Familiality of the Puerperal Trigger in Bipolar Disorder: Results of a Family Study
Abstract
OBJECTIVE: Puerperal psychosis, an episode of mania or psychosis precipitated by childbirth, follows approximately one in 1,000 deliveries. The evidence of clinical, outcome, and genetic studies supports the hypothesis that the majority of puerperal psychotic episodes are manifestations of an affective disorder diathesis with a puerperal trigger. Family studies of puerperal psychosis consistently demonstrate familial aggregation of psychiatric (particularly affective) disorder and suggest a major overlap in the familial factors predisposing to puerperal psychosis and bipolar disorder. The single large study that used direct interview of relatives suggested that familial factors play a role in vulnerability to puerperal triggering itself. The authors’ goal was to test this hypothesis further. METHOD: They conducted a study of the occurrence of episodes of puerperal psychosis in families multiply affected with bipolar disorder participating in an ongoing molecular genetic study of bipolar disorder in sibling pairs. RESULTS: Episodes of puerperal psychosis followed 81 (26%) of 313 deliveries to 152 parous women with bipolar disorder, 58 (38%) of whom had at least one puerperal psychotic episode. Puerperal episodes clustered in families. Episodes of puerperal psychosis occurred in 74% (N=20) of the 27 parous women with bipolar disorder who had a family history of puerperal psychosis in a first-degree relative but in only 30% (N=38) of the 125 women with bipolar disorder with no such family history. CONCLUSIONS: These results conclusively demonstrate that familial (probably genetic) factors are implicated in susceptibility to triggering of puerperal episodes in women with bipolar disorder. These findings have implications for future research and will be of use clinically in the management of women with bipolar disorder who are considering pregnancy.
Childbirth is a period of rapid and substantial biological, psychological, and social change. It provokes a wide variety of psychiatric disorders, from the brief and common experience of the “baby blues” to some of the most severe episodes of psychotic illness seen in clinical practice. Despite a long history of heated debate, there has been little consensus regarding the nosological status of episodes of psychotic illness in the puerperium. Opinions have varied from those who have argued that puerperal psychosis is a condition in its own right to those who have regarded childbirth as a nonspecific stressor like any other life event, acting to trigger a wide variety of psychotic illness (reviewed in references 1 and 2).
Despite diverse presentations, there is strong evidence from clinical, outcome, and genetic studies of a close relationship between puerperal psychosis and bipolar disorder. The majority of puerperal psychotic episodes are affective, and mania is particularly common in the 2 weeks following childbirth (3–11). Women who have suffered an episode of puerperal psychosis remain at high risk of developing further affective episodes (12), and puerperal episodes of illness follow 20% to 30% of births to women with a history of bipolar disorder or affective psychosis (4, 13, 14).
In a study linking the Danish birth and psychiatric admission registers, Terp and Mortensen (15) obtained the highest relative risk (6.82) for first-episode bipolar manic depressive psychosis 2–28 days following delivery. An even higher figure was obtained when only the first 2 weeks of the puerperium were considered (Terp, personal communication). In contrast, the relative risk for the onset of a schizophrenic episode following delivery was less than 1.
The link between childbirth and episodes of affective illness is further supported by the study of 139 women with bipolar disorder ascertained as part of the National Institute of Mental Health genetics initiative study (16): more than 45% of parous women reported experiencing “severe emotional problems” during pregnancy or within 1 month of childbirth. Surprisingly, however, and in contrast to other studies, no probands in this study reported a manic episode in the puerperium.
Family studies of puerperal psychosis consistently demonstrate familial aggregation of psychiatric (predominantly affective) disorder, with morbidity risks for first-degree relatives in the range 10% to 50% (5, 6, 9, 10, 17–19). The finding of higher rates of affective disorder in relatives of puerperal probands suggests a major overlap in the familial factors predisposing to puerperal psychosis and bipolar disorder but tells us little about whether there is a specific familial component to puerperal triggering.
As part of our ongoing molecular genetic study of bipolar disorder in sibling pairs, we have collected data from female participants regarding puerperal episodes of illness. We use these data here to examine the question of whether the vulnerability to puerperal triggering of episodes aggregates in families multiply affected with bipolar disorder.
