Mental Disorders and the Use of Alternative Medicine: Results From a National Survey
Abstract
OBJECTIVE: The study examined the relationship between mental disorders and the use of complementary and alternative medicine. METHOD: Data from a national household telephone survey conducted in 1997–1998 (N=9,585) were used to examine the relationships between use of complementary and alternative medicine during the past 12 months and several demographic variables and indicators of mental disorders. Structured diagnostic screening interviews were used to establish diagnoses of probable mental disorders. RESULTS: Use of complementary and alternative medicine during the past 12 months was reported by 16.5% of the respondents. Of those respondents, 21.3% met diagnostic criteria for one or more mental disorders, compared to 12.8% of respondents who did not report use of alternative medicine. Individuals with panic disorder and major depression were significantly more likely to use alternative medicine than those without those disorders. Respondents with mental disorders who reported use of alternative medicine were as likely to use conventional mental health services as respondents with mental disorders who did not use alternative medicine. CONCLUSIONS: We found relatively high rates of use of complementary and alternative medicine among respondents who met criteria for common mental disorders. Practitioners of alternative medicine should look for these disorders in their patients, and conventional medical providers should ask their depressed and anxious patients about the use of alternative medicine. More research is needed to determine if individuals with mental disorders use alternative medicine because conventional medical care does not meet their health care needs.
The Surgeon General’s recent report on mental health (1) emphasized the high rates of mental disorders in the United States and pointed out that many who suffer from these disorders do not receive mental health treatments that have been shown to be efficacious. It has been well established that persons with common mental disorders such as depression or anxiety are frequent users of general medical services (2, 3), but little is known about their use of alternative medical services. If a substantial unmet need for mental health care exists, then persons with mental illness might be expected to turn for help to alternative providers or therapies outside the formal health care system. The study reported here examined the use of complementary and alternative medicine among survey respondents who met criteria for a number of common mental disorders. The study used data from a large national survey of 9,585 adults.
Typical problems for which persons see alternative providers include back problems, anxiety, headaches, insomnia, depression, arthritis, and allergies (4, 5). Several recent studies have suggested high rates of depression or anxiety among users of alternative medicine (4, 6–10). Eisenberg et al. (7) found that 40.9% of the adults who reported severe depression and 42.7% of those who reported anxiety attacks had used alternative therapies in the past 12 months, compared with 28.2% of adults in the overall sample. Druss et al. (11) found that major depression was a significant predictor of use of both antidepressants and nonprescription dietary supplements. Burstein et al. (12) examined use of alternative medicine among women with early-stage breast cancer and found relatively high rates of depression among women who were new users of alternative medicine. Davidson et al. (13) administered structured diagnostic interviews (Structured Clinical Interview for DSM-III-R) to 83 users of complementary and alternative medicine services in the United States and the United Kingdom. The majority (69%) met lifetime criteria for an axis I disorder, and 40% met criteria for a current axis I disorder, most frequently an anxiety or depressive disorder. The authors concluded that individuals with depression or anxiety disorders may be particularly interested in pursuing alternative medicine services and called for greater awareness of the possibility of psychiatric illness in persons who seek help from the complementary medicine sector.
Most studies of the relationship between mental disorders and use of alternative medicine have used small and nonrepresentative samples or have used simple self-reports of the presence or absence of mental disorders, rather than more standardized interviews. In the study reported here, we used a household sample and included standardized screening measures for specific psychiatric disorders to examine the association between mental disorders and the use of alternative medicine, while controlling for potentially confounding demographic and health status factors. We hypothesized that respondents with common mental disorders such as depression or anxiety would have higher rates of complementary and alternative medicine use.
