducted an investigator-based assessment of childhood adversity in a community group of 76 depressed women, 31 of whom met Research Diagnostic Criteria for endogenous depression. RESULTS: In contrast to previous studies, severe physical abuse, sexual abuse, antipathy, and neglect were significantly and preferentially associated with endogenous depression, as were both high and lax levels of supervision and discipline. In multivariate analyses, severe sexual abuse and a composite variable comprising antipathy and neglect were most strongly associated with endogenous depression. CONCLUSIONS: Implications of these findings in the context of the existing literature are discussed, and potential mediators of the relationship between childhood adversity and endogenous depression are presented as avenues for future research.
The last decade has seen a surge of interest in the role of childhood adversity in the onset of major depression. Prospective studies that have used methodologically rigorous, investigator-based assessments of childhood adversity have revealed that parental neglect, antipathy, and physical and sexual abuse are associated with up to double the risk of depression onset over a 1–3-year prospective period (1–3). These results represent an important advance because they characterize in detail the particular childhood experiences that best predict depression onset in a prospective fashion. The present study sought to extend this area of research by investigating whether childhood adversity is more strongly associated with the nonendogenous versus endogenous depression subtype.
Kraepelin originally characterized endogenous depression by 1) a distinct pattern of symptoms (e.g., anhedonia, morning worsening, psychomotor disturbance), 2) a presumed biogenetic etiology, and 3) an absence of precipitating stressors (4, 5). By contrast, the more loosely defined nonendogenous subtype was traditionally conceptualized as a reaction to environmental adversity. Many studies have failed to find consistent support for a preferential relationship of recent precipitating stressors to nonendogenous depression (see reference 6). However, only recently have studies begun investigating the role of childhood adversity in validating this subtype distinction.
Parker and colleagues (7, 8) found that poor parental care and high parental control (“affectionless control”), as measured by the Parental Bonding Instrument (9), were preferentially associated with nonendogenous depression. Other adverse childhood experiences were also associated with nonendogenous depression in these studies (e.g., dysfunctional parental marriage, emotional abuse, and rejection [9], but not childhood physical or sexual abuse [10]). This research provides important support for the distinction between nonendogenous and endogenous depression and suggests that nonendogenous depression may be more strongly influenced by the effects of childhood adversity than endogenous depression.
The present study addressed two intriguing issues raised by this prior research. First, while previous studies have reported a relationship between nonendogenous depression and the presence versus absence of childhood adversity, it is unclear how gradations in the severity of childhood adversity relate to the distinction between subtypes. Therefore, the first goal of the present study was to investigate the relationship between nonendogenous versus endogenous depression and different levels of severity of several childhood adversity variables assessed by contextual interview methods (1).
Second, previous studies have examined only the univariate associations among particular adverse childhood experiences and depression onset or depression subtype. However, it is unclear which specific experiences emerge as most strongly associated with these outcomes in multivariate models. For example, is childhood neglect more strongly associated with nonendogenous depression than childhood physical or sexual abuse? Therefore, the second goal of the present study was to examine the relative contributions of different types of childhood adversity to depression subtypes.
Method
Participants
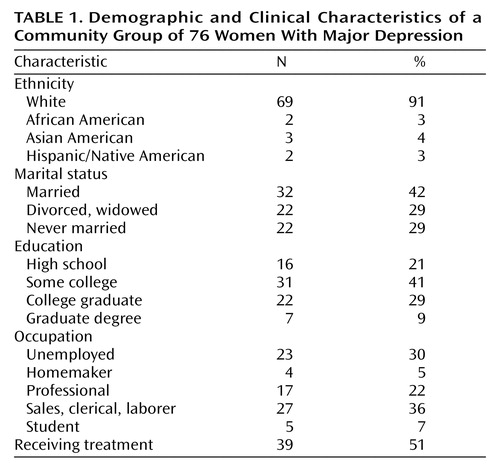
Seventy-six women, ranging in age from 18 to 70 (mean=37.3 years, SD=11.2), were recruited from a community in the Northwest United States through newspaper advertisements and requests on television news programs designed to target women experiencing a major depressive episode. Demographic and clinical characteristics of this study group are presented in Table 1. To be included in the study, women had to meet DSM-IV criteria for a current episode of primary, nonchronic, nonpsychotic, nonbipolar major depression and be 18 years of age or older. Women with a psychotic disorder, active substance abuse, or a medical disorder that could cause depression (e.g., hypothyroidism) were excluded. After complete description of the study to participants, written informed consent was obtained.