Method
Study Group
All women interviewed as part of our molecular genetic study of bipolar disorder in sibling pairs were eligible for inclusion in the study. Families were recruited for the study if at least one member had a lifetime diagnosis of DSM-IV bipolar I disorder and a first-degree relative had a lifetime DSM-IV diagnosis of bipolar, schizoaffective, or recurrent unipolar disorder. Women were recruited on the basis of a personal and family history of affective disorder without regard to a history of puerperal episodes.
After complete description of the study to the subjects, written informed consent was obtained. Probands were interviewed by a trained investigator using either the Schedule for Affective Disorders and Schizophrenia—Lifetime Version (20) or the Schedules for Clinical Assessment in Neuropsychiatry (21), and case note information was obtained. Consensus best-estimate lifetime diagnoses were made on the basis of all available clinical information according to DSM-IV criteria. Detailed information was also collected on the relationship of episodes of illness to childbirth, and, when sufficient information was available, each pregnancy was assessed regarding our criteria for the following: 1) narrowly defined puerperal psychosis (a DSM-IV episode of mania or psychotic episode with onset within 6 weeks of delivery), and 2) broadly defined perinatal episodes (any episode of DSM-IV affective disorder in pregnancy or up to 6 months following delivery).
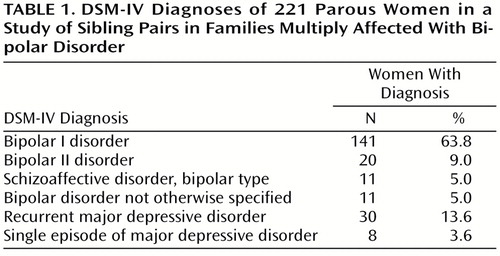
Of 300 women eligible for inclusion in the study, puerperal status could not be assigned to 19 because of lack of information and to 60 women who were nonparous. The DSM-IV diagnoses of the remaining 221 women are listed in Table 1. Two diagnostic groups were used in the analyses: 1) a narrow diagnostic group that included 152 women with a consensus lifetime DSM-IV diagnosis of bipolar I disorder or schizoaffective disorder, bipolar type, and 2) a broad diagnostic group that included 221 women with a consensus lifetime diagnosis of a DSM-IV affective disorder (bipolar I disorder; bipolar II disorder; bipolar disorder not otherwise specified; schizoaffective disorder, bipolar type; recurrent major depressive disorder; or major depressive disorder, single episode).
The occurrence of puerperal psychotic episodes was analyzed in the narrow diagnostic group; these episodes, by definition, could not occur in women with a lifetime diagnosis of a less severe affective disorder. The broad diagnostic group was used to examine the occurrence of perinatal affective episodes more generally, defined as any episode of affective disorder with onset in pregnancy or up to 6 months following delivery.
Statistical Analysis
Two broad approaches were taken to the analysis of the data obtained. First, the concordance for puerperal status between pairs of sisters was assessed by using the kappa statistic. Second, although all of the women, by nature of our inclusion criteria, had a family history of affective disorder, we were also able to distinguish those women with a specific family history of puerperal psychosis by examining the interviews with their female first-degree relatives. The occurrence of puerperal episodes was assessed in those women with bipolar disorder who did or did not have a first-degree relative with puerperal psychosis by using Pearson’s chi-square tests. Both a categorical division of women according to lifetime occurrence of puerperal episodes as well as rates of puerperal psychosis per delivery were analyzed.
Results
For the women with narrowly defined bipolar I disorder and schizoaffective disorder, bipolar type, the mean age at onset of affective illness was 28 years (median=25, SD=11), the mean number of manic episodes was 5.2 (median=4, SD=5.6), and the mean number of depressive episodes was 4.9 (median=4, SD=4.9). Eighty-five (56%) of these women had experienced psychotic symptoms at some stage during their illness.
