Dimensions of Personality Pathology: An Alternative to the Five-Factor Model
Abstract
OBJECTIVE: Researchers have advocated replacing the DSM-IV classification of personality disorders with an alternative diagnostic system based on the five-factor model. This study evaluates the clinical comprehensiveness of the five-factor model and addresses the broader question of how many factors, and which factors, are necessary to understand personality pathology. METHOD: A national sample of 530 psychiatrists and clinical psychologists used the Shedler-Westen Assessment Procedure (SWAP-200) to provide detailed psychological descriptions of patients with personality disorder diagnoses. The SWAP-200 is a 200-item instrument designed to capture the richness and complexity of clinical observations while also providing quantifiable data for research. We used factor analysis to identify dimensions of personality relevant to understanding personality pathology. RESULTS: The five-factor structure replicated in a content-restricted subset of 60 SWAP-200 items. However, factor analysis of the full SWAP-200 yielded a conceptually richer factor solution that did not resemble the five-factor model. The analysis identified 12 clinically relevant personality dimensions labeled psychological health, psychopathy, hostility, narcissism, emotional dysregulation, dysphoria, schizoid orientation, obsessionality, thought disorder, oedipal conflict (histrionic sexualization), dissociation, and sexual conflict. CONCLUSIONS: The five-factor model represents a sound distillation of the personality constructs used by laypersons. However, it omits key clinical constructs and may not capture the complexity of personality syndromes seen in clinical practice. The SWAP-200 factors may provide a framework for studying personality pathology that is both empirically grounded and clinically relevant.
Researchers are evaluating a range of alternatives to the personality disorder classification system provided by DSM-IV. Many advocate replacing the current categorical approach (in which personality disorders are diagnosed as present or absent) with a dimensional approach, which would treat personality traits as continua (1–3). Proponents of dimensional approaches point out that personality traits are normally distributed in nature, so categorical diagnosis imposes arbitrary dichotomies; that categorical diagnosis implies a discontinuity between normal and pathological personality, whereas dimensional approaches help integrate the understanding of normal and pathological personality; that dimensional variables have psychometric advantages and lend themselves more readily to statistical analysis, including measurement of change; and that the important dimensions of personality can be established empirically by means of factor analysis rather than by committee decision (1–3).
In particular, researchers have proposed replacing axis II with a dimensional system based on the five-factor model of personality (4). The five-factor model conceptualizes personality in terms of five basic dimensions or traits. This article examines the clinical relevance of the five-factor model and compares it to an alternative dimensional model derived from the Shedler-Westen Assessment Procedure (SWAP-200), an instrument designed to quantify the observations of experienced clinical observers. More broadly, this article addresses the questions of how many factors, and which factors, are necessary for understanding personality pathology.
Overview of the Five-Factor Model
The five-factor model reflects over four decades of research by academic psychologists. In the late 1950s and early 1960s, researchers asked volunteer (nonclinical) subjects to rate the personality traits of their peers using lists of adjectives from Webster’s unabridged dictionary (5). Factor analysis of the ratings yielded five factors or dimensions that accounted for much of the underlying variance (6–8). Over the ensuing decades, the five factors emerged reliably in factor analysis of self-rating and peer-rating data (e.g., references 9–12). The factors have commonly been labeled neuroticism, extroversion, agreeableness, conscientiousness, and openness to experience. Each label refers to one pole of a bipolar dimension (e.g., the opposite pole of extroversion is introversion).
Proponents argue that the five-factor model captures the essential features of personality and that any personality construct can ultimately be mapped onto the factors (11–14). Some maintain that the factors constitute the “universal structure” of human personality (13). This assertion rests on the lexical hypothesis that language evolves over time to describe what is important. According to this hypothesis, meaningful traits on which people differ will be represented in the natural language and can be identified through factor analysis of everyday terms. Indeed, the five-factor model has proven remarkably generative. It appears cross-culturally relevant (e.g., references 12, 15, 16), has proven valuable in studying consistency and change in personality over time (e.g., reference 11), and has been applied successfully in research on the heritability of personality traits (10, 17).
From a five-factor perspective, personality disorders are simply extreme variants of normal personality traits (4). Thus, five-factor model researchers have conceptualized histrionic personality disorder in terms of excessive extroversion, and antisocial personality disorder as a combination of low agreeableness and low conscientiousness (18). Because analysis at the level of five factors often lacks the specificity to characterize complex personality disorders, researchers have moved a level down the factor hierarchy to subfactors or “facets” of the five factors (18). Thus, the most widely used five-factor model inventory (the revised NEO Personality Inventory [19]) includes neuroticism subscales of anxiety, hostility, depression, self-consciousness, impulsiveness, and vulnerability. A patient with borderline personality disorder would be high on all facets, whereas a patient with avoidant personality disorder would be high on anxiety and self-consciousness but low on impulsivity and hostility.
Is the Five-Factor Model Clinically Relevant?