Procedure
A total of 245 women participated in an initial phone screening evaluation to determine eligibility for the study. Of these, 90 met study criteria and were scheduled for an interview. Excluded participants either did not meet criteria for major depression (N=80), had chronic depression (i.e., episode duration of longer than 2 years) (N=48), or had a comorbid exclusionary diagnosis (N=27). Nine women failed to attend the interview and declined to be rescheduled, and an additional five participants failed to meet criteria for major depression following a complete diagnostic interview, leaving 76 participants. These participants had experienced a median of five previous depressive episodes (range=1–20). More than one-half of the participants were receiving some sort of outpatient treatment in the community for their depression (Table 1).
At the clinic, participants underwent a diagnostic interview and the childhood adversity interview. Trained clinicians performed all interviews, and, in most cases, the same interviewer performed both interviews. The diagnostic interview was administered before the childhood adversity interview in order to prevent bias in the diagnosis of endogenous depression. In addition, information derived from the childhood adversity interview was rated by judges who were blind to the participants’ diagnoses. All participants were paid for their involvement in the study, given a list of treatment referrals, and invited to a free 3-hour cognitive behavior therapy workshop.
Diagnostic Measures
The diagnosis of major depression was determined after assessment with the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID) (11). During the SCID, endogenous versus nonendogenous depression was diagnosed on the basis of Research Diagnostic Criteria (RDC) (12). A diagnosis of endogenous depression requires the presence of at least two of the following symptoms: loss of interest, morning worsening, lack of reactivity, and incapacitation, with enough of the following to total at least six symptoms: loss of appetite, middle insomnia, early morning awakening, loss of interest in sex, excessive guilt, and psychomotor agitation or retardation. Forty-one percent (N=31) of participants met criteria for definite endogenous depression. The remaining 45 participants were categorized as having nonendogenous depression. The 17-item Hamilton Depression Rating Scale (13) was administered in order to determine the presence and severity of depression symptoms. Hamilton depression scale scores of the present participants (mean=18.26, SD=5.29) were consistent with those of most outpatient study groups reported in the literature.
Childhood adversity was assessed with the Childhood Experience of Care and Abuse scale (1), a semistructured interview that includes detailed questions about the quality of parental care and incidents of abuse from birth up to and including age 17. The Childhood Experience of Care and Abuse interview contains eight core scales: 1) antipathy (hostility and coldness directed toward the child); 2) neglect (indifference to the child’s physical and emotional needs); 3) supervision (monitoring of the child’s movements); 4) discipline (enforcement of rules and punishments); 5) discord (arguments, tension, or violence among family members); 6) physical abuse (violence directed toward the child by parents); 7) sexual abuse (nonconsensual sexual contact directed toward the child by any perpetrator); and 8) psychological abuse (humiliation, extreme rejection, or exploitation of the child).
Following the interview, expert judges who were blind to participants’ subtype diagnosis assigned ratings to the aforementioned scales on the basis of standardized criteria (1). The supervision and discipline scales were rated on a 3-point scale (1=high, 2=moderate, 3=lax). Moderate levels of these variables are normative (i.e., not associated with depression onset) (1). Antipathy, neglect, and discord were rated on a 4-point threat scale (1=marked, 2=moderate, 3=some, 4=little/none). Overall levels of these variables across all parent figures were used in the analyses. The abuse variables were rated as 0 (absent) and 1 (definitely present). Among those with abuse, the incidents were rated on a 4-point threat scale (1=marked, 2=moderate, 3=some, 4=little). For those with multiple abuse perpetrators, peak threat levels were used in the analyses.