Occurrence of Perinatal Episodes of Illness
Using the definition of puerperal psychosis already outlined, we found that episodes followed 81 (26%) of 313 deliveries to the 152 parous women in the narrow diagnostic group. Fifty-eight (38%) of the 152 women had experienced at least one episode of puerperal psychosis, 12 (8%) had experienced two episodes, and one (1%) had experienced three. A further 39 (26%) had suffered some other form of perinatal affective episode in pregnancy or within 6 months of delivery. This included four women with a hypomanic episode in the puerperium, 11 with an affective episode in pregnancy, five with a manic episode with onset after 6 weeks, and 19 with an episode of postnatal depression or anxiety. Fifty-five parous women in the narrow diagnostic group (36%) had not suffered any form of perinatal affective episode.
The average numbers of deliveries to women with bipolar disorder with a history of puerperal psychosis (mean=2.07, range=1–5) and deliveries to parous women with bipolar disorder who had no perinatal episodes (mean=2.15, range=1–6) were very similar and did not differ significantly.
Familial Clustering of Puerperal Episodes
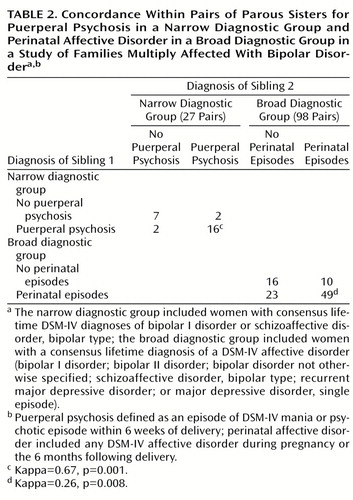
In the narrow diagnostic group, 23 of the 27 pairs of parous sisters were concordant for narrowly defined puerperal psychotic episodes; only four were discordant (Table 2). For the same 27 sibling pairs, there was less marked familial clustering for the wider definition of perinatal episode, including all affective episodes in pregnancy or the puerperium (kappa=0.43, p=0.03). In the broad diagnostic group, 65 of 98 pairs of parous sisters were concordant for the relaxed definition of perinatal episodes (Table 2).
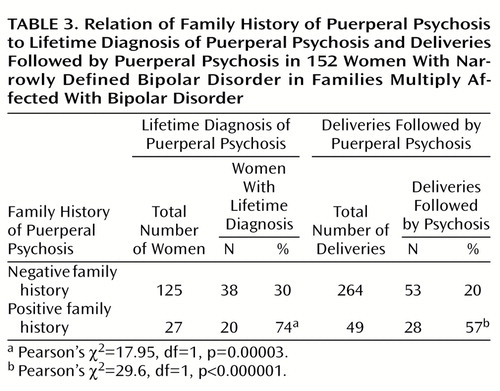
Of the 152 parous women in the group with narrowly defined bipolar disorder, 27 had a first-degree relative with a history of puerperal psychosis. Seventy-four percent of these women had themselves experienced an episode of puerperal psychosis, compared with only 30% of the women with bipolar disorder and no family history of puerperal psychosis (Table 3). Women with bipolar disorder who had a family history of puerperal psychosis were at more than a sixfold greater risk of suffering an episode of puerperal psychosis (odds ratio=6.54, 95% confidence interval [CI]=2.55–16.76) and nearly a fourfold greater risk of suffering any perinatal episode of illness (odds ratio=3.83, 95% CI=1.25–11.74) than parous women with bipolar disorder who had no such family history (Pearson’s χ2=6.14, df=1, p=0.02).
Sixty-nine (31%) of the 221 women in the broad diagnostic group had a first-degree relative with a history of a broadly defined perinatal episode. Fifty-one (74%) of the 69 women had themselves suffered an episode of perinatal affective disorder, compared with 87 (57%) of the 152 women with no such family history (Pearson’s χ2=5.63, df=1, p=0.02). Women with a family history of perinatal episodes were more than twice as likely to suffer an episode of perinatal affective disorder than women with no such family history (odds ratio=2.12, 95% CI=1.54–2.92).
The analysis of the lifetime occurrence of puerperal episodes does not take into account the fact that women differed in the number of episodes of parturition and the periods of risk to which they were exposed. Therefore, we analyzed the data for first pregnancies alone and for each individual pregnancy.