Critics have questioned the clinical relevance of the five-factor model (20–24). One concern is that factor analytic findings depend on the items included in the analysis. The five-factor model derives from factor analysis of adjectives, but lists of adjectives may be inadequate for describing the complexities of personality. Phrases, whole sentences, and occasionally even paragraphs may be necessary (20). Restricting attention to what can be described with lists of adjectives seems a significant handicap when describing complex psychological processes.
A related concern is that the five-factor model is too superficial for clinical (versus lay) personality description. One researcher characterized it as describing the “psychology of the stranger” (21), that is, the way a person appears to another after a casual encounter (e.g., gregarious, hostile, modest). Others have noted that everyday language may not be differentiated enough for scientific and clinical purposes (20, 23, 25).
The five-factor model derives from self-ratings and peer ratings provided by laypersons, not psychological assessments provided by psychiatrists and psychologists. However, lay observers may have limited exposure to the kinds of personality pathology that mental health professionals encounter daily. Further, the sophistication of a personality theory generated by this method can be no greater than that of the average person who contributes ratings. Thus, the five-factor model unavoidably reduces personality description to the lowest common denominator, implicitly denying differences in knowledge and understanding between professionals and laypersons.
Five-factor model research has relied heavily on self-report instruments that assume people report accurately on their own personalities. However, research by Shedler et al. (26) on “illusory mental health” demonstrates that self-report scales cannot distinguish between psychologically healthy individuals and emotionally disturbed individuals who lack self-awareness. Other research demonstrates that important cognitive, affective, and motivational processes (i.e., personality processes) may be implicit rather than explicit and not accessible by self-report (e.g., references 27, 28). The problems inherent in self-report instruments may be amplified for patients with personality disorders, for whom lack of insight and self-awareness is often diagnostic.
Researchers have made the five-factor model more useful for describing personality disorders by focusing on subfactors or “facets” of the factors. However, this is no longer the five-factor model that has been so well validated and replicated, and investigators can no longer claim the same advantages of universality, reproducibility, and cross-cultural relevance.
Finally, the five-factor model focuses on behavioral tendencies (e.g., extroversion) and relatively obvious internal states (e.g., depression) but not on the psychological processes that are the focus of much clinical work. For example, it is common in clinical practice to encounter patients who are angry but also inhibited about experiencing and expressing anger. A moderate score on an anger dimension would not differentiate between individuals who are conflicted about anger expression and those who truly have a moderate level of the trait. Similarly, narcissistic patients may have both feelings of inflated self-worth and feelings of inadequacy. A moderate score on a “modesty” dimension would not convey the nature of the narcissistic dilemma.
Rationale and Overview
The five-factor model represents an important distillation of the personality constructs used by laypeople and reflected in everyday language. Whether it is comprehensive enough to describe personality disorders, or provides a “language” sophisticated enough to encompass the constructs salient to clinical (as opposed to lay) personality assessors are open questions. To address these questions, we collected personality assessment data in a sample of 530 psychotherapy patients receiving treatment for personality disorders and factor-analyzed the set of personality-descriptive statements provided by the SWAP-200 (29–31). The SWAP-200 differs from five-factor model instruments in that it 1) samples from the domain of personality constructs used by clinical practitioners rather than adjectives from the dictionary (including, but not limited to, axis II criteria); 2) relies on expert observers, not laypersons, as personality assessors; and 3) includes items that address internal psychological processes (e.g., ways of experiencing the self, others, and relationships; motives and conflicts; affect regulation strategies or defenses) that are absent from five-factor-model instruments but that most clinicians consider important.
We performed two factor analyses. First, we selected a subset of 60 items from the SWAP-200 with face content that mapped readily onto any of the five five-factor model factors or facets (32) and factor-analyzed this content-restricted item set. Next, we factor-analyzed the full SWAP-200. We reasoned that if the five-factor model is indeed a comprehensive system for assessing personality and personality pathology, then a factor structure resembling the five-factor model should emerge in both factor analyses. If, on the other hand, reproduction of the five-factor model depends on the use of a content-restricted item set (derived from, and designed for, lay personality description), then the five factors should emerge only in the 60-item factor analysis but not in the 200-item factor analysis.
This study is not intended to compare the validity or utility of the SWAP-200 versus the five-factor model. Such a comparison would require administering the SWAP-200 and a five-factor instrument in the same sample and examining relations with a broad range of relevant criterion variables. We are suggesting only that failure to replicate the five-factor model in this clinical sample should raise questions about its comprehensiveness for assessing personality pathology, especially if factor analysis of the SWAP-200 identifies important personality constructs absent from the five-factor model.
The SWAP-200: Quantifying Clinical Judgment
The SWAP-200 is a set of 200 personality-descriptive statements, each printed on a separate index card (29–31, 33). To describe a patient using the SWAP-200, a clinician arranges the items into eight categories from those that are not descriptive of the patient (assigned a value of 0) to those that are highly descriptive (assigned a value of 7). Thus, the procedure yields a numeric score from 0 to 7 for each of 200 personality-descriptive variables. An interactive, web-based version of the instrument is also available. (The web-based version of the SWAP-200 can be viewed at www.psychsystems.net/guest.cfm.) The SWAP-200 is based on the Q-sort method, which requires clinicians to arrange the items into a fixed distribution. This method has psychometric advantages that have been described in detail elsewhere (34).