The Childhood Experience of Care and Abuse interview has a number of advantages over self-report questionnaires of childhood adversity (1). Most important is that it addresses depressive biases that can cloud retrospective recollections of childhood experience, since participants are interviewed about the context of their childhood experience and are encouraged to support their impressions with behavioral examples (14). For instance, a participant’s statement, “I think my mother hated me,” is only taken as an indicator of antipathy if it is supported by clear behavioral evidence (e.g., “She told me everyday that she wished she’d never had me”). Prior studies that used the Childhood Experience of Care and Abuse found that this measure had a high degree of reliability and validity in the assessment of childhood adversity (e.g., interrater reliability kappa estimates ranged from 0.78 to 1.00) (1). In the present study, two judges rated 12% of the group and reported 100% agreement on the parental care scales and 82% agreement on the abuse scales (kappa=0.60). All discrepancies between raters were resolved by consensus.
Results
Preliminary Analyses
In order to identify covariates to be included in the primary analyses, preliminary chi-square tests and independent-sample t tests were performed to examine the basic associations of the diagnostic groups and the adversity variables with age, marital status, education, occupation, number of previous episodes, and treatment status. Only the relationship between age and sexual abuse was significant: subjects with a history of sexual abuse were significantly younger (mean=33.95, SD=10.04) than those without such a history (mean=41.03, SD=11.20) (t=2.90, df=74, p<0.005). Results of the primary analyses including age as a covariate did not differ from the uncontrolled analyses, so only the uncontrolled results are presented.
On the Hamilton depression scale, those with endogenous depression scored significantly higher (mean=21.74, SD=4.22) than did those with nonendogenous depression (mean=15.87, SD=4.60) (t=5.66, df=74, p<0.0001). Those with histories of sexual abuse also scored significantly higher on the Hamilton depression scale (mean=20.15, SD=4.49) than did those without such a history (mean=16.17, SD=5.18) (t=3.52, df=74, p<0.01). Finally, Hamilton depression scale scores were related to supervision (F=3.11, df=2, 73, p<0.05). Post hoc tests revealed that those with lax supervision scored significantly higher (mean=19.96, SD=5.23) than did those with moderate supervision (mean=16.66, SD=5.20) (p<0.05).
Primary Analyses: Childhood Adversity and Depression Subtype
The prevalence and severity of the eight adversity variables among the 76 depressed women are presented in Table 2. Additional descriptive characteristics for physical and sexual abuse are as follows. The mean age at onset of sexual abuse was 9.62 years (SD=5.33), and the mean age at onset of physical abuse was 4.12 years (SD=4.62). Fifty-five percent (N=22) of those with sexual abuse experienced only one incident, while the rest experienced abuse ranging in duration from 3 to 207 months (median=30). The mean duration for physical abuse was 118.86 months (SD=59.78). Twenty-eight percent of sexual abuse cases (N=11) were perpetrated by a close relative, 50% (N=20) were perpetrated by a nonrelative or stranger, and 23% (N=9) experienced sexual abuse by multiple perpetrators, both relatives and nonrelatives. Physical abuse was perpetrated by parents in all cases.
Because of low numbers in some cells, and in order to simplify interpretation, three adversity variables (antipathy, neglect, and discord) were collapsed into nonsevere (ratings of some or little) and severe (ratings of moderate or marked) groups. A series of two-tailed two-by-two and two-by-three Pearson chi-square analyses were conducted to test the univariate associations among depression subtype and the adversity variables. Fisher’s exact test of significance was applied to the two-by-two chi-square analyses. The likelihood ratio test was applied to the sexual abuse analysis because of small expected frequencies.
In direct contrast to previous findings, endogenous depression was approximately twice as likely to be diagnosed in those with severe levels of physical abuse (χ2=7.00, df=2, p<0.05), sexual abuse (χ2=5.92, df=2, p<0.05), antipathy (χ2=5.69, df=1, p<0.05), and neglect (χ2=4.68, df=1, p<0.05) than in those with nonsevere adversity. In addition, while the relationship between subtype and discord was not significant, those with marked levels of discord were more than twice as likely to be diagnosed with endogenous depression (65%) than those with moderate (32%), some (33%), or little/no discord (36%). Furthermore, endogenous depression was more than twice as likely to be diagnosed in those with lax and high levels of supervision (χ2=8.40, df=2, p<0.05) and discipline (χ2=7.47, df=2, p<0.05) than in those with moderate levels of these variables.
