Cannabis Abuse as a Risk Factor for Depressive Symptoms
Abstract
OBJECTIVE: This study sought to estimate the degree to which cannabis abuse is a risk factor for depressive symptoms rather than an effort to self-medicate depression. METHOD: Participants (N=1,920) in the 1980 Baltimore Epidemiologic Catchment Area (ECA) study who were reassessed between 1994 and 1996 as part of a follow-up study provided the data. The analysis focused on two cohorts: those who reported no depressive symptoms at baseline (N=849) and those with no diagnosis of cannabis abuse at baseline (N=1,837). Symptoms of depression, cannabis abuse, and other psychiatric disorders were assessed with the Diagnostic Interview Schedule. RESULTS: In participants with no baseline depressive symptoms, those with a diagnosis of cannabis abuse at baseline were four times more likely than those with no cannabis abuse diagnosis to have depressive symptoms at the follow-up assessment, after adjusting for age, gender, antisocial symptoms, and other baseline covariates. In particular, these participants were more likely to have experienced suicidal ideation and anhedonia during the follow-up period. Among the participants who had no diagnosis of cannabis abuse at baseline, depressive symptoms at baseline failed to significantly predict cannabis abuse at the follow-up assessment. CONCLUSIONS: Further research is needed to identify characteristics of individuals who abuse cannabis that account for their higher risk of depression to estimate the degree of impairment resulting from their depression.
The comorbid presentation of cannabis abuse and depression is relatively common in clinical and community populations (1, 2). However, the degree to which psychiatric disorders such as depression are predisposing risk factors for substance abuse, or vice versa, is a subject of controversy (3, 4). On the one hand, individuals may use cannabis to self-medicate their dysphoria. On the other hand, chronic cannabis use may exacerbate, if not induce, dysphoria. Policies regarding the medical and legal status of cannabis may be better informed by a more definitive estimation of the risks posed by cannabis abuse, such as whether it is associated with a greater risk of depression.
Anecdotal studies of clinical populations suggest that individuals who abuse cannabis are self-medicating their anxiety and depression (5, 6). Similarly, cross-sectional studies of nonclinical populations suggest that cannabis use follows depression and that impaired motivation is a manifestation of depression rather than a consequence of cannabis use, although the dose-response association of cannabis use and depression has not been consistently reported (5–7). However, anecdotal and cross-sectional studies rely on retrospective reports of depressive symptoms, which are often biased by the reconstruction of memories based on current affective states, particularly in depressed individuals (8, 9). In contrast to cross-sectional studies, longitudinal studies of adult community populations have found an increase in depressive symptoms after cannabis use, although these studies have not controlled for the baseline comorbidity of cannabis use and depression (10–12). Longitudinal studies of children and adolescents have found that depression increases the risk of later cannabis use, rather than vice versa, but not consistently across populations (13, 14).
Overall, the literature on the comorbidity of cannabis abuse and depression is divided. Longitudinal studies suggest that cannabis abuse in adults increases depressive symptoms, whereas cross-sectional studies suggest that a history of depression explains the dysphoria associated with cannabis abuse. The literature leaves open to question if cannabis abuse increases the incidence (i.e., new cases) of depression or if depression increases the incidence of cannabis abuse. Thus, the etiological significance of depression and cannabis abuse as risk factors for cannabis abuse and depression, respectively, is not well understood. The current research addresses these issues through a longitudinal study of a randomly sampled adult population over a nearly 15-year period. Consistent with longitudinal studies and contrary to cross-sectional studies, depressive symptoms were expected to follow cannabis abuse, rather than vice versa.
Method
Participants and Measures
In 1980, the Epidemiologic Catchment Area (ECA) study randomly sampled 3,481 individuals in the Baltimore area by using utility records (15, 16). These individuals were reinterviewed between 1994 and 1996 as part of a follow-up study. Of the 3,481 noninstitutionalized participants, 24.4% (N=848) died before follow-up assessment, which reflects the oversampling of the elderly at baseline. Of the 2,633 remaining participants, 72.9% (N=1,920) were surveyed at the follow-up assessment, with the balance either refusing to participate (N=298) or unlocatable (N=415). After a complete description of the study, written informed consent was obtained from the participants.
Measures
The National Institute of Mental Health Diagnostic Interview Schedule (DIS) (17, 18) was used to assess the symptoms of DSM-III disorders at baseline and DSM-III-R disorders at the follow-up assessment. Baseline cannabis abuse was measured by an indicator of a cannabis use disorder computed by using the DIS algorithms. Cannabis abuse at the follow-up assessment was measured by an indicator of the occurrence of any of eight problems related to cannabis use (e.g., vocational impairment, intoxication while at work).
