In This Issue
Switching From Perphenazine to a Newer Antipsychotic
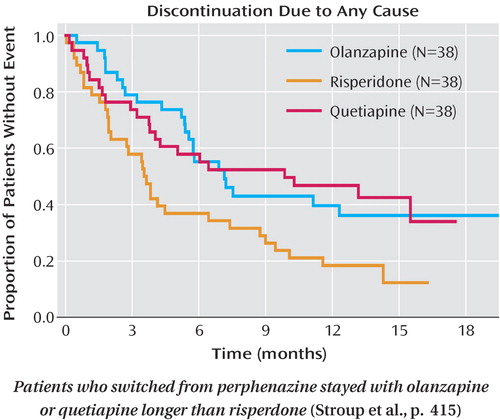
For patients with chronic schizophrenia who switched from perphenazine to a second-generation antipsychotic, quetiapine and olanzapine were more effective than risperidone. In the Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) study, the median time to discontinuation of the second-generation drug was 10 months for quetiapine, 7 months for olanzapine, and 4 months for risperidone. As Stroup et al. (p. Original article: 415 ) report, among patients who had stopped taking perphenazine because of side effects, intolerability led to discontinuation for 60%–70% of the patients taking risperidone or olanzapine but none of those in the quetiapine group. The authors conclude that failure to respond to perphenazine may have identified a subgroup of patients who would not respond to or were intolerant of other potent dopamine D 2 -receptor antagonists. Dr. Stephen Marder, in an editorial on p. Original article: 375 , suggests that subclinical akathisia and bradykinesia contributed to the patients’ poor response to perphenazine.
Functional Outcomes for Schizophrenia Patients
Return of daily living skills is a practical measure of success in treatment of serious mental illness. In phase 1 of the Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) study, three second-generation antipsychotic medications and perphenazine modestly improved psychosocial functioning but did not differ from each other. Swartz et al. (CME, p. Original article: 428 ) examined changes in scores on the Quality of Life Scale, which evaluates social functioning, interpersonal relationships, vocational functioning, and psychological functioning. Perphenazine, olanzapine, ziprasidone, and risperidone produced similar changes, and results were comparable for clozapine in phase 2E. Swartz et al. suggest that more targeted vocational rehabilitative efforts are needed for schizophrenia. As an example, McGurk et al. (p. Original article: 437 ) improved employment outcomes for patients with schizophrenia by adding a cognitive training program to supported employment. The program included cognitive assessment, computer-based training, and ongoing consultation. Over 2–3 years, patients in the combined program had better employment outcomes than those in supported employment only. The average total number of weeks worked was 5.4 for supported employment only but 27.0 weeks for the combined program. An editorial by Dr. John Lauriello on p. Original article: 377 addresses real-world outcomes in schizophrenia.
New Views of Aberrant Brain Processes in Schizophrenia
Six articles in this issue use new brain imaging techniques to identify brain mechanisms that contribute to poor attention and auditory hallucinations in persons with schizophrenia. Functional magnetic resonance imaging (fMRI) enabled Gur et al. (p. Original article: 442 ) to demonstrate that patients’ difficulty in paying attention to visual stimuli is due to both insufficient activation of the brain systems needed for focusing and overactivation of areas that process distractors. Garrity et al. (p. Original article: 450 ) used a similar strategy with targets and distractors, but they used auditory stimuli and measured activation during the baseline auditory condition, the “default mode.” Compared to healthy subjects, patients with schizophrenia had greater temporal fluctuations in this baseline or resting mode. Time-frequency analyses of EEG recordings by Ford et al. (p. Original article: 458 ) indicated that patients with auditory hallucinations were especially likely to have deficient phase synchrony of EEG oscillations before speaking. In healthy people, neural synchrony precedes self-generated speech and inhibits the person from responding to their own voice. High-density EEG applied by Ferrarelli et al. (p. Original article: 483 ) to patients with schizophrenia revealed deficits in sleep spindles, bursts of EEG activity generated by the thalamic reticular nucleus in conjunction with specific thalamic nuclei. Low sleep spindle activity therefore points to dysfunction in mechanisms involving these structures, which are involved in paying attention during waking. Leitman et al. (p. Original article: 474 ) related structural disturbances at the level of the primary auditory cortex to patients’ impaired ability to decode emotions according to voice tone modulation. Brain structure was examined by using diffusion tensor magnetic resonance imaging, which is sensitive to white matter abnormalities in schizophrenia. Diffusion tensor imaging also provided a means for Shergill et al. (p. Original article: 467 ) to examine whether the functional dysconnectivity in schizophrenia is due to disrupted anatomical connectivity. They found abnormalities in the white matter connections of the frontal cortex to the temporal and parietal cortexes and with the contralateral and temporal lobes. However, patients in whom the temporal lobe connections were relatively intact were more likely to have auditory hallucinations. Dr. Robert Freedman comments on these findings in an editorial on p. Original article: 385 .