Multivariate Analyses
In order to examine the relative contributions of the aforementioned significant childhood adversity variables to endogenous versus nonendogenous depression, a forward stepwise logistic regression was performed. A stepwise model was chosen instead of a theoretically driven entry model because we had no a priori hypotheses regarding the relative importance or temporal ordering of childhood adversity variables to the model.
To avoid problems with multicollinearity, two composite variables were created because of the high intercorrelations between antipathy and neglect (r=0.74, df=74, p<0.001) and between supervision and discipline (r=0.54, df=74, p<0.001). The dichotomous composite variable “poor care” denoted the presence or absence of severe antipathy or neglect. The composite variable “control” had three levels: 0=moderate supervision and discipline; 1=high supervision or discipline; 2=lax supervision or discipline. Therefore, the predictors included in the stepwise procedure were physical abuse, sexual abuse, poor care, and control.
As seen in Table 3, the forward stepwise model identified poor care and sexual abuse as significant predictors (χ2=11.62, df=2, p<0.005), with 68% of participants correctly classified to endogenous versus nonendogenous groups. The odds ratios indicated that women with poor care were almost two and a half times as likely to be diagnosed with endogenous depression than those without. Similarly, those with severe sexual abuse were almost twice as likely to be diagnosed with endogenous depression than those without. Physical abuse and control, despite displaying univariate relationships with endogenous depression, were no longer significant when poor care and sexual abuse were included in the model.
Follow-Up Control Analyses: Sexual Abuse and Depression Severity
As noted in the preliminary analyses, sexual abuse was significantly associated with overall depression severity, as assessed by the Hamilton depression scale. This finding is interesting in and of itself but raises the question of whether depression severity alone can account for the strong relationship between sexual abuse and endogenous depression. That is, do those with severe sexual abuse score higher on a broad, uniformly distributed range of depression symptoms, or is sexual abuse associated with higher scores on only those symptoms that make up the supposedly qualitatively distinct syndrome of endogenous depression? The severity confound is challenging to address statistically, since many Hamilton depression scale symptoms are also symptoms of endogenous depression. Therefore, the Hamilton depression scale and the endogenous depression measure are highly collinear, and covarying Hamilton depression scale scores statistically would partial out most of the variance in the endogenous depression measure.
We chose instead to descriptively examine the univariate correlations among severe sexual abuse and the individual Hamilton depression scale symptoms. We found that severe sexual abuse was associated with higher scores on the endogenous symptoms of guilt (r=0.27, df=74, p<0.05) and psychomotor retardation (r=0.27, df=74, p<0.05). The only nonendogenous symptom to significantly discriminate severe versus nonsevere levels of sexual abuse was suicidal ideation (r=0.23, df=74, p<0.05). These results provide further evidence, to be pursued more rigorously in future research, that severe sexual abuse is significantly and preferentially associated with the qualitatively distinct symptoms of endogenous depression.
Discussion
In the present study, severe physical abuse, sexual abuse, antipathy, and neglect, as well as both high and lax levels of supervision and discipline, were significantly associated with endogenous versus nonendogenous depression. Sexual abuse and poor care, a composite of antipathy and neglect, were most strongly associated with endogenous depression in a multivariate model. Sexual abuse was also associated with more severe depression and higher levels of suicidal ideation, consistent with prior research (15–17). Together, these results suggest that severe childhood adversity, particularly sexual abuse, is associated with severe endogenous depression with significant suicidal ideation. This profile is of great concern clinically, since it has been associated with higher rates of relapse and recurrence (5) as well as with risk for more active suicidal intent.
The present results were inconsistent with previous studies that had demonstrated a preferential association between childhood adversity and nonendogenous depression (7, 8). There are a number of potential explanations for this discrepancy. First, previous studies relied on mean Parental Bonding Instrument scores and categorizations of abuse as present or absent (8, 9). By contrast, we examined more fine-grained distinctions in the severity of childhood adversity. We found that while nonsevere levels of childhood adversity were indeed associated with a higher risk of nonendogenous depression, severe childhood adversity was consistently associated with at least double the risk of endogenous depression. Exploiting the richness of the descriptive data provided by the Childhood Experience of Care and Abuse interview, which assigns continuous threat levels, may have allowed this interesting crossover pattern to emerge.