SWAP-200 items are written in straightforward, experience-near language (e.g., “Tends to be passive and unassertive” or “Has an exaggerated sense of self-importance”), and statements that require inferences about internal psychological processes are written in simple English, not jargon (e.g., “Tends to see own unacceptable feelings or impulses in other people instead of in him/herself”). In prior studies, interrater reliability of the SWAP-200 has ranged from 0.75 to 0.89 (e.g., references 29, 35; Marin-Avellan et al., 2004, unpublished manuscript), and scores derived from the SWAP-200 correlate with a range of criterion measures in both adult and adolescent samples (e.g., references 35–37).
The SWAP-200 item set was developed and revised over a 7-year period (see reference 29) and incorporates constructs from a wide variety of sources, including axis II diagnostic criteria included in DSM-III through DSM-IV, selected axis I criteria that could reflect personality traits (such as depression and anxiety), research in personality psychology (including research on the five-factor model), and the clinical literature on personality disorders written over the past 50 years (e.g., references 38–40).
Most important, the SWAP-200 is the product of an iterative revision process that incorporated the feedback of hundreds of clinicians who used the instrument to describe their patients. Each time a clinician used the instrument, we asked one crucial question: “Were you able to describe the things you consider psychologically important about your patient?” We added, edited, rewrote, and revised items based on this feedback, then asked new clinicians to describe new patients. We repeated this process over many iterations until most clinicians could answer “yes” most of the time.
Method
The data collection methods have been described elsewhere (30); here we summarize the procedures relevant to the present study. A national sample of 530 board-certified psychiatrists and licensed clinical psychologists contributed data to the study. These clinicians were recruited from the rosters of the American Psychiatric Association and the American Psychological Association. We initially surveyed the clinicians to determine which personality disorders were represented in their practices. We then randomly assigned a specific personality disorder for each clinician to describe (with the constraint that the personality disorder was represented in the clinician’s practice). Each clinician used the SWAP-200 to describe a current patient with a specified personality disorder. The clinicians also rated the extent to which the patient met criteria for each personality disorder included in DSM-IV (7-point rating scale; 1=not at all, 7=fully meets criteria).
Results
Characteristics of Clinicians
The participating clinicians had an average of 18.4 years (SD=9.8) practice experience posttraining. Approximately one-third were psychiatrists and two-thirds were psychologists; 64% were men. They tended to have multiple institutional affiliations: 31% worked in hospitals at least part-time, 20% worked in clinics, 82% maintained private practices, and 11% worked in forensic settings. Two percent described their primary theoretical orientation as systemic, 4.8% as biological, 14.4% as cognitive behavior, 29.4% as eclectic, and 48.6% as psychodynamic.
Characteristics of Patients
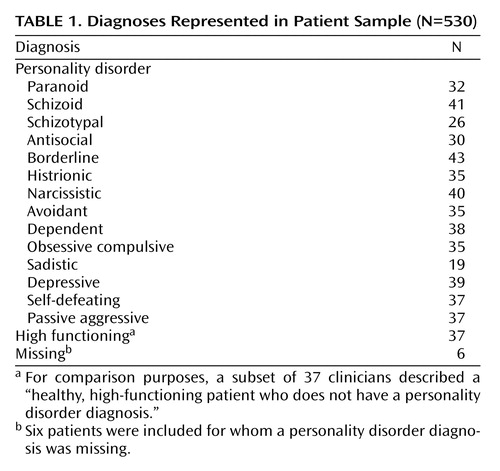
The sample included patients with all personality disorders recognized by DSM-III through DSM-IV as well as personality disorders described in the DSM appendices (30). Table 1 lists the included personality disorders and associated numbers of subjects. The median length of treatment before completion of the SWAP-200 was 24 sessions, so the patients were well known to the reporting clinicians. The patients were 53.1% women and 46.9% men, with a mean age of 40.9 (SD=11.6). The mean Global Assessment of Functioning Scale score was 61.8 (SD=13.6), within the expected range for an outpatient sample with personality pathology.
Replicating the Five-Factor Model
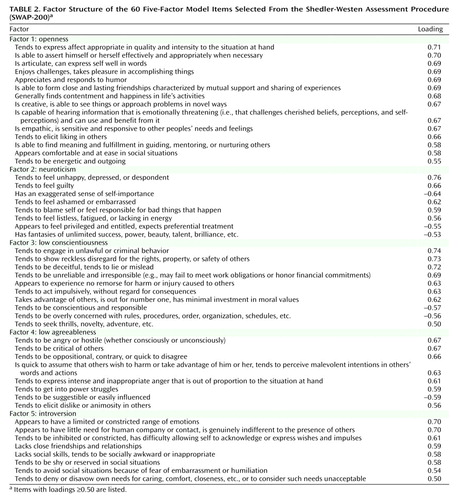
Through item inspection, we identified a subset of 60 SWAP-200 items with content that mapped directly onto five-factor model factors and facets, and subjected these items to a principal-component analysis. There was a clear break in the scree plot between the fifth and sixth principal components, supporting a five-factor solution. Therefore, we retained and varimax-rotated five factors, which cumulatively accounted for approximately half (49.25%) of the variance in the 60-item set.
