The Role of Childhood Interpersonal Trauma in Depersonalization Disorder
Abstract
OBJECTIVE: In contrast to trauma’s relationship with the other dissociative disorders, the relationship of trauma to depersonalization disorder is unknown. The purpose of this study was to systematically investigate the role of childhood interpersonal trauma in depersonalization disorder. METHOD: Forty-nine subjects with DSM-IV depersonalization disorder and 26 healthy comparison subjects who were free of lifetime axis I and II disorders and of comparable age and gender were administered the Dissociative Experiences Scale and the Childhood Trauma Interview, which measures separation or loss, physical neglect, emotional abuse, physical abuse, witnessing of violence, and sexual abuse. RESULTS: Childhood interpersonal trauma as a whole was highly predictive of both a diagnosis of depersonalization disorder and of scores denoting dissociation, pathological dissociation, and depersonalization. Emotional abuse, both in total score and in maximum severity, emerged as the most significant predictor both of a diagnosis of depersonalization disorder and of scores denoting depersonalization but not of general dissociation scores, which were better predicted by combined emotional and sexual abuse. The majority of the perpetrators of emotional abuse were either or both parents. Although different types of trauma were modestly correlated, only a few of these relationships were statistically significant, underscoring the importance of comprehensively considering different types of trauma in research studies. CONCLUSIONS: Childhood interpersonal trauma and, in particular, emotional abuse may play a role in the pathogenesis of depersonalization disorder. Compared to other types of childhood trauma, emotional maltreatment is a relatively neglected entity in psychiatric research and merits more attention.
Dissociation is the disruption of the normal integrative processes of consciousness, perception, memory, and identity that define self-hood. All dissociative disorders currently classified in DSM-IV are characterized by pathological dissociation but differ in the dissociative domains in which symptoms are primarily manifested. Research has revealed that pathological dissociation is a categorically distinct entity from the normal dissociative tendencies that characterize the general population (1), and in a well-designed twin study (2), the genetic heritability estimate for pathological dissociation was zero, suggesting that these conditions may be strongly driven by environmental traumas. It appears that traumatic antecedents play a major role in the pathogenesis of various dissociative disorders, although the age, type, and severity of the traumas involved differs. Putnam and Trickett (3) eloquently described the shifts in self-states and the fragmentation of self and behavior that characterize victims of child abuse. In a review article (4), 26 studies involving 2,108 subjects were compiled exploring the relationship between abuse and dissociation; in this meta-analysis, the effect size of this association was highly significant and independent of the type of abuse.
When examined by individual disorder, the role of trauma can be briefly summarized as follows. Several studies (5, 6) have clearly documented the relationship between childhood interpersonal trauma, in particular, severe physical and/or sexual abuse, and dissociative identity disorder. In dissociative amnesia, an acute precipitating traumatic event is commonly identified, and in dissociative fugue, subacute chronic stress is typically described. In the more culturally bound dissociative disorders, such as ataque and possession or trance states, traumatic stressors are also typically described (7). Even in subjects who do not suffer from a dissociative disorder, dissociative symptoms are strongly suggestive of traumatic histories. In a study of subjects with borderline personality disorder (8), derealization was the single best predictor of childhood sexual abuse. Another study of general psychiatric inpatients (9) found that childhood trauma was more strongly related to dissociation than to posttraumatic stress disorder (PTSD). Dissociation is one of the core symptoms of the newly proposed DSM-IV criterion for acute stress disorder, and it appears predictive both of later PTSD (10) and later dissociation (11).
Given the well-documented traumatic antecedents to a variety of dissociative symptoms and disorders, we were interested in determining the possible role of trauma in the pathogenesis of depersonalization disorder, one of the major DSM-IV dissociative disorders, in which traumatic antecedents have been minimally elucidated. In a preliminary study of childhood trauma in depersonalization disorder (12), subjects were found to be significantly more traumatized than healthy comparison subjects. However, the trauma interview employed in that study had important limitations. It only categorically quantified as present or absent just three types of trauma—physical abuse, sexual abuse, and witnessing of domestic violence—during three developmental periods. It did not measure dimensions such as severity, frequency, or duration nor other types of childhood trauma, such as emotional abuse, separation or loss, and neglect. Thus, our prior positive findings led us to undertake a more elaborate trauma study in a larger group, which is the subject of this report.