Second, one of the strengths of the study by Parker and colleagues (7) was its use of several diagnostic systems. However, significant associations only emerged when using a “clinical” definition of subtypes, and no differences were found when subtypes were defined according to DSM-IV, Newcastle (18), or CORE (19) criteria. Nonendogenous depression in this “clinical” system was defined, in part, by the presence of “ongoing dysfunctional depressogenic attitudes.” However, a depressogenic cognitive style has been associated with a bias to recall negative information and to magnify the negative aspects of situations (20). Therefore, individuals in Parker et al.’s nonendogenous group were, by definition, more likely to magnify the negative aspects of their childhood experiences. As a result, it is possible that a depressogenic recall bias may account, in part, for the association between childhood adversity and nonendogenous depression in this previous study. This issue is particularly prominent given Parker et al.’s use of the Parental Bonding Instrument, which does not encourage respondents to support their impressions with behavioral evidence and does not probe for potential positive information.
By contrast, a diagnosis of RDC endogenous depression relies on observable depression symptoms as opposed to inferred personality characteristics. However, the RDC have been criticized for being less stringent than other definitions, such as DSM-IV melancholia (21). In the present study, only 10 women met criteria for melancholia, thus precluding multivariate analyses. Nevertheless, when we performed univariate chi-square analyses of the relationship between melancholia and the individual Childhood Experience of Care and Abuse scales, we replicated entirely our results obtained by using RDC endogenous depression, thus further strengthening the present findings.
Since the many diagnostic systems that exist for endogenous depression are each made up of slightly different criteria, each system diagnoses slightly different groups of patients. Such discrepancies in the definition of endogenous depression across studies make comparison of results difficult and limit research investigating the predictive validity of the endogenous depression syndrome. Therefore, we urge researchers in this area to examine the individual symptom profiles of those with different types of childhood adversity. For example, the present results indicate that severe sexual abuse was associated with suicidal ideation along with traditional endogenous symptoms. Future research along these lines may suggest that the criteria for endogenous depression need to be revised for those with childhood adversity.
Finally, the present study group included women only. While Parker and colleagues (7) did not report any sex differences in the relationship between childhood adversity and depression subtype in their patient group, this is still an important methodological difference between the two reports that may help to account for the discrepant findings. It is of interest that the relationship of sexual abuse to severe depression in the present study is consistent with the findings of Gladstone et al. (10), who also used a female patient group. To our knowledge, there have been no systematic attempts to chart sex differences in the relationship of childhood adversity to endogenous versus nonendogenous depression, and we suggest this as an area of future research.
Future studies are required to elucidate potential mediators or moderators of the relationship between childhood adversity and endogenous depression. For example, one might wonder how recent stressful life events or depression recurrence contribute to this model. In preliminary analyses not included in the present results, we examined life events with the Life Events and Difficulties Schedule (22), a rigorous contextual interview and rating system. Neither “severe” events (i.e., events rated as marked or moderate on a 4-point index of threat and believed to be most etiologically central in depression) nor total number of events of any threat level were related to depression subtype. This was the case when recent events were examined as mediators, moderators, or as independent predictors of subtype. In addition, we did not find evidence for an association between childhood adversity and first-onset versus recurrent depression, nor did depression recurrence mediate or moderate the relationship between childhood adversity and depression subtype. Speculation regarding the reasons for these null results is outside of the main focus of the present study, and we urge researchers to pursue these associations more directly.
Endogenous depression has traditionally been associated with a neurobiological etiology, and it is compelling to find it here preceded by severe environmental adversity. However, a large body of research suggests that severe, prolonged, and uncontrollable stress, such as that inherent in severe sexual abuse and poor parental care, has enduring effects on developing brain networks (23–25). Furthermore, prolonged and uncontrollable stress has been proposed as an animal model of anhedonia, provoking behavioral signs analogous to the symptoms of endogenous depression (26). While the present results clearly require replication before undertaking detailed investigations into mediating mechanisms, one intriguing possibility is that severe childhood adversity may have neuropathological consequences that mediate the development of endogenous depression in adulthood. Additional and complementary mediating mechanisms are also possible, and multivariate models are needed to examine the respective contributions of many different variables (e.g., family history, childhood adversity, recent life events, and neuropathological mechanisms) to the development of endogenous versus nonendogenous depression.