In the narrow diagnostic group, episodes of puerperal psychosis followed 66% (N=18) of first deliveries to women with a family history of puerperal psychosis but only 23% (N=29) of first deliveries to women with no such family history (Pearson’s χ2=15.77, df=1, p=0.00008), a greater than sixfold increase in risk (odds ratio=6.1, 95% CI=2.34–15.97). For all pregnancies, episodes of puerperal psychosis followed 57% of deliveries to women with a family history of puerperal psychosis but only 20% of deliveries to women with no such family history (Table 3) (under the assumption that each pregnancy can be treated as an independent event, odds ratio=5.31, 95% CI=2.80–10.08).
In the broad diagnostic group, an episode of perinatal affective disorder occurred in relationship to 56% (N=40) of first pregnancies in women with a family history of perinatal affective episodes but only 39% (N=40) of first pregnancies in women with no family history of perinatal episodes (odds ratio=2.01, 95% CI=1.09–3.69, Pearson’s χ2=5.09, df=1, p=0.03). For all pregnancies, episodes of perinatal affective disorder were associated with 40% (N=52) of deliveries in women with a family history of perinatal disorder but only 28% (N=95) of deliveries to women with no such family history (under the assumption that each pregnancy can be treated as an independent event, Pearson’s χ2=8.44, df=1, p=0.004, odds ratio=1.75, 95% CI=1.20–2.55).
Discussion
The finding of episodes of puerperal psychosis following 26% of deliveries to women with bipolar I disorder or schizoaffective disorder, bipolar type, is consistent with previous studies that have shown rates of puerperal psychosis of between 20% and 30% in women with bipolar disorder (4, 13, 14). The figure of 260 episodes per 1,000 deliveries is strikingly higher than the approximate population rate of 1 in 1,000 (4) and emphasizes the close relationship between puerperal psychosis and bipolar disorder. Our study further demonstrates that in women with bipolar disorder who had a family history of puerperal psychosis, the rate of puerperal episodes is even higher at 570 per 1,000 deliveries. More than half of the deliveries to women in this group were followed by an episode of mania or psychosis. These rates of illness will be useful in counseling women with bipolar disorder who are considering pregnancy and may inform decisions regarding the use of prophylactic medication in the puerperium.
The results of our study provide compelling evidence, consistent across all methods of analysis employed, that vulnerability to episodes of puerperal psychosis clusters in families multiply affected with bipolar disorder. Moreover, familial aggregation for this most severe form of postnatal illness is greater than for perinatal affective episodes more generally. The finding of familial clustering of puerperal episodes is consistent with the largest family study of puerperal psychosis that used the direct interview of relatives (10). That study employed a narrow definition of puerperal episodes, including only those with onset within 2 weeks of delivery. In contrast to the current study, however, the probands were not selected for a family history of mood disorder, and the puerperal group included women with episodes of major depression in addition to mania and psychosis. Puerperal episodes of illness followed eight (2.2%) of 366 deliveries to female first-degree relatives of 51 patients with only puerperal episodes, but no puerperal episodes were found to have followed 183 deliveries to the relatives of 19 women with bipolar disorder with no history of puerperal illness. For the relatives of 33 women with both puerperal and nonpuerperal illness, two puerperal episodes (1.2%) followed 163 deliveries (nonpuerperal disease versus puerperal psychosis: p=0.05, Fisher’s exact test).
In contrast, Reich and Winokur (14) found no significant loading for postpartum illness in first-degree relatives of bipolar probands with broadly defined puerperal episodes than in bipolar patients more generally. It should be noted, however, that, in their study, numbers were small and perinatal episodes defined very broadly. Only 20 parous women with bipolar disorder were included, and eight of these women had experienced a puerperal episode (any affective disorder with onset within 6 months of delivery).
Limitations
Our study must be interpreted in the light of two important limitations. First, although it demonstrates the familiality of puerperal triggering, it does not, of course, prove that genes are the cause of this resemblance—members of families can be similar because of the effect of shared environment. Given what is known about puerperal psychosis and bipolar disorder, however, genes provide by far the most plausible mechanism for this striking familiality. There is no evidence that the psychosocial context in which a delivery occurs influences the susceptibility to puerperal psychosis (22, 23), and consideration of the abrupt onset at a time of major physiological change convinces most researchers that biological factors are perhaps of fundamental importance. There are no twin or adoption studies of puerperal psychosis, but the importance of genetic factors in etiology is further supported by reports of identical twin pairs concordant for puerperal psychosis (24, 25), and a report of familial clustering of puerperal psychosis associated with close consanguinity raises the possibility of one or more recessive genes contributing to susceptibility (26). When combined with the unequivocal evidence implicating susceptibility genes for bipolar disorder (27), the weight of evidence points to the involvement of genetic factors in puerperal triggering.