Method
Data Source and Sample
We analyzed data from a pre-release version of Healthcare for Communities, a national household telephone survey funded by the Robert Wood Johnson Foundation and fielded in 1997–1998 (14). Healthcare for Communities researchers reinterviewed adults who had participated in an earlier telephone survey, the Community Tracking Study, an average of 15 months after the earlier study. The Community Tracking Study sample was representative of the U.S. civilian, noninstitutionalized population (15) and included individuals clustered within 60 randomly selected U.S. communities, as well as a geographically dispersed subsample. In 12 communities that were considered primary sites, a larger sample size allowed for site-specific estimates. The remaining 48 communities were considered secondary sites. Community Tracking Study researchers interviewed all adults and one randomly selected child within each participating household. In the primary sites, the study included a small field sample, so that households with little or no chance of being selected in a telephone survey could be represented. A sample of 14,985 individuals was selected for the Healthcare for Communities survey from a random sample of 30,375 adult respondents to the Community Tracking Study telephone interview. To allow for more power for national estimates with the reduced sample size, Healthcare for Communities oversampled individuals from the geographically dispersed sample and from the secondary sites in the Community Tracking Study. To obtain more precise national estimates of mental health care needs, Healthcare for Communities also oversampled individuals from the previous study who had reported low income, high levels of psychological distress, and use of mental health specialty services. The sample was stratified by family income (£$20,000 versus >$20,000), psychological distress (distressed versus nondistressed, determined on the basis of subjects’ responses to two mental health items in the 12-Item Short-Form Health Survey [16]), and use of mental health specialty services in the past 12 months (use versus no use). Healthcare for Communities selected everyone who reported psychological distress or mental health service use (N=7,164). We sampled among the nondistressed nonusers of mental health services to obtain a group of 4,305 nonpoor, nondistressed nonusers of services and a group of 3,516 poor, nondistressed nonusers. Of the 14,985 respondents selected for the sample, 9,585 completed the Healthcare for Communities interview, for a response rate of 64.0%. The study was approved by the institutional review boards at RAND and UCLA. After complete description of the study to the subjects, informed consent was obtained from all subjects. Sampling weights based on the inverse of the probability of selection were derived. The weights included adjustments for nonresponse and for the exclusion of households without telephones.
Measures
The Healthcare for Communities telephone survey included questions on demographic characteristics, health and daily activities, mental health, alcohol and drug use, insurance coverage, and the use of medications and health services. Specifically, we asked whether respondents had made any primary care visits, made any primary care visits that addressed mental health problems, used specialty mental health care, or used psychotropic medications. We used an indicator developed in earlier work to assess appropriate use of psychotropic medication or counseling for respondents with probable depressive or anxiety disorders (17). To assess the use of complementary and alternative medicine, we asked participants the following question: “In the past 12 months, did you use any alternative or folk medicine, either from a practitioner or on your own?” We included the following statement to give examples of alternative medicine therapies: “Alternative medicine includes therapies like homeopathic medicine, acupuncture, massage therapy, herbal medicine, and spiritual healing.” Individuals who reported the use of alternative medicine were asked if they used alternative medicine to help with emotional, mental health, alcohol, or drug abuse problems.
Other studies have used somewhat different methods to assess the use of alternative medicine. For example, Eisenberg et al. (4) used a relatively broad definition of “unconventional medicine” that included such treatments as relaxation techniques, herbal medicine, massage, chiropractic, spiritual healing by others, megavitamins, self-help groups, imagery, commercial diets, folk remedies, lifestyle diets, energy healing, homeopathy, hypnosis, biofeedback, and acupuncture. In recent years, it has become harder to make clear distinctions between conventional and alternative medicine. As medical schools have developed courses in alternative and complementary medicine, insurers have started to cover many treatments previously considered “alternative” (i.e., chiropractic and acupuncture) and prominent hospitals have started centers for “alternative,” “complementary,” or “integrative” medicine. We asked respondents to use their own judgment about whether the services they reported were considered “alternative,” given the definition reported above.
We assessed the presence of mental disorders by using a structured diagnostic interview. Questions on generalized anxiety disorder and major depression were based on the World Health Organization (WHO) Composite International Diagnostic Interview Short Form (18). Questions on dysthymia, panic disorder, and mania were derived from items in the WHO Composite International Diagnostic Interview (19). Alcohol use/abuse was assessed by using the Alcohol Use Disorders Identification Test (20). Drug abuse was assessed by using a screening instrument described by Rost and colleagues (21). We also included a question about lifetime history of having been hospitalized for schizophrenia or symptoms of psychosis.