Method
Forty-nine subjects with DSM-IV depersonalization disorder and 26 healthy comparison subjects were recruited. Most subjects with depersonalization disorder were participating in a pharmacological treatment study, and a minority in neurochemical challenge studies. The healthy comparison subjects were participating in studies of neuropsychology or neurochemical challenges. After a complete explanation of the study, written informed consent was obtained from all subjects. All studies had a similar baseline evaluation that included the diagnostic and trauma assessments described next, along with numerous other questionnaires not included in this report. The overall evaluation procedure was described on the written informed consent form as follows: “You will be administered some psychiatric questionnaires and ratings which are designed to determine your current and past feelings, behavior and life circumstances. These initial questionnaires may take up to 6 hours to complete.” Trauma was not a focus in these studies, thus minimizing potential subject bias in the reporting of childhood trauma and effectively serving as a blind. The subjects were also not recruited from or evaluated within the context of any specialized trauma treatment unit or therapy that may have increased subject bias. The investigators were not blind to subject diagnoses. However, as will be described, trauma scoring criteria were highly detailed and quantifiable, thus decreasing potential interviewer biases. The subjects with depersonalization disorder were recruited mostly through newspaper advertisements for research (“Do you frequently feel unreal/detached, as if in a dream/fog?”) and occasionally by means of direct clinician referrals. The healthy comparison subjects were also recruited through advertisements (“no lifetime psychiatric problems”). After a telephone screening, subjects who were potentially appropriate were seen for an initial clinical evaluation. This initial evaluation was always conducted by the principal investigator (D.S.), most often in conjunction with a co-investigator (O.G.). It lasted up to 1 hour, and it comprised a general psychiatric history with an emphasis on dissociative symptoms, treatment history, and an overview of the major inclusion or exclusion criteria with regard to study participation; trauma histories were not elicited.
Clinical diagnoses were subsequently confirmed by the following structured diagnostic interviews. The subjects were evaluated by means of the Structured Clinical Interview for DSM-IV Dissociative Disorders (13), which allows the diagnosis of DSM-IV dissociative disorders with a kappa of 0.96. The healthy comparison subjects were free of dissociative disorders, other lifetime axis I disorders, as assessed by means of the Structured Clinical Interview for DSM-IV Axis I Disorders (14), and axis II disorders, as assessed by means of the Structured Interview for DSM-IV Personality Disorders (15).
The subjects completed the Dissociative Experiences Scale (16, 17), which is by far the most widely employed scale measuring dissociation, used in more than 250 research studies to date (18). The Dissociative Experiences Scale is a 28-item self-report measure of dissociative experiences that is intended for use as a trait measure and inquires about “experiences that you may have in your daily life.” Items are marked on a 0–100-mm visual analog scale and are scored to the nearest 5 mm. The total score on the Dissociative Experiences Scale is the mean score on the 28 items and ranges from 0 to 100. The Dissociative Experiences Scale has been shown to have good test-retest reliability (intraclass correlation coefficent=0.79–0.96), high internal consistency (Cronbach’s alpha=0.95), and strong convergent, discriminant, and criterion validity (17).
Although some debate exists in the literature regarding the validity of factor analyses of the Dissociative Experiences Scale, which yield dissociative symptom subscales and scores that can be used in research, numerous studies have similarly replicated three factors: self-absorption, amnesia, and depersonalization (17). A factor analysis of subjects with depersonalization disorder confirmed these three factors (19). In the current study we employed a depersonalization score from the Dissociative Experiences Scale based on that factor analysis (the mean of items 7, 12, 13, 24, and 28). In addition, in this study we employed the pathological dissociation taxon score from the Dissociative Experiences Scale that was proposed by Waller et al. (1). They reexamined the structure of the Dissociative Experiences Scale with sophisticated taxometric analyses and found that it encompasses two categorically distinct entities: normal dissociation, which is widely distributed in the general population and pathological dissociation, which is relatively rare in the population and a clear indication of pathology. The taxon includes Dissociative Experiences Scale items 3, 5, 7, 8, 12, 13, 22, and 27. We have previously found that this taxon score, when applied to subjects with depersonalization disorder, reflects their pathological dissociative state much more strongly than their relatively modest scores on the Dissociative Experiences Scale (19).