The rotated factors were remarkably similar to those of the five-factor model (Table 2). Only the openness factor (called by some researchers “culture” or “intellect”) left questions as to interpretation, as it included items related to general psychological health. Openness has been the least consistent and interpretable dimension in previous five-factor model research (13) and is least relevant to psychopathology (and hence is least represented in the SWAP-200). The remaining four factors were unambiguous: neuroticism, low conscientiousness, low agreeableness, and introversion.
Factor Structure of the SWAP-200
We conducted a second factor analysis using the entire 200 items contained in the SWAP-200. The items were subjected to principal-component analysis. We examined the resulting eigenvalues, the percent of variance accounted for by each principal component, and the scree plot. The scree plot showed no clear break, with a gradual leveling between 10 and 20 factors. (This relatively large number of factors is consistent with the findings of Clark and colleagues, who used self-report instruments designed for personality disorder samples [3, 41].) Seventeen of the principal components cumulatively accounted for approximately half (50.2%) of the variance in the item set. Thus, we retained and varimax-rotated 17 factors. The first 12 of the rotated factors proved theoretically coherent, readily interpretable, and well marked by multiple items.
(Eigenvalues for the first 12 principal components ranged from 2.7 to 23.9, accounting for 1.35% to 11.95% of the variance each. Scale reliabilities [coefficient alpha] for the 12 rotated factors ranged from a high of 0.94 [factor I] to a low of 0.59 [factor 10], with all other scales showing reliability >0.70.)
To verify the stability of the 12 factors, we performed additional factor analyses specifying fewer factors and more factors and consistently obtained similar factor solutions. We also performed a second factor analysis using oblique (promax) rotation. The results of the two approaches were virtually identical; for ease of presentation, we report results based on orthogonal rotation. Table 3 lists the items that load most highly on each of the 12 factors in descending order of factor loading. There appears to be little question about the interpretation of any of the factors.
Factor 1, psychological health, assesses the positive presence of psychological strengths and inner resources, including the capacity to love, find meaning in life experiences, and gain insight into self and others.
Factor 2, psychopathy, includes features associated not only with antisocial personality disorder but also with the classical clinical construct of psychopathy (42, 43), such as lack of remorse, a seeming imperviousness to consequences, impulsivity, and a tendency to abuse alcohol and drugs.
Factor 3, hostility, is straightforward and requires no interpretation. It resembles the five-factor model neuroticism facet of the same name.
Factor 4, narcissism, reflects self-importance, grandiosity, entitlement, and the tendency to treat others as audiences to provide admiration. The factor taps a core construct in contemporary clinical thought.
Factor 5, emotional dysregulation, refers to a deficiency in the capacity to modulate and regulate affect, so that affect tends to spiral out of control, change rapidly, get expressed in intense and unmodified form, and overwhelm reasoning. This construct is crucial to an understanding of borderline personality disorder and has no five-factor model equivalent.
Factor 6, dysphoria, captures depression, anhedonia, shame, humiliation, and a number of their cognitive and affective correlates. The factor is closely related to the five-factor model neuroticism factor.
Factor 7, schizoid orientation, bears a family resemblance to the extreme negative pole of extroversion, but a review of the items shows this to be a distinct and clinically richer construct. Patients high on this dimension do not just keep to themselves. They are also concrete in their thinking, barren in their representations of others (as reflected by an inability to describe others in meaningful ways), have constricted emotions, and have little capacity for empathy. In contrast, many introverts are reflective about themselves and others, feel emotion intensely, and are sophisticated and abstract in their thinking.
Factor 8, obsessionality, bears a family resemblance to the five-factor model conscientiousness factor. Note, however, that the obsessionality factor describes not only hyperconscientiousness but a cognitive and defensive style that includes absorption in details, intellectualization, preoccupation with dirt and contamination, intrusive and obsessional thoughts, stinginess, and difficulty discarding things. It appears related to the historical construct of obsessionality (see references 44, 45).
Factor 9, thought disorder (or schizotypy), captures a phenomenon of crucial clinical import that has no five-factor model equivalent (as acknowledged by McCrae [46]). (With respect to research on psychotic spectrum disorders, this factor appears to assess characterological and subsyndromal positive symptoms; the schizoid orientation factor appears to assess subsyndromal negative symptoms.)
Factor 10, oedipal conflict, includes a constellation of items reflecting triangulated romantic relationships that always involve a third-party competitor, choosing romantic partners who are unavailable or inappropriate, sexual jealousy, and excessive or inappropriate seductiveness. Some readers may prefer the label “histrionic sexualization.” Regardless of one’s preferred terminology, the factor captures an important clinical phenomenon with no five-factor model equivalent.