The number of DSM-III depressive symptoms at baseline was used to measure depression as a risk factor for cannabis abuse at the follow-up assessment. The symptoms counted only if they occurred nearly every day for 2 weeks or more at some point in the participants’ lifetimes. An indicator of the occurrence of any of the nine depressive symptoms during the follow-up period was used as an outcome measure.
Design and Analysis
The risk of depression posed by cannabis abuse was examined in 849 of the 1,920 participants at the follow-up assessment who had no symptoms of depression at baseline. Logistic regression was used to predict the occurrence of any depressive symptoms during the follow-up period in these 849 participants. An indicator of cannabis abuse was forced into the equation first to estimate the risk of depression posed by cannabis abuse. Following entry of this variable, other baseline covariates were force-entered into the equation to adjust the risk estimate for factors that might confound the association of cannabis abuse at baseline and depression at the follow-up assessment.
The risk of cannabis abuse posed by depression was examined in the 1,837 participants who had no diagnosis of cannabis abuse at baseline. Logistic regression was used to predict the occurrence of any cannabis abuse symptoms during the follow-up period in these 1,837 participants. The number of depressive symptoms at baseline was forced into the equation first to estimate the risk of cannabis abuse posed by depression. Following entry of this variable, other baseline covariates were force-entered into the equation to adjust the risk estimate for confounding covariates.
Sociodemographic and other factors that might confound the comorbidity of cannabis and depression were held constant in the analyses. These variables included gender, age, marital status (1=married, 0=not married), race (white=1, nonwhite=0), the highest grade in school or year of college completed at baseline, and household income, which was identified by using several income levels. The number of nine stressful life events (e.g., marital separation, divorce) and six chronic illnesses (e.g., hypertension, diabetes) at baseline were each included in the analysis. An indicator of the receipt of any mental health treatment at baseline also was used in the analysis. The numbers of symptoms of seven psychiatric disorders at baseline were used in the analysis as covariates. Indicators of diagnoses of five forms of substance abuse or dependence also were used in the analysis. The algorithms for the DIS DSM diagnoses in this sample have been described previously and used in several previous studies (16).
Results
Attrition
The participants who could not be located at the time of the follow-up assessment tended to be older and less educated, with lower household incomes, more physical illness, and fewer baseline symptoms of depression, mania, and somatization. These results are consistent with those from a previous report on the ECA follow-up sample (19). In addition, participants lost to follow-up tended to be unmarried compared with those retained (χ2=14.9, df=1, p<0.01) and had a lower prevalence of cannabis abuse than did those retained (2.6% versus 4.3%, respectively; χ2=6.6, df=1, p<0.05).
Baseline Cannabis Abuse and Depression
Of the 1,920 subjects retained, the 83 participants with a baseline cannabis abuse diagnosis reported more baseline depressive symptoms than the 1,837 without a cannabis abuse diagnosis (F=36.3, df=1, 1918, p<0.0001). In the 83 participants with a baseline diagnosis of cannabis abuse, differences between those with and without depressive symptoms were examined. The 15 who reported no depressive symptoms were not significantly different from the 68 who did report depressive symptoms, except that the latter group had more symptoms of mania (F=5.7, df=1, 81, p<0.04) and somatization (F=6.7, df=1, 81, p<0.05). Thus, the cohort of 15 cannabis abusers followed for assessment of depression risk was a representative sample of cannabis abusers in this population at baseline.
Risk of Depressive Symptoms at Follow-Up Assessment
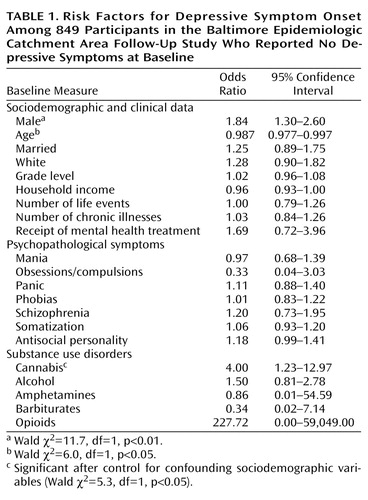
The risk of the onset of depressive symptoms during the follow-up period in participants diagnosed with cannabis abuse at baseline was about four times greater than the risk in participants without a baseline cannabis abuse diagnosis (odds ratio=4.49, 95% confidence interval [CI]=1.51–13.26; Wald χ2=7.4, df=1, p<0.01). This association was little changed after adjusting for the association of baseline depressive symptoms with other possibly confounding covariates. The risk of depressive symptoms remained about four times greater in participants diagnosed with cannabis abuse at baseline than in those without a baseline cannabis abuse diagnosis (Table 1).