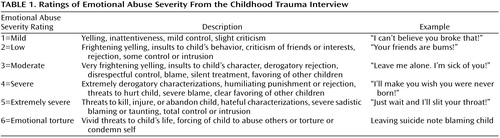
The Childhood Trauma Interview (20) is a detailed clinician-administered interview of childhood interpersonal trauma up to age 18, which has been described as “unique in providing a means of quantifying the frequency, severity, and duration of a wide range of childhood interpersonal traumatic events” (18). It has been shown to have high reliability and validity and inquires in detail about six types of trauma (separation or loss, physical neglect, emotional abuse, physical abuse, witnessing of violence, and sexual abuse) and codes age range, duration, frequency, severity, and perpetrator types. Duration is scored in years (range=0–18), while severity and frequency are scored on a scale of 0–6. A frequency score of 1 represents “once or a few times over a number of years,” and a score of 6 “daily or more than once a day.” Severity can range from very mild to extreme, customized to each type of trauma and described with many detailed examples in the scoring manual. Table 1 summarizes the severity coding for emotional abuse from the Childhood Trauma Interview.
Total scores for each type of trauma were calculated by multiplying duration by frequency by severity for each perpetrator (range=0–648) and summed across all perpetrators in the particular category. The total trauma score is the sum of total scores for the six types of trauma. Maximum severity for each type of trauma is defined as the highest severity score of all traumatic incidents in that category (range=0–6). We examined severity separately, in addition to total trauma scores, because severity of traumatic events is considered a major variable with pathogenic implications in the trauma literature (18). It is conceivable, for example, that a frequent and chronic low-grade trauma could yield, by means of the scoring of this instrument, a greater total trauma score than that for a one-time very severe trauma. Investigators (D.S. and O.G.) were fully trained in the administration and scoring of the Childhood Trauma Interview under the guidance of its developer, Laura Fink, Ph.D.
All between-group comparisons of types of trauma employed Student’s t tests that were Bonferroni corrected for six comparisons. Student’s t tests were also used to compare dissociation scores between the two groups. Logistic regression analyses were used to predict diagnostic group by trauma scores, while multiple regression analyses were used to predict dissociation scores by trauma scores. All stepwise regressions were conservatively corrected for the number of predictors by means of an adaptation of the Scheffé procedure for multiple comparisons. For logistic regressions, this meant simply testing the chi-square value by using the degrees of freedom for all predictors. For multiple regressions, the sum of squares for any set of predictors was tested by using the degrees of freedom for all the predictors. Pearson’s correlations were employed to examine the relationships between the six different types of trauma and were Bonferroni corrected for 15 comparisons. All tests were two-tailed.
Results
The two groups did not differ in age (subjects with depersonalization disorder, mean=33.84 years, SD=8.74; healthy comparison subjects, mean=30.50 years, SD=9.57) (t=1.52, df=73, n.s.) or gender (χ2=1.88, df=1, n.s.). The mean age of illness onset in the group with depersonalization disorder was 16.14 years (SD=7.62, range=3–41). All scores on the Dissociative Experiences Scale were significantly higher in the group with depersonalization disorder than in the comparison subjects (total score, mean=24.43, SD=13.57, versus mean=4.55, SD=3.51, respectively) (t=7.32, df=73, p<0.001) (depersonalization score, mean=46.73, SD=20.44, versus mean=2.70, SD=3.11) (t=10.88, df=73, p<0.001) (pathological dissociation taxon score, mean=24.97, SD=12.04, versus mean=1.45, SD=2.72) (t=9.80, df=73, p<0.001).
Current axis I comorbidity in the group with depersonalization disorder was the following: one with bipolar disorder, six with major depression, 10 with dysthymia, six with panic disorder, nine with social phobia, four with obsessive-compulsive disorder, seven with generalized anxiety disorder, two with PTSD, one with bulimia, four with somatization, two with body dysmorphic disorder, and three with adjustment disorder. Axis II comorbidity in the group with depersonalization disorder consisted of the following personality disorders: avoidant (N=13), dependent (N=4), obsessive-compulsive (N=10), paranoid (N=6), schizoid (N=0), schizotypal (N=1), antisocial (N=1), borderline (N=9), histrionic (N=4), and narcissistic (N=7).
