In This Issue
A Terrorist Attack’s Physiologic Legacy
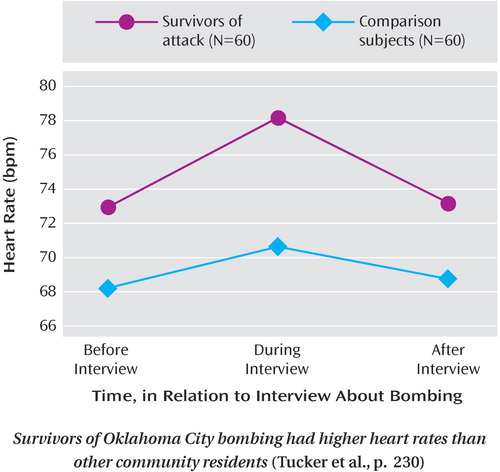
Among people directly exposed to the 1995 Oklahoma City bomb blast, even those without posttraumatic stress disorder (PTSD) show heightened physiologic reactions to reminders of the attack. Tucker et al. (p. Original article: 230 ) found that 60 survivors of the bombing had greater increases in heart rate and blood pressure during interviews about the bombing than Oklahoma City residents who were not closely connected to the explosion. The bombing survivors also had a higher baseline heart rate, and their blood pressure remained elevated after the interview. This sensitivity was independent of PTSD, demonstrating that biological disturbance may persist despite apparent emotional resilience many years after a terrorist attack. Dr. Douglas Delahanty reviews the mental health aspects of terrorist attacks in an editorial on p. Original article: 189 .
Genetics of Mood Disorders
A study of 708 families bolsters evidence that some of the genes conferring susceptibility to bipolar disorder are shared with schizophrenia. Goes et al. (p. Original article: 236 ) found that mood-incongruent psychotic symptoms of bipolar disorder are transmitted within families and are associated with chromosomal regions 13q21-33 and 2p11-q14. The linkage to 13q21-33 supports previous findings of overlap between bipolar disorder and schizophrenia in this region. Until now, 2p11-q14 has been tied to schizophrenia but not bipolar disorder. Dr. Linda Brzustowicz comments on these findings in an editorial on p. Original article: 192 . Holmans et al. (p. Original article: 248 ) discovered an association between recurrent, early-onset depression and chromosomal region 15q25-q26. In addition, the genome scan of 656 families indicated that this disorder is related to chromosomes 17p12 and 8p22-p21.3 in a sex-specific fashion. The families were also tested for known DNA markers within region 15q25-q26, and the results appear in a companion article by Levinson et al. (p. Original article: 259 ). This fine-mapping narrowed down the genetic location that appears to confer susceptibility to depression. This locus could account for up to 25% of the increased risk of recurrent, early-onset depression among siblings of individuals with the same disorder. Dr. Peter McGuffin discusses these findings in an editorial on p. Original article: 195 .
Anxiety at an Early Age
More than half of the adults with anxiety disorders have a childhood history of psychiatric illness, and more than one-third had anxiety disorders at ages 11–15. This continuity emerged from longitudinal assessments of the individuals born during 1972–1973 in Dunedin, New Zealand. Gregory et al. (p. Original article: 301 ) report that among those with anxiety diagnoses at age 32, an early history of depression was also common. For children and adolescents with generalized anxiety disorder, Rynn et al. (p. Original article: 290 ) found that extended-release venlafaxine is an effective treatment. Combined data on 313 participants in two placebo-controlled trials demonstrated that 69% of the venlafaxine patients were greatly improved at the end of 8 weeks, compared to 48% of the placebo patients. The improvements occurred in both children (ages 6–11) and adolescents (ages 12–17). The venlafaxine and placebo groups each had one case of suicidal thoughts or attempts. Extended-release venlafaxine had effects on weight, height, cholesterol level, heart rate, and blood pressure.
Psychoanalytic Therapy for Panic Disorder
Medication and cognitive behavior therapy (CBT) are the most common treatments for panic disorder. Brief psychodynamic psychotherapy may offer a third option. Milrod et al. (p. Original article: 265 ) report a 12-week randomized trial comparing a panic-focused psychodynamic intervention with relaxation training for patients with panic disorder. The response rate for psychodynamic psychotherapy was 73%, compared to 39% for relaxation training. The dropout rates differed as well—7% versus 34%. Response was unrelated to concurrent psychotropic medications. Panic-focused psychodynamic psychotherapy could be valuable when medication or CBT is inappropriate or when neither leads to response.