As with all retrospective studies, biases are possible in the recall of childhood experiences, especially since all participants were currently depressed. The Childhood Experience of Care and Abuse interview addresses this concern in a more rigorous fashion than that provided by self-report questionnaires, since respondents are probed during the interview about potentially neglected positive information. Furthermore, ratings of childhood adversity are made by judges who are blind to diagnostic subtype. Another limitation of the present design is that it was based on a community group of women, and, therefore, results may not generalize to men or to patient groups. Nevertheless, Hamilton depression scale scores of the present participants were comparable to those reported in most outpatient study groups in the literature. In addition, more than half of the study group was currently receiving outpatient treatment in the community, and no differences were noted on any study variables between this subgroup and those not receiving treatment.
The present study was also limited by its cross-sectional design, which precluded analysis of the relationship between childhood adversity and endogenous depression across repeated episodes. In particular, controversy exists regarding whether endogenous depression is a stable syndrome that expresses itself similarly across recurrent episodes (27, 28) or whether the phenomenology of depression changes across episodes (29). Future research investigating the relationship of childhood adversity to the phenomenology of depression across the lifetime course of the disorder is necessary to help resolve this issue.
In summary, severe levels of childhood adversity were significantly associated with severe endogenous depression. These results may enlarge thinking about the traditional etiological distinction between endogenous and nonendogenous depression and are consistent with emerging research outlining the neuropathological consequences of childhood adversity. Such a symptom profile is of great concern clinically, since it is associated with higher rates of relapse and recurrence (5). Therefore, we suggest that individuals with severe abuse and poor parental care be identified early through regular clinical assessment for childhood adversity and targeted for rigorous acute and maintenance interventions.
 |
 |
 |
Received Oct. 6, 2000; revisions received March 13 and July 20, 2001; accepted Aug. 15, 2001. From the Department of Psychology, University of Oregon. Address reprint requests to Dr. Harkness, Department of Psychology, Queen’s University, Kingston, ONT K7L 3N6, Canada; [email protected] (e-mail). Supported by a grant from the Center for the Study of Women in Society, University of Oregon. The authors thank Burt Sorkey and David Markley for conducting the clinical interviews and ratings, Leela Sears and Meghan Fallenstein for data management, and Drs. Anne Simons, Richard Zinbarg, Marie Harvey, Ellen Frank, Stefanie Hlastala, and Mark Sabbagh for providing comments on earlier versions of this article.
1. Bifulco A, Brown GW, Harris TO: Childhood Experience of Care and Abuse (CECA): a retrospective interview measure. J Child Psychol Psychiatry 1994; 35:1419-1435Crossref, Medline, Google Scholar
2. Bifulco AT, Brown GW, Moran P, Ball C, Campbell C: Predicting depression in women: the role of past and present vulnerability. Psychol Med 1998; 28:39-50Crossref, Medline, Google Scholar
3. Brown GW, Harris TO: Aetiology of anxiety and depressive disorders in an inner-city population, 1: early adversity. Psychol Med 1993; 23:143-154Crossref, Medline, Google Scholar
4. Kraepelin E: Manic-Depressive Insanity and Paranoia. Translated by Barclay RM, edited by Robertson GM. Edinburgh, E & S Livingstone, 1921Google Scholar
5. Rush AJ, Weissenburger JE: Melancholic symptom features and DSM-IV. Am J Psychiatry 1994; 151:489-498Link, Google Scholar
6. Mazure CM: Life stressors as risk factors in depression. Clin Psychol Sci and Practice 1998; 5:291-313Crossref, Google Scholar