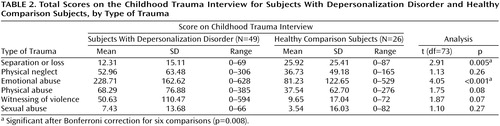
Total scores for each of the six types of trauma differed between the two groups for separation or loss and emotional abuse (Table 2). It is of interest that separation or loss was greater in the healthy subjects, whereas emotional abuse was greater in the subjects with depersonalization disorder. The total trauma score was significantly higher in the group with depersonalization disorder than in the comparison subjects (mean=420.29, SD=295.27, versus mean=194.62, SD=179.94, respectively) (t=3.56, df=73, p=0.001). The vast majority of the perpetrators of emotional abuse were parents: both parents for 23 subjects with depersonalization disorder, the mother only for 12, and the father only for nine. The reported incidence of other perpetrators, such as siblings, other relatives, other adult caregivers or acquaintances, and peer groups, was notably lower, with frequencies of eight or fewer for the group with depersonalization disorder.
The six total trauma scores together significantly predicted diagnostic group by logistic regression (χ2=27.55, df=6, p<0.001), correctly classifying 77% of all subjects and 90% of the subjects with depersonalization disorder. When entered stepwise into the logistic regression, emotional abuse alone significantly predicted diagnosis (χ2=17.95, df=6, p<0.01). Emotional abuse and separation or loss together also predicted diagnosis more powerfully than emotional abuse alone (χ2=24.77, df=6, p<0.001), whereas the improvement to the emotional abuse prediction contributed by separation or loss did not approach significance (χ2=6.82, df=6, n.s.).
In addition, we examined the prediction of dissociation scores by total trauma scores by means of multiple regressions. As a unit, the six total trauma scores significantly predicted the total score on the Dissociative Experiences Scale (R=0.42, R2=0.18; F=2.41, df=6, 68, p<0.05), the pathological dissociation taxon score (R=0.42, R2=0.18; F=2.46, df=6, 68, p<0.05), and especially the depersonalization score (R=0.50, R2=0.25; F=3.81, df=6, 68, p=0.002). When entered stepwise into the multiple regression analyses, emotional abuse alone significantly predicted the depersonalization score (R=0.41, R2=0.17; corrected F=2.51, df=6, 68, p<0.05) but not the total or taxon scores. No other types of trauma yielded significant predictions.
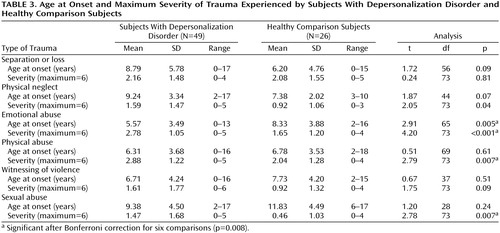
The two groups did not differ significantly in the age at onset for any type of trauma other than emotional abuse, which had an earlier onset in the subjects with depersonalization disorder (Table 3). Maximum severity for each type of trauma was significantly greater in the subjects with depersonalization disorder for emotional, physical, and sexual abuse (Table 3). As a unit, the six maximum severity trauma scores significantly predicted diagnostic group by means of logistic regression (χ2=25.23, df=6, p<0.001), correctly classifying 76% of the subjects. When entered stepwise into the logistic regression, the maximum severity of emotional abuse alone significantly predicted diagnosis (χ2=15.23, df=6, p<0.05). Emotional abuse severity and sexual abuse severity together predicted diagnosis more powerfully than emotional abuse severity alone (χ2=22.75, df=6, p<0.001), whereas the improvement to the prediction by emotional abuse severity contributed by sexual abuse severity did not approach significance (χ2=7.52, df=6, n.s.).