Analysis
We used t tests and chi-square tests to examine the association of use of complementary and alternative medicine with several demographic variables, several indicators of mental disorders (depression, dysthymia, panic disorder, generalized anxiety disorder, and severe mental illness such as bipolar disorder or psychosis), and an indicator of probable alcohol or drug abuse. We also used chi-square tests to examine whether respondents with mental disorders who did and did not report use of alternative medicine differed in their use of and satisfaction with conventional mental health services.
We then developed a series of logistic regression models to predict the use of alternative medicine. Because substantial overlap exists among the specific mental disorders we studied, we first developed a model containing all of the indicators for mental disorders and then a full model containing all of the diagnoses and a number of demographic and health status factors such as gender, geographic area, level of education, age, marital status, ethnic minority status, employment status, insurance status, and overall satisfaction with health care.
Our analyses were weighted to account for the disproportionate sampling of respondents from the Community Tracking Study and to be nationally representative (14). We used SUDAAN statistical software (22) to adjust our analyses for the clustering.
Results
Of the total of 9,585 respondents who agreed to participate in the telephone survey for this study, 19 answered “don’t know” or refused to answer the question about use of complementary and alternative medicine. Of the remaining 9,566 respondents, 1,576 reported use of alternative medicine in the past 12 months, resulting in an unweighted proportion of 16.5%. After weighting, we estimated the prevalence of the use of alternative medicine to be 14.5%. From this point on, we present only weighted proportions.
Among those who reported using alternative medicine, 15.0% reported that they had used it to treat mental or emotional problems, 45.4% reported at least one visit to an alternative medicine practitioner, and 54.6% either self-administered alternative treatments or received treatments from a traditional health care provider (we do not have data to distinguish these two possibilities).
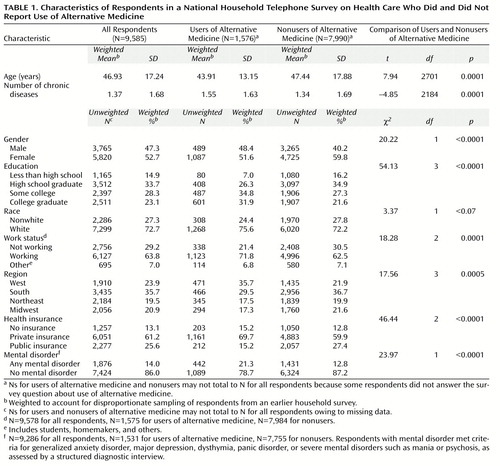
Table 1 shows the characteristics of the study participants and the differences between study participants who did and did not report use of alternative medicine in the 12 months before the study. Individuals who reported use of alternative medicine were significantly more likely to meet diagnostic criteria for at least one of the mental disorders we assessed.
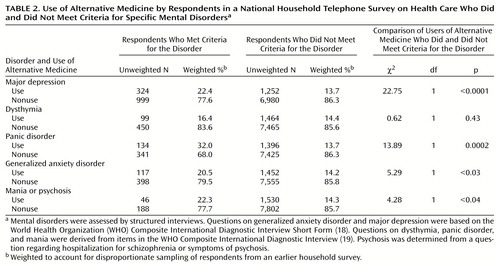
Table 2> shows the association between use of alternative medicine and each of the mental disorders we assessed. Use of alternative medicine was significantly more likely among respondents who met criteria for any of the disorders except for dysthymia. Respondents who met criteria for major depression and panic disorder were particularly likely to report the use of alternative medicine.
Respondents with more than one mental disorder were not significantly more likely to use alternative medicine than those who met criteria for just one disorder (22.4% versus 21.5%) (χ2=0.10, df=1, p=0.76). Use of alternative medicine was significantly higher among respondents who reported that they needed help with emotional or substance abuse problems in the past 12 months than among those who did not report needing such help (30.1% versus 12.7%) (χ2=86.31, df=1, p<0.001).