Of the 267 participants who experienced depressive symptoms during the follow-up period, 3.7% (N=10) had been diagnosed with cannabis abuse at baseline, whereas only 0.9% (N=5) of the 582 participants who did not report depressive symptoms had a baseline cannabis abuse diagnosis. A significant association of cannabis abuse at baseline and depressive symptoms at the follow-up assessment was found (χ2=8.0, df=1, p<0.01). Fisher’s exact test was performed to test the statistical significance of this association, since the expected count of participants with both a baseline cannabis abuse diagnosis and depressive symptoms at the follow-up assessment was less than five. After this test (either one-tailed or two-tailed), the association remained significant (p<0.01).
Risk of Cannabis Abuse Symptoms at Follow-Up Assessment
In the 1,837 participants with no diagnosis of cannabis abuse at baseline, the occurrence of any cannabis abuse symptoms during the follow-up period was not significantly predicted by baseline depressive symptoms, either with or without adjustment for baseline covariates. The significant baseline covariates for cannabis abuse at the follow-up assessment included amphetamine abuse (odds ratio=7.77, 95% CI=1.82–33.07; Wald χ2=7.7, df=1, p<0.01), opioid abuse (odds ratio=10.46, 95% CI=1.43–76.16; Wald χ2=5.4, df=1, p<0.05), female gender (odds ratio=0.32, 95% CI=0.19–0.53; Wald χ2=20.7, df=1, p<0.001), and age (odds ratio=0.88, 95% CI=0.85–0.91; Wald χ2=62.9, df=1, p<0.001). None of the other covariates entered in the equation was significant.
Post Hoc Analyses
A post hoc analysis was performed to identify the particular symptoms of depression predicted by cannabis abuse. The occurrence of each of the nine depressive symptoms during the follow-up period was predicted by using the same baseline measures used to predict the incidence of any of the symptoms. Only suicidal ideation and anhedonia during the follow-up period were predicted by a baseline diagnosis of cannabis abuse. Of the 98 participants with anhedonia, 35 also had suicidal ideation (χ2=64.6, df=1, p<0.001).
The incidence of suicidal ideation was approximately four times greater in cannabis abusers than in nonabusers (odds ratio=4.55, 95% CI=1.37–15.12; Wald χ2=6.1, df=1, p<0.05) after adjustment for baseline covariates. The significant baseline covariates of suicidal ideation during the follow-up period included female gender (odds ratio=1.90, 95% CI=1.11–3.24; Wald χ2=5.6, df=1, p<0.05), age (odds ratio=0.98, 95% CI=0.95–0.98; Wald χ2=20.1, df=1, p<0.05), and white race (odds ratio=1.86, 95% CI=1.09–3.15; Wald χ2=5.2, df=1, p<0.05). None of the other covariates entered into the equation was significant. Of the 97 participants with thoughts about death during the follow-up period, six (6.2%) had a cannabis abuse diagnosis at baseline, whereas nine (1.2%) of the 752 participants without thoughts of death had a baseline diagnosis of cannabis abuse (χ2=12.3, df=1, p<0.01). Fisher’s exact test found this association to be significant (p<0.01).
Similarly, the incidence of anhedonia was approximately four times greater in cannabis abusers than in nonabusers (odds ratio=4.32, 95% CI=1.32–14.16; Wald χ2=5.8, df=1, p<0.05) after adjustment for the baseline covariates entered into the equation. The significant baseline covariates of anhedonia during the follow-up period were age (odds ratio=0.97, 95% CI=0.96–0.99; Wald χ2=12.4, df=1, p<0.0001) and antisocial symptoms (odds ratio=1.42, 95% CI=1.16–1.75; Wald χ2=11.1, df=1, p<0.001). None of the other covariates entered into the equation was significant. Of the 98 participants who experienced anhedonia during the follow-up period, six (6.1%) had a baseline diagnosis of cannabis abuse, whereas nine (1.2%) of the 751 participants who did not experience anhedonia had a baseline diagnosis of cannabis abuse (χ2=12.1, df=1, p<0.01). Fisher’s exact test found this association to be significant (p<0.01).