Factor 11, dissociation, describes incongruity and disconnectedness between affect, cognition, and memory that is often associated with a developmental history of trauma or abuse. This construct is of crucial clinical import, especially for individuals who have been victims of complex trauma and for many patients diagnosed with borderline personality pathology. The construct has no five-factor-model equivalent.
Factor 12, sexual conflict, describes a conflicted orientation toward sexuality, including the association of sexuality with danger (whether consciously or unconsciously), and guilt, shame, revulsion, or disgust in connection with sexuality. The factor is not represented in the five-factor model. From a clinical perspective, the absence of items to assess sexuality is a particularly salient omission in the five-factor model. It is also a significant omission from the perspective of evolutionary psychology.
Ruling Out Alternative Hypotheses
A critic might argue that the 12-factor solution reflects not so much the personalities of the patients but rather the shared cognitive schemas of the clinicians who provided the data. In this case, the factor solution would reveal more about the beliefs of clinicians than the characteristics of their patients (this same criticism has been directed against the five-factor model itself [47, 48]).
The strongest version of the “cognitive schema” argument might run as follows. Nearly half of the participating clinicians reported a psychodynamic orientation. Could the factor solution therefore be a function of their shared theories?
To explore this rival hypothesis, we eliminated clinicians from the data set who identified their orientation as psychodynamic and reanalyzed the SWAP-200 data contributed by the remaining 257 nonpsychodynamic clinicians. The factor solution was virtually identical; the only substantive difference was that the 12th factor became a self-destructive factor and the sexual conflict items loaded on a 13th factor.
Another possibility is that the 12 SWAP factors are lower-level facets of the five-factor-model factors. If so, the factors could themselves be factor-analyzed, and the resulting higher-order factors should resemble the five-factor model. To explore this, we subjected the SWAP-200 factors to higher-order factor analysis using the strategy adopted by Clark, Livesley, and colleagues (49). We first created variables to represent each factor by averaging items with loadings of 0.50 or higher (or above 0.35–0.40 if fewer than eight items had loadings >0.50). We then factor-analyzed these 12 variables. The resulting scree plot showed no clear break. We nevertheless retained and varimax-rotated five factors.
The five-factor solution did not yield higher-order factors that were easily interpretable, and the factors did not resemble the five-factor model. The first higher-order factor was marked by schizoid orientation, dissociation, and psychological health (negative loading); the underlying construct is not readily apparent. The second higher-order factor was marked by narcissism, dysphoria (negative loading), and psychopathy; again, the underlying construct is not readily apparent, although one might stretch to label it malignant narcissism. The third higher-order factor was marked by one variable: obsessionality (which has often loaded on its own factor in prior research factoring axis II criteria, e.g., reference 50). The fourth higher factor was marked by sexual conflict and oedipal conflict and hence might be labeled problematic sexuality. The fifth higher-order factor was marked by emotional dysregulation and hostility; again, the underlying construct is difficult to discern, although it may reflect borderline affectivity.
The higher-order factors lack theoretical coherence and appear to bring less rather than more order to the data. We performed additional higher-order factor analyses, retaining and rotating three, four, and six higher-order factors, using both orthogonal and oblique rotations, but failed to find higher-order factors that resembled five-factor model factors.
Convergent and Discriminant Validity
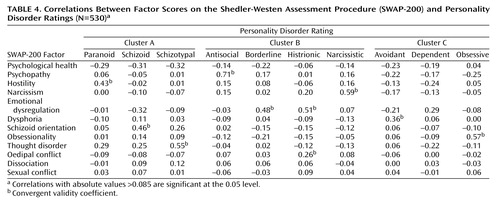
As an initial step in locating the 12 SWAP-200 factors in a conceptually meaningful nomological network (establishing construct validity), we examined their relations with dimensional measures of the current axis II personality disorders. The reporting clinicians rated the extent to which patients met DSM-IV criteria for each axis II disorder using a 7-point rating scale (1=not at all, 4=has some features, 7=fully meets criteria). Table 4 presents correlations between the SWAP-200 factors and these personality disorder ratings. The SWAP-200 factors are clearly predictive where they should be and not predictive where they should not be, indicating strong convergent and discriminant validity. Predicted positive correlations (convergent validity coefficients) are noted.