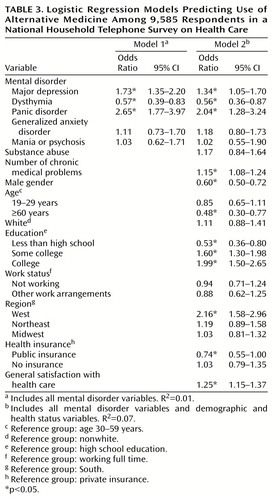
After controlling for all mental disorders in our logistic regression model (Table 3, model 1), we found that major depression and panic disorder remained significantly associated with the use of alternative medicine. In addition, in the model that controlled for the other disorders, a significant association between dysthymia and use of alternative medicine emerged. In the full model that included all mental disorder diagnoses and demographic and clinical covariates (Table 3, model 2), major depression, dysthymia, panic disorder, gender, age, level of education, geographic area, severity of chronic medical illness, type of insurance, and general satisfaction with health care were significantly associated with use of alternative medicine. When all other factors were controlled, participants with generalized anxiety disorder and with severe mental disorders (probable bipolar disorder or schizophrenia) did not have significantly higher rates of alternative medicine use than those without those disorders. Participants who met criteria for dysthymia were significantly less likely to report use of alternative medicine than those who did not meet those criteria.
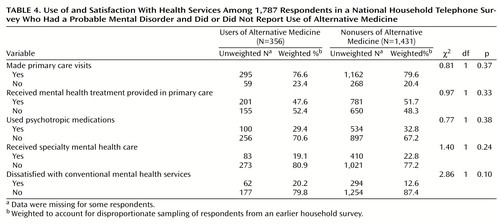
Table 4 shows the association between the use of alternative medicine, the use of conventional mental health treatments, and satisfaction with available mental health services among the 1,787 respondents who met criteria for at least one mental disorder and used any health services (primary, specialty, or alternative care) in the year before the survey. In this subgroup, respondents who used alternative medicine were as likely as those who did not to report having made primary care visits, having received mental health treatments in primary care, having used specialty mental health care, and having used psychotropic medications. All of the users of alternative medicine in this group also used at least one of the conventional mental health treatments we asked about (mental health treatment in primary care, a psychotropic medication, or specialty mental health care).
When we examined participants’ ratings of “health care available for personal or emotional problems during the past 12 months,” we found that 20.3% of those who used alternative medicine reported being dissatisfied, compared with 12.6% of those who did not use alternative medicine (χ2=2.86, df=1, p<0.10).
Among the 1,762 respondents who met diagnostic criteria for common mental disorders (anxiety or depressive disorders), those who used alternative medicine were more likely to have received appropriate treatment with psychotropic medications or counseling than those who did not use alternative medicine (50.1% versus 30.2%) (χ2=23.14, df=1, p<0.001).
Discussion
In our sample, about 21% of complementary and alternative medicine users met diagnostic criteria for at least one probable mental disorder (compared to about 13% of nonusers). About 15% of those who reported using alternative medicine said that they were using these services to help with emotional, mental, or substance abuse problems. This rate is consistent with the rates of 13% reported by Elder et al. (23) and 11% reported by Kelner and Wellman (24) but lower than the rates reported by Eisenberg (4), who found that users of alternative medicine considered anxiety and depression some of the most common indications for the use of those services (for 28% and 20% of users, respectively). The discrepancy may be due to differences in the populations sampled, in the way we defined and elicited information about alternative medicine use, or in the way we elicited the reason for alternative medicine use.
Our findings suggest that practitioners of alternative medicine should be aware that a considerable number of their patients may be suffering from common mental disorders such as major depression or panic disorder. For these patients, consultation and collaboration with a specialty mental health practitioner should be strongly considered if they do not respond to alternative medicine treatments as expected. We also encourage all primary care providers and mental health specialists who are treating patients with major depression and anxiety disorders to inquire about the use of alternative treatments. Clinicians’ knowledge of such treatments and, when indicated, coordination with providers of alternative medicine might improve overall health care for these patients and prevent potentially harmful interactions between conventional and alternative treatments (25, 26).