Discussion
The increase in incidence of depressive symptoms in individuals who abused cannabis cannot be explained by an underreporting of baseline depressive symptoms, given that they were more likely to report depressive symptoms than individuals who did not abuse cannabis, as reported here and in many other studies (5–9). The risk of depression found here also cannot be explained by factors confounded with cannabis abuse, which were ruled out as superior predictors of depressive symptoms (e.g., alcohol abuse, age, stressful life events). Nonetheless, confounding characteristics not assessed at baseline, and therefore not available for analysis, may account for the greater risk of depressive symptoms (e.g., suicidal ideation and anhedonia) in adults diagnosed with cannabis abuse. Further research is required to identify other characteristics of individuals who abuse cannabis that may explain their greater risk of subsequent depressive symptoms.
The inability to locate individuals with depressive and cannabis abuse symptoms during the follow-up period may have resulted in an underestimation of their association. Bias in the estimation of this association would have been introduced if the retention of individuals with one set of symptoms was greater than the retention of individuals with the other set of symptoms, which was not the case. Selective retention of individuals with certain characteristics assessed here is not likely to have biased the estimates, since these characteristics failed to confound the estimated associations. Although the estimated associations are based on small numbers of individuals and represent small effect sizes, the results may nonetheless generalize to large numbers of people in the general population, and the small effect sizes may nonetheless have great practical validity(20).
The results underscore the importance of cannabis abuse prevention rather than treatment because they address the incidence (i.e., new cases) of depressive symptoms rather than the prevalence of depressive disorder. This finding extends those of the national ECA study (1), which found that alcohol abuse and cocaine, but not cannabis or other drugs, were risk factors for suicide over the initial 1–2-year period of the study (1980–1981).
Obviously, causal associations or other mechanisms that explain the higher risk of depression in cannabis abusers cannot be determined by an epidemiological survey. However, a physiological mechanism underlying a causal association of cannabis use and suicide has been proposed, although it is somewhat limited to young male subjects (21). Cannabis increases levels of interferon-gamma, which inhibits the activity of aromatase, the enzyme that converts androgens to estrogen. This in turn creates a deficiency in estrogen, a hormone that augments the synthesis of serotonin, thereby creating a deficiency in serotonin characteristic of major depression and suicide. Further research with animal models of cannabis-induced depression may be warranted.
The finding here that baseline depressive symptoms failed to predict subsequent cannabis abuse symptoms is not inconsistent with other research that has found that antidepressant medications reduce cannabis use in clinical populations of adult alcoholics (22). Treating depression may reduce cannabis use in clinical populations, but depression did not necessarily lead these individuals to initiate cannabis use. Further, the results of the current research do not necessarily have implications for public policy regarding the decriminalization of cannabis. A reduction in cannabis abuse, as opposed to its prevention, will not necessarily reduce levels of dysphoria in the general population. Also, such a reduction would not necessarily impact public health or health service utilization, given that the level of dysphoria observed was subclinical. Subclinical levels of anhedonia in cannabis abusers may constitute an “amotivational” syndrome, but the degree to which such an amotivational syndrome impairs social or occupational functioning cannot be ascertained here and requires further study. Nonetheless, such subclinical dysphoria could represent a preclinical condition, particularly in certain subpopulations.
Finally, the results of this study do not have obvious implications for policies regarding the prescription of cannabis for medical conditions. The creation of depression as a result of prescribed cannabis use cannot be ascertained on the basis of the current study, which examined the self-administration of excessive levels of cannabis from illicit sources in an uncontrolled context. Thus, the higher suicide risk associated with cannabis abuse will not necessarily occur in cases in which cannabis is medically prescribed, even if patients have terminal illnesses or other disorders that also increase their suicide risk. Despite the limitations of the current study, the results suggest that the potentially serious consequences of cannabis abuse require further research.
 |
Received March 1, 2001; revision received June 20, 2001; accepted Aug. 1, 2001. From the University of Pennsylvania Treatment Research Center. Address reprint requests to Dr. Bovasso, University of Pennsylvania Treatment Research Center, 3900 Chestnut St., Bldg. 3, Philadelphia, PA 19104; [email protected] (e-mail). Supported by grants from NIMH (MH-47447 and MH-14592), the National Institute on Drug Abuse (DA-05186), and the Department of Veterans Affairs (D-05858).