The following findings are especially pertinent:
| 1. | Correlations between SWAP-200 factor scores and related personality disorders (e.g., between psychopathy [factor 2] and antisocial personality disorder) were uniformly high, and correlations with unrelated personality disorders hovered near zero. This is striking given the generally poor discriminant validity (high comorbidity) of axis II personality disorder diagnoses (51, 52). | ||||
| 2. | Emotional dysregulation (factor 5) correlated with borderline and histrionic personality disorders but not with depressive, dependent, or avoidant personality disorders. This suggests that emotional dysregulation and dysphoria (“neuroticism” in the five-factor model) are separate and distinct constructs (see also references 53, 54). | ||||
| 3. | Schizoid orientation (factor 7) was related to both schizoid personality disorder and secondarily to schizotypal personality disorder but not to avoidant personality disorder. This is important because prior empirical studies have had difficulty distinguishing between schizoid and avoidant personality disorders, and comorbidity between the disorders is often above 50% (see reference 25). Additionally, both schizoid and avoidant personality disorders are candidates for the extreme negative pole of extroversion, yet the schizoid factor correlated with only one of them. | ||||
| 4. | Thought disorder (factor 9) distinguished schizotypal personality disorder from all other personality disorders, even schizoid and borderline. In contrast, previous empirical studies have found high comorbidities between schizotypal, schizoid, and borderline personality disorders (see reference 55). | ||||
Discussion
The SWAP-200 factors provide a more differentiated description of personality than the five-factor model in a sample of patients diagnosed with personality pathology. For example, it differentiates between dysphoria and emotional dysregulation, a distinction that has great clinical import. Many clinical syndromes are associated with dysphoria (or negative affectivity), but the affective lability or dyscontrol captured by the emotional dysregulation factor appears unique to patients with borderline and histrionic personality disorders (and has emerged in other item sets designed to assess the spectrum of normal and pathological personality) (41, 56).
The SWAP-200 factor structure differentiates between hostility, psychopathy, and narcissism, whereas the five-factor model attempts to capture these phenomena through various combinations of low agreeableness and low conscientiousness. Whereas five-factor model researchers have explained obsessional personality disorder as extreme conscientiousness, the SWAP-200 obsessionality factor includes many elements not accounted for by conscientiousness. Patients high on this dimension were not only conscientious but were also affectively constricted and intellectualized, stingy, and concerned about dirt and contamination. They manifested other traits associated with historical descriptions of obsessional character organization (see, e.g., references 44, 45, 57).
The emergence of thought disorder, oedipal conflict, and sexual conflict factors is especially noteworthy and further highlights the clinical limitations of the five-factor model. Thought disorder is a crucial psychological construct relevant to personality pathology that could not have been anticipated in the development of five-factor model instruments in nonclinical samples. The absence in the five-factor model of such an important dimension as sexuality also speaks to its limitations as a comprehensive model of personality, from both a clinical and an evolutionary standpoint.
Potential Objections
Several objections could be raised to this study, of which two are most important. First, a critic might argue that the factor analytic results are an artifact of an idiosyncratic item set that does not include the “right” items. The steps taken to develop the SWAP-200 item set should minimize this concern. The item set includes multiple markers of the five-factor factors and does indeed allow us to recover a five-factor solution using a large subset of the items. In addition to sampling from the universe of personality descriptors contained in everyday language, the SWAP-200 reflects an effort to sample in a systematic way from the universe of personality descriptors used by professionals who treat personality pathology (without resorting to jargon that would limit its reliability and usefulness). Thus, the item set includes 80-plus personality descriptors that reflect the consensus of the framers of the DSM over three successive editions regarding the variables necessary for describing personality pathology, plus over 100 additional items reflecting the feedback of hundreds of clinicians who used earlier versions of the SWAP to describe their patients. We also followed generally accepted psychometric practices to minimize redundancy of item content (e.g., eliminating or rewriting items that were highly correlated) that could lead to artifactual factors.
A second potential objection is that the factor structure reflects clinicians’ biases. This argument runs as follows: psychiatrists and clinical psychologists are so moored in theory and diagnostic categories that their descriptions are inherently biased, suspect, and invalid (i.e., they describe their theories rather than their patients). Although confirmation biases are real and can influence both expert and lay observations, this is an argument that we do not generally apply in other branches of science or medicine. Few would argue, for example, that radiologists are less qualified to read X-rays than their patients because they have too many preconceived ideas based on training and experience. The argument smacks of an anticlinical bias and implies that the cumulative insights of generations of professionals have less evidential value than the casual observations of laypeople.
Anticlinical biases notwithstanding, a number of considerations should minimize this concern. First, we were able to replicate the five-factor model factor structure in a subset of items that tapped constructs relevant to the five-factor model. Since most clinical practitioners are unfamiliar with the five-factor model, this suggests that they were indeed describing their patients and not their theories. Second, the 12 SWAP-200 factors emerged when we stratified the sample by clinicians’ theoretical orientation (the finding is consistent with earlier data showing minimal differences between cognitive behavioral and psychodynamic clinicians, despite considerable differences in theory and training [29]). Third, the 12-factor solution did not simply reproduce axis II diagnoses, even though the research design arguably pulled for this (because we asked clinicians to describe patients with specific axis II diagnoses). Finally, clinician bias cannot account for the theoretically coherent pattern of correlations between SWAP-200 factors and personality disorder ratings. It is implausible to imagine that instead of describing their patients, clinicians were juggling 10 diagnostic prototypes (axis II diagnoses) in their minds while simultaneously trying to sort 200 items (see reference 30 for a more detailed discussion).
Applying the Lexical Hypothesis to Personality Disorders
Ultimately, the five-factor model is a model of personality derived from the constructs and observations of laypeople, and it provides an excellent map of the domains of personality to which the average layperson attends. However, the present findings suggest that the five-factor model is not sufficiently comprehensive for describing personality disorders or sophisticated enough for clinical purposes.