In addition, we examined the prediction of dissociation scores by maximum severity for each type of trauma using multiple regression analyses. The six trauma scores for maximum severity together significantly predicted total score on the Dissociative Experiences Scale (R=0.52, R2=0.27; F=4.21, df=6, 68, p=0.001), the pathological dissociation taxon score (R=0.48, R2=23; F=3.41, df=6, 68, p<0.01), and the depersonalization score (R=0.51, R2=0.26; F=4.01, df=6, 68, p=0.002). When entered stepwise into the multiple regression analyses, maximum severity of emotional abuse and sexual abuse combined significantly predicted total score on the Dissociative Experiences Scale (R=0.46, R2=0.21; corrected F=3.28, df=6, 68, p<0.01). Maximum severity of emotional abuse alone significantly predicted only depersonalization score (R=0.44, R2=0.19; corrected F=2.91, df=6, 68, p<0.05).
When we examined the relationships between total scores for each type of trauma, Bonferroni corrected for 15 comparisons to p=0.003, the only significant correlations were between emotional abuse and physical abuse (r=0.35, df=73, p=0.002), as well as between witnessing of violence and physical abuse (r=0.52, df=73, p<0.001). Relationships among maximum severity ratings for each type of trauma, with the same statistical correction, revealed a significant correlation only between the maximum severity of emotional abuse and physical abuse (r=0.46, df=73, p<0.001).
Discussion
The main findings of this study can be summarized as follows: childhood interpersonal trauma as a whole was highly predictive of both a diagnosis of depersonalization disorder and of scores denoting dissociation, pathological dissociation, and depersonalization. When we examined the role of the various types of trauma with conservative statistical methods, emotional abuse alone, both total score and maximum severity, emerged as the most significant predictor of both depersonalization disorder diagnosis and depersonalization severity. The large majority of perpetrators in the category of emotional abuse were either or both parents. It appears, then, that the ongoing chronicity and frequency of abuse, which presumably reflect the predominant affective coloring of the underlying attachment between parent and child and are captured by the total score, the worst form that the emotional abuse ever took as encoded by its maximum severity, and its earlier age at onset, may all play an important role in the pathogenesis of depersonalization disorder. It is of interest that separation or loss appeared protective; one might speculate that their greater occurrence in healthy subjects yielded them protection from otherwise potentially abusive individuals. It is also intriguing that emotional abuse significantly predicted depersonalization disorder but not general scores denoting dissociation, which were better predicted by the combined severity of emotional and sexual abuse. This suggests a unique relationship between emotional abuse and depersonalization disorder, while other more severe types or combinations of abuse may contribute to more severe dissociative symptoms, such as amnesia or identity disturbances.
The results clearly indicate that although different types of trauma tended to be modestly correlated, a limited number of these relationships were statistically significant, underscoring the importance of considering different types of trauma as independent entities as well as in conjunction with each other in their cumulative impact. This variation highlights the importance of comprehensively assessing the various types of childhood trauma in research. Concerns can arise when studies of particular types of abuse fail to control for other covarying types of abuse (21, 22). For example, concomitant physical or psychological abuse may account for some of the difficulties otherwise attributed to sexual abuse (23), whereas emotional maltreatment is present in almost all cases of physical maltreatment and may be more strongly related to detrimental outcomes (24–27).
There is a notable paucity of research on emotional maltreatment compared to physical or sexual abuse, which is probably contributed to by a number of factors. For one, emotional maltreatment can certainly be less dramatic and toxic than more severe types of abuse. Second, it is almost ubiquitous, and therefore its definition, operationalization, and measurement pose particular challenges (28). A variety of terms have been used to describe it, such as emotional abuse, psychological abuse, psychological maltreatment, mental injury, mental cruelty, and emotional neglect, which capture similar but not necessarily identical concepts (29). Five subcategories have been delineated by experts in the field: rejection and degradation, terror, exploitation and corruption, denial of emotional responsiveness, and isolation (30).