When we examined use of alternative medicine among individuals with specific mental disorders, we found relatively high rates of use among individuals with major depression and panic disorder, even after the analysis adjusted for comorbid mental disorders and demographic and health status variables. In addition, after this adjustment, the associations between use of alternative medicine, generalized anxiety disorder, and severe mental disorders were no longer significant, and individuals with dysthymia were actually significantly less likely to report use of alternative medicine. However, these results may be due to relatively high rates of comorbidity between these disorders.
Our research also confirmed previously identified associations between use of alternative medicine and number of factors, such as female gender, middle age, a higher level of education, a higher level of medical illness, and residence in the Western part of the United States (7, 24, 27, 28).
Our overall estimates of alternative medicine use are lower than those previously reported (4, 7, 20, 27, 29, 30) but higher than the rate reported by Druss and Rosenheck (31). The discrepancy may be due to differences in the populations studied and the definitions of complementary and alternative medicine used. For example, we did not include chiropractic medicine in our definition of alternative medicine, as this treatment is now covered by a large number of health insurers and most states have health insurance mandates to cover chiropractic care (28).
Our study sampled a larger population than most previously reported surveys about alternative medicine, but the data we collected have some limitations. We relied on respondents’ recall of services used over a 12-month period, and this long recall period may have resulted in some underreporting of alternative medicine use. We provided a definition of alternative medicine, but we relied on respondents to classify treatments they were reporting as “alternative.” We did not collect detailed information on why respondents used alternative medicine except for asking if the services had been used to treat mental or emotional problems. A number of theories for the use of alternative medicine have been advanced in earlier studies (5, 24, 29, 30, 32–35), and we cannot add to this discussion.
We did not collect detailed information about what specific types of alternative medicine treatments were used. We did collect information about medications taken several times a week for at least 1 month in the past year, and we found that 3.7% of the respondents with probable depression or dysthymia reported the use for at least 1 month of St. John’s wort (hypericum), an over-the-counter herbal product for which there is some empirical evidence of efficacy (36–38). We cannot determine from our data if the use of this compound represented self-use or was recommended by a traditional or alternative health care provider. Additional research should examine the nature of the alternative medicine treatments used by individuals with mental disorders in greater detail. It would, for example, be important to know whether people are using alternative treatments for which there is some evidence of efficacy.
Most users of alternative medicine also use conventional medical treatments, and some researchers (31) have suggested that alternative medicine is used as a complementary treatment to conventional health care rather than as a substitute. In our study, users of alternative medicine who met criteria for mental disorders were as likely to use primary care or conventional mental health treatments as those who did not use alternative medicine. All respondents who met probable diagnostic criteria for mental disorders and reported using alternative medicine also reported using at least one of the conventional mental health services we asked about, suggesting that, in this sample, use of alternative medicine was indeed complementary to conventional treatments. Persons with high levels of psychological distress may be more likely to use a range of available treatments, including conventional mental health and alternative medicine treatments.
Alternative medicine users with probable depressive or anxiety disorders were somewhat more likely to receive conventional mental health care that met criteria for appropriate care than were those who did not use alternative medicine. On the other hand, respondents with probable mental disorders who used alternative medicine reported a somewhat lower level of satisfaction with available mental health services than those who did not, although the difference was not statistically significant. It is possible that patients with mental disorders attempt to get help in the conventional medical sector and then turn to alternative medicine if they feel that they have not been helped by conventional medicine. However, our cross-sectional data do not allow us to adequately test this hypothesis.
In summary, we found relatively high rates of use of complementary and alternative medicine in individuals with common mental disorders, particularly major depression and panic disorder. Further research is needed to examine the nature and quality of alternative medicine treatments used by persons with mental disorders and to determine whether these individuals use alternative medicine treatments because conventional medical and mental health care does not properly address their health care needs. Such research may help us improve conventional medical services for these persons and may suggest ways of coordinating services across the conventional and alternative health care sectors to provide better care to patients.
 |
 |
 |
 |
Received March 14, 2000; revision received June 12, 2000; accepted July 6, 2000. From UCLA Neuropsychiatric Institute, and RAND, Santa Monica, Calif. Address reprint requests to Dr. Unützer, Center for Health Services Research, UCLA Neuropsychiatric Institute, 10920 Wilshire Blvd., Suite 300, Los Angeles, CA 90024; [email protected] (e-mail).Supported by a grant from the Robert Wood Johnson Foundation (Dr. Wells, principal investigator).