In contrast to laypeople, practicing clinicians devote their professional lives to understanding the intricacies of personality. They develop intimate knowledge of others’ lives and inner experience in ways that may not be possible in everyday social interaction. Moreover, they treat patients with variants of personality pathology that laypeople encounter only infrequently (and are likely to avoid when they do encounter it). One would therefore expect expert clinicians to develop constructs more differentiated than those of lay observers.
Indeed, if this were not true, it would violate the lexical hypothesis on which the five-factor model rests: that language evolves over time to reflect what is important. To the extent that mental health professionals observe personality with particular goals and expertise, and observe the more pathological end of the personality spectrum, the constructs they consider important should differ from those of the average layperson.
Implications for the Classification of Personality Disorders
There is considerable ferment in personality disorder circles regarding the best way to reconfigure axis II for DSM-V. A consensus is emerging that the basic framework laid down in DSM-III and revised over subsequent editions has been fruitful in generating a rich empirical literature, but that 25 years and hundreds of studies later, the framework needs reworking. Virtually all the major alternatives are dimensional, with most focusing on factor-analytically derived personality traits rather than the multifaceted constellations of traits (personality types) historically connoted by the term “personality disorder.” The major question has been how to identify the optimal traits or dimensions. (Elsewhere we have proposed a “prototype matching” approach that preserves the concept of personality types and also permits dimensional diagnosis; see reference 58.)
Most of the proposed dimensional approaches derive from factor analysis of self-report questionnaires. As we have argued elsewhere, self-report data have significant limitations in clinical contexts, especially with respect to assessing personality disorders (26, 30, 53). We believe that the most useful trait approaches to personality disorders will be those derived from item sets designed explicitly to 1) tap constructs considered useful by clinicians who treat personality pathology and 2) assess pathological personality processes in addition to traits observed by laypeople in everyday social interaction.
Finally, future revisions of axis II will need to balance empirical considerations with clinical utility. It is not sufficient for a diagnostic system to be empirically elegant; it must encompass the spectrum of personality pathology clinicians see in real-world practice, it must be practical to apply in the clinic as well as the laboratory, and, ideally, it should help guide therapeutic intervention. Ultimately, the most empirically elegant classification system will have little impact on clinical practice if clinicians do not find it helpful for understanding their patients.
 |
 |
 |
 |
Received Oct. 17, 2002; revisions received May 29, July 1, and July 29, 2003; accepted Nov. 11, 2003. From the University of Denver; and Emory University. Address reprint requests to Dr. Shedler, Graduate School of Professional Psychology, University of Denver, 2450 South Vine St., Denver, CO 80208; [email protected] (e-mail); or to Dr. Westen, Departments of Psychology and Psychiatry and Behavioral Sciences, Emory University, 532 Kilgo Cir., Atlanta, GA 30309; [email protected] (e-mail). Supported in part by NIMH grants MH-62377 and MH-62378. The authors thank the more than 950 clinicians who helped refine the SWAP-200 assessment instrument, including the 530 who contributed data to the present study; their research assistants, Michelle Levine, Alan Reyes, Lisa Goldstein, Melanie Glickson, Elizabeth Schafer, and Angela Emerick; and Drs. Laura Arkowitz Westen and Lee Anna Clark for their comments on an earlier draft of this article.
1. Frances A: Categorical and dimensional systems of personality diagnosis: a comparison. Compr Psychiatry 1982; 23:516–527Crossref, Medline, Google Scholar
2. Widiger T: Categorical versus dimensional classification: implications from and for research. J Personal Disord 1992; 6:287–300Crossref, Google Scholar
3. Clark LA, Livesley WJ, Morey L: Personality disorder assessment: the challenge of construct validity. J Personal Disord 1997; 11:205–231Crossref, Medline, Google Scholar
4. Widiger T, Frances A: Towards a dimensional model for the personality disorders, in Personality Disorders and the Five Factor Model of Personality. Edited by Costa P, Widiger T. Washington, DC, American Psychological Association, 1994, pp 19–39Google Scholar
5. Allport G, Odbert H: Trait names: a psycho-lexical study. Psychol Monogr 1936; 47(1)Google Scholar
6. Norman WT: Toward an adequate taxonomy of personality attributes: replicated factor structure in peer nomination personality ratings. J Abnorm Soc Psychol 1963; 66:574–583Crossref, Medline, Google Scholar