Even so, a number of studies have underscored the potential importance of emotional maltreatment. Parental warmth in early life is well known to be protective against later psychiatric risk (31), and the presence of emotional abuse, in addition to its direct detriments, has been found to be significantly related to less loving support and promotion of individuation by parents of both genders (32). One study of women with bulimia nervosa (33) found that they differed from healthy comparison women in exposure to emotional and physical abuse and cautioned against focusing simply on sexual abuse. In a nonclinical female sample, disordered eating was predicted only by emotional abuse, and the effect was strongly mediated by anxiety and dissociation (34). In a study of patients with personality disorder and substance abuse (35), emotional abuse was a broad risk factor for all three clusters, whereas no specific associations emerged for sexual abuse.
The relationship between emotional abuse and dissociation in particular has received limited attention. Almost all studies to date have focused on the relationship between sexual and/or physical abuse and dissociation, although there has been growing interest in the pathogenic role of seriously disrupted early attachments (36). Indeed, in a study of dissociation in female college students (37), no single type of abuse accounted for a unique proportion of the variance in dissociation when the other types of abuse were controlled. In adolescent general psychiatric inpatients, dissociation was significantly correlated with emotional abuse, physical abuse, sexual abuse, and neglect (38). In adult general psychiatric inpatients, the severity of dissociative symptoms was best predicted by sexual abuse, physical abuse, and maternal neglect (39). A reported history of childhood psychological maltreatment in the absence of physical or sexual abuse was found to correlate with adult dissociation in female health care providers (40). Dissociation also correlated with negative home environment and neglect, separate from sexual abuse and from punishment, in college students (41).
Certain important limitations of this study should be highlighted. Given the absence of a psychiatric control group, one could argue that the higher rates of emotional abuse in the subjects with depersonalization disorder than in the healthy volunteers was a nonspecific finding that might characterize a variety of psychiatric disorders. However, the very powerful prediction, not just of diagnosis but also of dissociation scores by trauma, and the uniquely specific prediction of depersonalization scores by emotional abuse, mitigated against this possibility. It is well established that scores denoting dissociation, and particularly pathological dissociation, effectively discriminate dissociative diagnoses from other psychiatric diagnoses (1, 17). Still, a future study might benefit from the inclusion of a psychiatric control group, such as one with major depression or measures of other symptom profiles, such as anxiety and depression. Also, our trauma interviews could not be conducted with investigators blind to diagnoses; this may have conceivably skewed our findings. However, the Childhood Trauma Interview is highly operationalized and quantifiable and leaves little room for subjective interpretation, and we did not have a preexisting hypothesis regarding emotional abuse in particular. The trauma interview utilized in this study thoroughly explores certain aspects of emotional abuse, such as spurning and terrorizing, but is more limited in its coverage of emotional neglect, i.e., the absence of positive parenting (42). A larger mixed group of subjects with dissociative disorders might better allow a teasing out of the relationship among the various dissociative disorders and symptoms and the various types of childhood trauma. Finally, any cross-sectional study has to be very cautious in inferences about causality, and ultimately, the genesis and evolution of dissociative symptoms has to become fully elaborated from children subjected to trauma followed prospectively into adulthood.
In conclusion, this study is the first systematic demonstration of an association between depersonalization disorder and childhood interpersonal trauma and suggests that emotional abuse may play an important role in the genesis of depersonalization symptoms. In contrast to physical and sexual abuse, psychological maltreatment appears underestimated and neglected in the psychiatric literature and merits more attention. Finally, the various dissociative disorders may lie on a spectrum of severity associated with different types of childhood traumatic antecedents.
 |
 |
 |
Presented in part at the 16th annual conference of the International Society for the Study of Dissociation, Miami, Nov. 11–13, 1999, and at the 153rd annual meeting of the American Psychiatric Association, Chicago, May 13–18, 2000. Received March 16, 2000; revisions received July 12 and Dec. 4, 2000; accepted Feb. 1, 2001. From the Department of Psychiatry, Mount Sinai School of Medicine, New York. Address reprint requests to Dr. Simeon, Psychiatry Box 1230, Mount Sinai, One Gustave L. Levy Pl., New York NY 10029; [email protected] (e-mail). Funded in part by NIMH grant MH-55582 (to Dr. Simeon). The authors thank Laura Fink, Ph.D., for her guidance and training in the use of the Childhood Trauma Interview.