7. Parker G, Gladstone G, Wilhelm K, Mitchell P, Hadzi-Pavlovic D, Austin M-P: Dysfunctional parenting: over-representation in non-melancholic depression and capacity of such specificity to refine sub-typing depression measures. Psychiatry Res 1997; 73:57-71Crossref, Medline, Google Scholar
8. Parker G, Kiloh L, Hayward L: Parental representations of neurotic and endogenous depressives. J Affect Disord 1987; 13:75-82Crossref, Medline, Google Scholar
9. Parker G, Tupling H, Brown LB: A parental bonding instrument. Br J Med Psychol 1979; 52:1-10Crossref, Google Scholar
10. Gladstone G, Parker G, Wilhelm K, Mitchell P, Austin MP: Characteristics of depressed patients who report childhood sexual abuse. Am J Psychiatry 1999; 156:431-437; correction, 156:812Abstract, Google Scholar
11. First MB, Spitzer RL, Gibbon M, Williams JBW: Structured Clinical Interview for DSM-IV Axis I Disorders (SCID). New York, New York State Psychiatric Institute, Biometrics Research, 1995Google Scholar
12. Spitzer RL, Endicott J, Robins E: Research Diagnostic Criteria: rationale and reliability. Arch Gen Psychiatry 1978; 35:773-782Crossref, Medline, Google Scholar
13. Hamilton M: A rating scale for depression. J Neurol Neurosurg Psychiatry 1960; 23:56-62Crossref, Medline, Google Scholar
14. Brewin CR, Andrews B, Gotlib IH: Psychopathology and early experience: a reappraisal of retrospective reports. Psychol Bull 1993; 113:82-98Crossref, Medline, Google Scholar
15. Margo GM, McLees EM: Further evidence for the significance of a childhood abuse history in psychiatric inpatients. Compr Psychiatry 1991; 32:362-366Crossref, Medline, Google Scholar
16. Surrey J, Swett C, Michaels A, Levin S: Reported history of physical and sexual abuse and severity of symptomatology in women psychiatric outpatients. Am J Orthopsychiatry 1990; 60:412-417Crossref, Medline, Google Scholar
17. Santa Mina EE, Gallop RM: Childhood sexual and physical abuse and adult self-harm and suicidal behaviour: a literature review. Can J Psychiatry 1988; 43:793-800Google Scholar
18. Carney MWP, Roth M, Garside RF: The diagnosis of depressive syndromes and the prediction of ECT response. Br J Psychiatry 1965; 111:659-674Crossref, Medline, Google Scholar
19. Parker G, Hadzi-Pavlovic D, Wilhelm K, Hickie I, Brodaty H, Boyce P, Mitchell P, Eyers K: Defining melancholia: properties of a refined sign-based measure. Br J Psychiatry 1994; 164:316-326Crossref, Medline, Google Scholar
20. Kovacs M, Beck AT: Maladaptive cognitive structures in depression. Am J Psychiatry 1978; 135:525-533Link, Google Scholar
21. Zimmerman M, Coryell W, Pfohl B: The validity of four definitions of endogenous depression. Arch Gen Psychiatry 1986; 43:234-244Crossref, Medline, Google Scholar
22. Brown GW, Harris TO: Social Origins of Depression: A Study of Psychiatric Disorder in Women. New York, Free Press, 1978Google Scholar
23. Sapolsky R: Why stress is bad for your brain. Science 1996; 273:749-750Crossref, Medline, Google Scholar
24. Ladd CO, Owens MJ, Nemeroff CB: Persistent changes in corticotropin-releasing factor neuronal systems induced by maternal deprivation. Endocrinology 1996; 137:1212-1218Crossref, Medline, Google Scholar
25. Bremner JD, Randall P, Vermetten E, Staib L, Bronen RA, Mazure C, Capelli S, McCarthy G, Innis RB, Charney DS: Magnetic resonance imaging-based measurement of hippocampal volume in posttraumatic stress disorder related to childhood physical and sexual abuse: a preliminary report. Biol Psychiatry 1997; 41:23-32Crossref, Medline, Google Scholar
26. Willner P: Animal models of depression: validity and applications. Adv Biochem Psychopharmacol 1995; 49:19-41Medline, Google Scholar
27. Coryell W, Winokur G, Shea T, Maser JD, Endicott J, Akiskal HS: The long-term stability of depressive subtypes. Am J Psychiatry 1994; 151:199-204Link, Google Scholar
28. Paykel ES, Prusoff BA, Tanner J: Temporal stability of symptom patterns in depression. Br J Psychiatry 1976; 128:369-374Crossref, Medline, Google Scholar
29. Young MA, Keller MB, Lavori PW, Scheftner WA, Fawcett JA, Endicott J, Hirschfeld RMA: Lack of stability of the RDC endogenous subtype in consecutive episodes of major depression. J Affect Disord 1987; 12:139-143Crossref, Medline, Google Scholar