1. Petronis KR, Samuels JF, Moscicki EK, Anthony JC: An epidemiologic investigation of potential risk factors for suicide attempts. Soc Psychiatry Psychiatr Epidemiol 1990; 25:193-199Medline, Google Scholar
2. Rowe MG, Fleming MF, Barry KL, Manwell LB, Kropp S: Correlates of depression in primary care. J Fam Pract 1995; 41:551-558Medline, Google Scholar
3. Khantzian E: The self-medication hypothesis of substance abuse disorders: a reconsideration and recent applications. Harv Rev Psychiatry 1997; 4:231-244Crossref, Medline, Google Scholar
4. Frances RJ: The wrath of grapes versus the self-medication hypothesis. Harv Rev Psychiatry 1997; 4:287-289Crossref, Medline, Google Scholar
5. Kupfer DJ, Detre T, Koral J, Fajans P: A comment on the “amotivational syndrome” in marijuana smokers. Am J Psychiatry 1973; 130:1319-1322Link, Google Scholar
6. Musty RE, Kaback L: Relationships between motivation and depression in chronic marijuana users. Life Sci 1995; 56:2151-2158Crossref, Medline, Google Scholar
7. Troisi A, Pasani A, Saracco M, Spalleta G: Psychiatric symptoms in male cannabis users not using other illicit drugs. Addiction 1998; 4:487-492Crossref, Google Scholar
8. Murray LA, Whitehouse WG, Alloy LB: Mood congruence and depressive deficits in memory: a forced-recall analysis. Memory 1999; 7:175-196Crossref, Medline, Google Scholar
9. Watkins PC, Vache K, Verney SP, Mathews A: Unconscious mood-congruent memory bias in depression. J Abnorm Psychol 1996; 105:34-41Crossref, Medline, Google Scholar
10. Angst J: Comorbidity of mood disorders: a longitudinal prospective study. Br J Psychiatry Suppl (June) 1996; 168(30):31-37Google Scholar
11. Grant BF: Comorbidity between DSM-IV drug abuse disorders and major depression: results of a national survey. J Subst Abuse 1995; 7:481-497Crossref, Medline, Google Scholar
12. Weller RA, Halikas JA: Marijuana use and psychiatric illness: a follow-up study. Am J Psychiatry 1985; 142:848-850Link, Google Scholar
13. Block JH, Gjerde PF, Block JH: Personality antecedents of depressive tendencies in 18-year-olds: a prospective study. J Pers Soc Psychol 1991; 60:726-738Crossref, Medline, Google Scholar
14. Way N, Stauber HY, Nakkula MJ, London P: Depression and substance use in two divergent high school cultures: a quantitative and qualitative analysis. J Youth and Adolescence 1994; 23:331-357Crossref, Google Scholar
15. Eaton WW, Kessler LG: Epidemiologic Field Methods in Psychiatry. Orlando, Fla, Academic Press, 1985Google Scholar
16. Robins LN, Regier DA (eds): Psychiatric Disorders in America: The Epidemiological Catchment Area Study. New York, Free Press, 1991Google Scholar
17. Robins LN, Helzer JE, Croughan J (eds): National Institute of Mental Health Diagnostic Interview Schedule, version III: PHS Publication ADM-T-42-3. Rockville, Md, NIMH, 1981Google Scholar
18. Robins LN, Helzer JE, Croughan J, Ratcliff KS: The National Institute of Mental Health Diagnostic Interview Schedule: its history, characteristics, and validity. Arch Gen Psychiatry 1981; 38:381-389Crossref, Medline, Google Scholar
19. Badawi MA, Eaton WW, Myllyluoma J, Weimer LG, Gallo J: Psychopathology and attrition in the Baltimore ECA 15-year follow-up 1981-1996. Soc Psychiatry Psychiatr Epidemiol 1999; 34:91-98Crossref, Medline, Google Scholar
20. Rosenthal R, Rosnow RL: Essentials of Behavioral Research: Methods and Data Analysis. New York, McGraw-Hill, 1991Google Scholar
21. Holden RJ, Pakula I: Marijuana, stress and suicide: a neuroimmunological explanation. Aust NZ J Psychiatry 1998; 32:465-466Medline, Google Scholar
22. Cornelius JR, Salloum IM, Haskett RF, Ehler JG, Jarrett PJ, Thase ME, Perel JM: Fluoxetine versus placebo for the marijuana use of depressed alcoholics. Addict Behav 1999; 24:111-114Crossref, Medline, Google Scholar