1. Waller NG, Putnam FW, Carlson EB: Types of dissociation and dissociative types: a taxometric analysis of dissociative experiences. Psychol Methods 1996; 1:300-321Crossref, Google Scholar
2. Waller NG, Ross CA: The prevalence and biometric structure of pathological dissociation in the general population: taxometric and behavior genetic findings. J Abnorm Psychol 1997; 106:499-510Crossref, Medline, Google Scholar
3. Putnam FW, Trickett PK: Child sexual abuse: a model of chronic trauma. Psychiatry 1993; 56:82-95Crossref, Medline, Google Scholar
4. van Ijzendoorn MH, Schuengel C: The measurement of dissociation in normal and clinical populations: meta-analytic validation of the Dissociative Experiences Scale (DES). Clin Psychol Rev 1996; 16:365-382Crossref, Google Scholar
5. Putnam FW, Guroff JJ, Silberman EK, Barban L, Post RM: The clinical phenomenology of multiple personality disorder: review of 100 recent cases. J Clin Psychiatry 1986; 47:285-293Medline, Google Scholar
6. Ross CA, Miller SD, Reagor P, Bjornson L, Fraser GA, Anderson G: Structured interview data on 102 cases of multiple personality disorder from four centers. Am J Psychiatry 1990; 147:596-601Link, Google Scholar
7. Simeon D, Hollander E: Dissociative not otherwise specified, in Comprehensive Textbook of Psychiatry, 7th ed. Edited by Kaplan BJ, Sadock VA. Philadelphia, Lippincott Williams & Wilkins, 2000, pp 1570-1576Google Scholar
8. Ogata SN, Silk KR, Goodrich S, Lohr NE, Westen D, Hill EM: Childhood sexual and physical abuse in adult patients with borderline personality disorder. Am J Psychiatry 1990; 147:1008-1013Google Scholar
9. Chu JA, Dill DL: Dissociative symptoms in relation to childhood physical and sexual abuse. Am J Psychiatry 1990; 147:887-892Link, Google Scholar
10. Marmar CR, Weiss DS, Schlenger WE, Fairbank JA, Jordan BK, Kulka RA, Hough RL: Peritraumatic dissociation and posttraumatic stress in male Vietnam theater veterans. Am J Psychiatry 1994; 151:902-907Link, Google Scholar
11. Bremner JD, Brett E: Trauma-related dissociative states and long-term psychopathology in posttraumatic stress disorder. J Trauma Stress 1997; 10:37-49Medline, Google Scholar
12. Simeon D, Gross S, Guralnik O, Stein DJ, Schmeidler J, Hollander E: Feeling unreal:30 cases of DSM-III-R depersonalization disorder. Am J Psychiatry 1997; 154:1107-1113Google Scholar
13. Steinberg M: Structured Clinical Interview for DSM-IV Dissociative Disorders (SCID-D), Revised. Washington, DC, American Psychiatric Press, 1994Google Scholar
14. First MB, Spitzer RL, Gibbon M, Williams JBW: Structured Clinical Interview for DSM-IV Axis I Disorders, Patient Edition (SCID-P), version 2. New York, New York State Psychiatric Institute, Biometrics Research, 1995Google Scholar
15. Pfohl B, Blum N, Zimmerman M: Structured Interview for DSM-IV Personality: SIDP-IV. Iowa City, University of Iowa, Department of Psychiatry, 1995Google Scholar
16. Bernstein EM, Putnam FW: Development, reliability, and validity of a dissociation scale. J Nerv Ment Dis 1986; 174:727-735Crossref, Medline, Google Scholar
17. Bernstein-Carlson E, Putnam FW: An update on the Dissociative Experiences Scale. Dissociation 1993; 6:16-27Google Scholar
18. Carlson EB: Trauma Assessments: A Clinician’s Guide. New York, Guilford, 1997Google Scholar
19. Simeon D, Guralnik O, Gross S, Stein DJ, Schmeidler J, Hollander E: The detection and measurement of depersonalization disorder. J Nerv Ment Dis 1998; 186:536-542Crossref, Medline, Google Scholar
20. Fink LA, Bernstein D, Handelsman L, Foote J, Lovejoy M: Initial reliability and validity of the Childhood Trauma Interview: a new multidimensional measure of childhood interpersonal trauma. Am J Psychiatry 1995; 152:1329-1335Google Scholar