1. Mental Health: A Report of the Surgeon General. Rockville, Md, US Department of Health and Human Services, Substance Abuse and Mental Health Services Administration, Center for Mental Health Services, National Institute of Mental Health, 1999Google Scholar
2. Simon GE, VonKorff M, Barlow W: Health care costs of primary care patients with recognized depression. Arch Gen Psychiatry 1995; 52:850-856Crossref, Medline, Google Scholar
3. Unützer J, Patrick DL, Simon G, Grembowski D, Walker E, Rutter C, Katon W: Depressive symptoms and the costs of health services in HMO patients aged 65 years and older: a 4-year prospective study. JAMA 1997; 277:1618-1623Google Scholar
4. Eisenberg DM, Kessler RC, Foster C, Norlock FE, Calkins DR, Delbanco TL: Unconventional medicine in the United States. N Engl J Med 1993; 328:246-252Crossref, Medline, Google Scholar
5. Vincent C, Furnham A: Complementary Medicine: A Research Perspective. Chicester, UK, John Wiley & Sons, 1997Google Scholar
6. Jacobs J, Crothers D: Who sees homeopaths? Br Homeopath J 1991; 80:57-58Google Scholar
7. Eisenberg DM, Davis RB, Ettner SL, Appel S, Wilkey S, Van Rompay M, Kessler RC: Trends in alternative medicine use in the United States, 1990-1997. JAMA 1998; 280:1569-1575Google Scholar
8. Jansen GRHJ, Koster TGC: Complaints and diagnoses in homeopathic practice: a tentative stock taking. Br Homeopath J 1995; 84:40-43Crossref, Google Scholar
9. Hollifield M, Katon W, Spain D, Pule L: Anxiety and depression in a village in Lesotho, Africa: a comparison with the United States. Br J Psychiatry 1990; 156:343-350Crossref, Medline, Google Scholar
10. Katerndahl DA, Realini JP: Where do panic attack sufferers seek care? J Fam Pract 1995; 40:237-243Google Scholar
11. Druss BG, Rohrbaugh R, Kosten T, Hoff R, Rosenheck RA: Use of alternative medicine in major depression. Psychiatr Serv 1998; 46:1397Link, Google Scholar
12. Burstein HJ, Gelber S, Guadagnoli E, Weeks JC: Use of alternative medicine by women with early-stage breast cancer. N Engl J Med 1999; 340:1733-1739Google Scholar
13. Davidson JR, Rampes H, Eisen M, Fisher P, Smith RD, Malik M: Psychiatric disorders in primary care patients receiving complementary medical treatments. Compr Psychiatry 1998; 39:16-20Crossref, Medline, Google Scholar
14. Sturm R, Gresenz C, Sherbourne C, Minnium K, Klap R, Bhattacharya J, Farley D, Young AS, Burnam MA, Wells KB: The design of Healthcare for Communities: a study of health care delivery for alcohol, drug abuse, and mental health conditions. Inquiry 1999; 36:221-233Medline, Google Scholar
15. Kemper P, Blumenthal D, Corrigan JM, Cunningham PJ, Felt SM, Grossman JM, Kohn LT, Metcalf CE, St Peter RF, Strouse RC, Ginsburg PB: The design of the Community Tracking Study: a longitudinal study of health system change and its effects on people. Inquiry 1996; 33:195-206Medline, Google Scholar
16. Ware J Jr, Kosinski M, Keller SD: A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care 1996; 34:220-233Crossref, Medline, Google Scholar
17. Young AS, Klap R, Sherbourne CD, Wells KB: The quality of care for depressive and anxiety disorders in the United States. Arch Gen Psychiatry (in press)Google Scholar
18. Kessler RC, Andrews G, Mroczek D, Ustun B, Wittchen HU: The World Health Organization Composite International Diagnostic Interview Short Form (CIDI-SF). Int J Methods in Psychiatr Res (in press)Google Scholar
19. World Health Organization: Composite International Diagnostic Interview (CIDI), version 1.0. Geneva, WHO, 1990Google Scholar