Second, our study was based on the direct interview of women from families multiply affected with affective illness recruited as part of our molecular genetic study of bipolar disorder in sibling pairs. However, a systematically ascertained community sample would need to be impractically large to recruit the number of parous female bipolar relative pairs reported here. Moreover, the consistency between the rates of puerperal episodes in this and previous studies provides reassurance that our study group of women with bipolar disorder is representative with regard to puerperal status.
Conclusions
Promising findings are emerging from molecular genetic studies of bipolar disorder, but no genes have been unequivocally identified (27, 28). For complex genetic disorders there are marked benefits in focusing on a homogenous subtype that allows a subset of hypotheses to be tested (29). Molecular genetic studies of puerperal psychosis provide an excellent example of this strategy, allowing a hierarchy of hypotheses concerning the involvement of steroid pathways in pathophysiology to be tested. We recently reported significant evidence (p<0.003) that variation at the serotonin transporter gene exerts a substantial (odds ratio=4) and important (population attributable fraction=69%) influence on susceptibility to bipolar affective puerperal psychosis (30). If replicated, this finding may improve our understanding of the etiological basis of puerperal psychosis. Discovering the basis of the puerperal trigger will lead to major benefits in treatment and prevention of puerperal psychosis and may inform research on a range of other disorders, including menstrual psychosis, premenstrual syndrome, steroid psychosis, and nonpuerperal affective disorders.
 |
 |
 |
Received June 13, 2000; revision received Dec. 11, 2000; accepted Dec. 29, 2000. From the Division of Neuroscience, Department of Psychiatry, University of Birmingham. Address reprint requests to Dr. Jones, Division of Neuroscience, University of Birmingham, Queen Elizabeth Psychiatric Hospital, Birmingham B15 2QZ, U.K.; [email protected] (e-mail). Supported in part by the Wellcome Trust, the South Birmingham Mental Health Trust, and the Women’s Mental Health Trust Charity. The authors thank Prof. Ian Brockington for advice and support and thank the study participants.
1. Brockington IF: Motherhood and mental health, in Puerperal Psychosis. Oxford, UK, Oxford University Press, 1996, pp 200–284Google Scholar
2. Jones I, Lendon C, Coyle N, Robertson E, Brockington N, Craddock N: Molecular genetic approaches to puerperal psychosis. Prog Brain Res (in press)Google Scholar
3. Brockington IF, Cernick KF, Schofield EM, Downing AR, Francis AF, Keelan C: Puerperal psychosis: phenomena and diagnosis. Arch Gen Psychiatry 1981; 38:829–833Crossref, Medline, Google Scholar
4. Kendell RE, Chalmer JC, Platz C: Epidemiology of puerperal psychoses. Br J Psychiatry 1987; 150:662–673Crossref, Medline, Google Scholar
5. Protheroe C: Puerperal psychoses: a long term study 1927–1961. Br J Psychiatry 1969; 15:9–30Crossref, Google Scholar
6. Thuwe I: Genetic factors in puerperal psychosis. Br J Psychiatry 1974; 125:378–385Crossref, Medline, Google Scholar
7. Dean C, Kendell RE: The symptomatology of puerperal illness. Br J Psychiatry 1981; 139:128–133Crossref, Medline, Google Scholar
8. Meltzer ES, Kumar R: Puerperal mental illness: clinical features and classification: a study of 142 mother-and-baby admissions. Br J Psychiatry 1985; 147:647–654Crossref, Medline, Google Scholar