21. Briere J, Runtz M: Multivariate correlates of childhood psychological and physical maltreatment among university women. Child Abuse Negl 1988; 12:331-341Crossref, Medline, Google Scholar
22. Briere J, Runtz M: Differential adult symptomatology associated with three types of child abuse histories. Child Abuse Negl 1990; 14:357-364Crossref, Medline, Google Scholar
23. Briere J: Methodological issues in the study of sexual abuse effects. J Consult Clin Psychol 1992; 60:196-203Crossref, Medline, Google Scholar
24. Claussen AH, Crittenden PM: Physical and psychological maltreatment: relations among types of maltreatment. Child Abuse Negl 1991; 15:5-18Crossref, Medline, Google Scholar
25. Egeland B, Sroufe LA, Erikson M: The developmental consequences of different patterns of maltreatment. Child Abuse Negl 1983; 7:459-469Crossref, Medline, Google Scholar
26. Ney PG: Does verbal abuse leave deeper scars: a study of children and parents. Can J Psychiatry 1987; 32:371-378Crossref, Medline, Google Scholar
27. Gross AB, Keller HR: Long-term consequences of childhood physical and psychological maltreatment. Aggressive Behavior 1992; 18:171-185Crossref, Google Scholar
28. McGee RA, Wolfe DA: Psychological maltreatment: toward an operational definition. Dev Psychopathol 1991; 3:3-18Crossref, Google Scholar
29. O’Hagan KP: Emotional and psychological abuse: problems of definition. Child Abuse Negl 1995; 19:449-461Crossref, Medline, Google Scholar
30. Hart SN, Brassard MR: Psychological maltreatment: progress achieved. Dev Psychopathol 1991; 3:61-70Crossref, Google Scholar
31. Bowlby J: Developmental psychiatry comes of age. Am J Psychiatry 1988; 145:1-10Link, Google Scholar
32. Nicholas KB, Bieber SL: Parental abusive versus supportive behaviors and their relation to hostility and aggression in young adults. Child Abuse Negl 1996; 20:1195-1211Google Scholar
33. Rorty MR, Yager J, Rossotto E: Childhood sexual, physical, and psychological abuse in bulimia nervosa. Am J Psychiatry 1994; 151:1122-1126Google Scholar
34. Kent A, Waller G, Dagnan D: A greater role of emotional than physical or sexual abuse in predicting disordered eating attitudes: the role of mediating variables. Int J Eat Disord 1999; 25:159-167Crossref, Medline, Google Scholar
35. Bernstein DP, Stein JA, Handelsman L: Predicting personality pathology among adult patients with substance use disorders: effects of childhood maltreatment. Addict Behav 1998; 23:855-868Crossref, Medline, Google Scholar
36. Liotti G: Disorganized/disoriented attachment in the etiology of the dissociative disorders. Dissociation 1992; 5:196-204Google Scholar
37. Sanders DA, Lynn SJ: Dissociative experiences, psychopathology and adjustment, and child and adolescent maltreatment in female college students. J Abnorm Psychol 1992; 18:1-7Google Scholar
38. Sanders B, Giolas MH: Dissociation and childhood trauma in psychologically disturbed adolescents. Am J Psychiatry 1991; 148:50-54Link, Google Scholar
39. Draijer N, Langeland W: Childhood trauma and perceived parental dysfunction in the etiology of dissociative symptoms in psychiatric inpatients. Am J Psychiatry 1999; 156:379-385Abstract, Google Scholar
40. Ferguson KS, Dacey CM: Anxiety, depression and dissociation in women health care providers reporting a history of childhood psychological abuse. Child Abuse Negl 1997; 21:941-952Crossref, Medline, Google Scholar
41. Sanders B, Becker-Lausen E: The measurement of psychological maltreatment: early data on the Child Abuse and Trauma Scale. Child Abuse Negl 1995; 19:315-323Crossref, Medline, Google Scholar
42. Brassard MR, Hart SN, Hardy DB: The psychological maltreatment rating scales. Child Abuse Negl 1993; 17:715-729Crossref, Medline, Google Scholar