20. World Health Organization: The Alcohol Use Disorders Identification Test (AUDIT): Guidelines for Use in Primary Health Care. Geneva, WHO, 1992Google Scholar
21. Rost K, Burnam MA, Smith GR: Development of screeners for depressive disorders and substance abuse disorder history. Med Care 1993; 31:189-200Crossref, Medline, Google Scholar
22. SUDAAN: Professional Software for Survey Data Analysis, Version 7.5. Research Triangle Park, NC, Research Triangle Institute, 1997Google Scholar
23. Elder NC, Gillerist A, Minz R: Use of alternative health care by family practice patients. Arch Fam Med 1997; 6:181-184Crossref, Medline, Google Scholar
24. Kelner M, Wellman B: Who seeks alternative healthcare? a profile of the users of five modes of treatment. J Altern Complement Med 1997; 3:127-140Crossref, Medline, Google Scholar
25. Shaw D, Leon C, Kolev S, Murray V: Traditional remedies and food supplements: a 5-year toxicological study (1991–1995). Drug Safety 1997; 17:342-356Crossref, Medline, Google Scholar
26. Slifman NR, Obermeyer WR, Aloi BK, Musser SM, Correll WA, Cichowicz SM, Betz JM, Love LA: Contamination of botanical dietary supplements by digitalis lanata. N Engl J Med 1998; 339:806-811Crossref, Medline, Google Scholar
27. Millar WJ: Use of alternative health care practitioners by Canadians. Can J Public Health 1997; 88:154-158Crossref, Medline, Google Scholar
28. Sturm R, Unützer J: State legislation and the use of complementary and alternative medicine. Inquiry (in press)Google Scholar
29. Astin JA: Why patients use alternative medicine: results of a national study. JAMA 1998; 279:1548-1553Google Scholar
30. Pelletier KR, Marie A, Krasner M, Haskell WL: Current trends in the integration and reimbursement of complementary and alternative medicine by managed care, insurance carriers, and hospital providers. Am J Health Promot 1997; 12:112-122Crossref, Medline, Google Scholar
31. Druss BG, Rosenheck RA: Association between use of unconventional therapies and conventional medical services. JAMA 1999; 282:651-656Crossref, Medline, Google Scholar
32. Furnham A, Smith C: Choosing alternative medicine: a comparison of the beliefs of patients visiting a general practitioner and a homeopath. Soc Sci Med 1988; 26:685-689Crossref, Medline, Google Scholar
33. Sutherland LR, Verhoef MJ: Why do patients seek a second opinion or alternative medicine? J Clin Gastroenterol 1994; 19:194-197Google Scholar
34. Vincent C, Furnham A: Why do patients turn to complementary medicine? an empirical study. Br J Clin Psychol 1996; 35:37-48Crossref, Medline, Google Scholar
35. Jonas WB: Alternative medicine—learning from the past, examining the present, advancing to the future (editorial). JAMA 1998; 280:1616-1618Google Scholar
36. Linde K, Ramirez G, Mulrow CD, Pauls A, Weidenhammer W, Melchart D: St John’s wort for depression: an overview and meta-analysis of randomised clinical trials. Br Med J 1996; 313:253-258Crossref, Medline, Google Scholar
37. Mulrow CD, Williams JW Jr, Trivedi M, Chiquette E, Aguilar C, Cornell JE, Badgett R, Noel PH, Lawrence V, Lee S, Luther M, Ramirez G, Richardson WS, Stamm K: Treatment of depression: newer pharmacotherapies. Psychopharmacol Bull 1998; 34:409-795Medline, Google Scholar
38. American Psychiatric Association: Practice Guideline for the Treatment of Patients with Major Depressive Disorder (Revision). Am J Psychiatry 2000; 157(April suppl)Google Scholar