9. Schopf J, Bryois C, Jonquiere M, Scharfetter C: A family hereditary study of post-partum “psychoses.” Eur Arch Psychiatry Neurol Sci 1985; 235:164–170Crossref, Medline, Google Scholar
10. Dean C, Williams RJ, Brockington IF: Is puerperal psychosis the same as bipolar manic-depressive disorder? a family study. Psychol Med 1989; 19:637–647Crossref, Medline, Google Scholar
11. McNeil TF: A prospective study of postpartum psychoses in a high-risk group, I: clinical characteristics of the current postpartum episodes. Acta Psychiatr Scand 1986; 74:205–216Crossref, Medline, Google Scholar
12. Davidson J, Robertson E: A follow-up study of postpartum illness, 1946–1978. Acta Psychiatr Scand 1985; 71:451–457Crossref, Medline, Google Scholar
13. Bratfos O, Haug JO: Puerperal mental disorders in manic depressive females. Acta Psychiatr Scand 1966; 42:285–294Crossref, Medline, Google Scholar
14. Reich T, Winokur G: Postpartum psychoses in patients with manic depressive disease. J Nerv Ment Dis 1970; 151:60–68Crossref, Medline, Google Scholar
15. Terp IM, Mortensen PB: Post-partum psychoses: clinical diagnoses and relative risk of admission after parturition. Br J Psychiatry 1998; 172:521–526Crossref, Medline, Google Scholar
16. Blehar MC, DePaulo JR, Gershon ES, Reich T, Simpson SG, Nurenberger JI: Women with bipolar disorder: findings from the NIMH genetics initiative sample. Psychopharmacol Bull 1998; 34:239–243Medline, Google Scholar
17. Kadramas A, Winokur G, Crow R: Postpartum mania. Br J Psychiatry 1979; 135:551–554Crossref, Medline, Google Scholar
18. Whalley LJ, Roberts DF, Wentzel J, Wright AF: Genetic factors in puerperal affective psychoses. Acta Psychiatr Scand 1982; 65:180–193Crossref, Medline, Google Scholar
19. Platz C, Kendell RE: A matched-control follow-up and family study of “puerperal psychosis.” Br J Psychiatry 1988; 153:90–94Crossref, Medline, Google Scholar
20. Endicott J, Spitzer RL: A diagnostic interview: the Schedule for Affective Disorders and Schizophrenia. Arch Gen Psychiatry 1978; 35:837–844Crossref, Medline, Google Scholar
21. Wing JK, Babor T, Brugha T, Burke J, Cooper JE, Giel R, Jablenski A, Regier D, Sartorius N: SCAN: Schedules for Clinical Assessment in Neuropsychiatry. Arch Gen Psychiatry 1990; 47:589–593Crossref, Medline, Google Scholar
22. McNeil TF: A prospective study of postpartum psychoses in a high-risk group, 3: relationship to mental health characteristics during pregnancy. Acta Psychiatr Scand 1988; 77:604–610Crossref, Medline, Google Scholar
23. Marks MN, Wieck A, Checkley SA, Kumar R: Life stress and postpartum psychosis: a preliminary report. Br J Psychiatry 1991; 158:45–49Crossref, Google Scholar
24. Kane FJ Jr: Postpartum psychosis in identical twins. Psychosomatics 1968; 9:278–281Crossref, Medline, Google Scholar
25. Kallman FJ: The Genetics of Schizophrenia. New York, JJ Augustin, 1938Google Scholar
26. Craddock N, Brockington I, Mant R, Parfitt E, McGuffin P, Owen M: Bipolar affective psychosis associated with consanguinity. Br J Psychiatry 1994; 164:359–364Crossref, Medline, Google Scholar
27. Craddock N, Jones I: Genetics of bipolar disorder. J Med Genet 1999; 36:585–594Crossref, Medline, Google Scholar
28. Risch N, Botstein D: A manic depressive history. Nat Genet 1996; 12:351–353Crossref, Medline, Google Scholar
29. Lander ES, Schork NJ: Genetic dissection of complex traits. Science 1994; 265:2037–2048Google Scholar
30. Coyle N, Jones I, Robertson E, Lendon C, Craddock N: Variation at the serotonin transporter gene influences susceptibility to bipolar affective puerperal psychosis. Lancet 2000; 356:1490–1491Google Scholar