7. Norman WT, Goldberg LR: Raters, ratees, and randomness in personality structure. J Pers Soc Psychol 1966; 4:681–691Crossref, Google Scholar
8. Tupes EC, Christal RE: Stability of Personality Trait Rating Factors Obtained Under Diverse Conditions: USAF WADC Technical Note 59–198. Dayton, Ohio, Wright Air Development Center, 1958Google Scholar
9. Digman J: The curious history of the five-factor model, in The Five-Factor Model of Personality. Edited by Wiggins JS. New York, Guilford, 1996, pp 1–20Google Scholar
10. John O: The big five factor taxonomy: dimensions of personality in the natural language and in questionnaires, in Handbook of Personality: Theory and Research. Edited by Pervin L. New York, Guilford, 1990, pp 66–100Google Scholar
11. McCrae R, Costa P: Personality in Adulthood. New York, Guilford, 1990Google Scholar
12. McCrae R, Costa PL: Personality trait structure as a human universal. Am Psychol 1997; 52:509–516Crossref, Medline, Google Scholar
13. Goldberg L: The structure of phenotypic personality traits. Am Psychol 1993; 48:26–34Crossref, Medline, Google Scholar
14. Goldberg LR, Rosolack TK: The big five factor structure as an integrative framework: an empirical comparison with Eysenck’s P-E-N model, in The Developing Structure of Temperament and Personality From Infancy to Adulthood. Edited by Halverson CF, Kohnstamm GA, Martin RP. Hillsdale, NJ, Lawrence Erlbaum Associates, 1994, pp 7–35Google Scholar
15. Kuo-shu Y, Bond MH: Exploring implicit personality theories with indigenous or imported constructs: the Chinese case. J Pers Soc Psychol 1990; 58:1087–1095Crossref, Medline, Google Scholar
16. Stumpf H: The factor structure of the Personality Research Form: a cross-national evaluation. J Pers 1993; 61:1–26Crossref, Google Scholar
17. Plomin R, DeFries JC, McClearn G, Rutter M: Behavioral Genetics. New York, WH Freeman, 1997Google Scholar
18. Widiger T, Trull T, Clarkin J, Sanderson CJ, Costa P: A description of the DSM-III-R and DSM-IV personality disorders with the five-factor model of personality, in Personality Disorders and the Five Factor Model of Personality. Edited by Costa P, Widiger T. Washington, DC, American Psychological Association, 1994, pp 41–56Google Scholar
19. Costa PL, McCrae RR: Revised NEO Personality Inventory (NEO-PI-R) and NEO Five Factor Inventory (NEO-FFI) Professional Manual. Odessa, Fla, Psychological Assessment Resources, 1992Google Scholar
20. Block J: A contrarian view of the five-factor approach to personality descriptions. Psychol Bull 1995; 117:187–215Crossref, Medline, Google Scholar
21. McAdams D: The five-factor model in personality: a critical appraisal. J Pers 1992; 60:329–361Crossref, Medline, Google Scholar
22. Pervin L: A critical analysis of current trait theory. Psychol Inquiry 1994; 5:103–113Crossref, Google Scholar
23. Westen D: A clinical-empirical model of personality: life after the Mischelian ice age and the NEO-lithic era. J Pers 1995; 63:495–524Crossref, Medline, Google Scholar
24. Westen D: A model and a method for uncovering the nomothetic from the idiographic: an alternative to the five-factor model? J Res Pers 1996; 30:400–413Crossref, Google Scholar
25. Millon T, Martinez A: Avoidant personality disorder, in The DSM-IV Personality Disorders. Edited by Livesley WJ. New York, Guilford, 1995, pp 218–233Google Scholar
26. Shedler J, Mayman M, Manis M: The illusion of mental health. Am Psychol 1993; 48:1117–1131Crossref, Medline, Google Scholar
27. Nisbett RE, Wilson TD: Telling more than we can know: verbal reports on mental processes. Psychol Rev 1977; 84:231–259Crossref, Google Scholar
28. Westen D: The scientific legacy of Sigmund Freud: toward a psychodynamically informed psychological science. Psychol Bull 1998; 124:333–371Crossref, Google Scholar
29. Shedler J, Westen D: Refining the measurement of axis II: a Q-sort procedure for assessing personality pathology. Assessment 1998; 5:333–353Crossref, Medline, Google Scholar
30. Westen D, Shedler J: Revising and assessing axis II, part I: developing a clinically and empirically valid assessment method. Am J Psychiatry 1999; 156:258–272Abstract, Google Scholar
31. Westen D, Shedler J: Revising and assessing axis II, part II: toward an empirically based and clinically useful classification of personality disorders. Am J Psychiatry 1999; 156:273–285Abstract, Google Scholar
32. Costa PTJ, McCrae RR: Six approaches to the explication of facet-level traits: examples from conscientiousness. Eur J Pers 1998; 12:117–134Crossref, Google Scholar
33. Shedler J: A new language for psychoanalytic diagnosis. J Am Psychoanal Assoc 2002; 50:429–456Crossref, Medline, Google Scholar
34. Block J: The Q-Sort Method in Personality Assessment and Psychiatric Research. Palo Alto, Calif, Consulting Psychologists Press, 1978Google Scholar
35. Westen D, Muderrisoglu S: Reliability and validity of personality disorder assessment using a systematic clinical interview: evaluating an alternative to structured interviews. J Personal Disord 2003; 17:350–368Crossref, Google Scholar
36. Westen D, Shedler J: A prototype matching approach to diagnosing personality disorders toward DSM-V. J Personal Disord 2000; 14:109–126Crossref, Medline, Google Scholar
37. Westen D, Chang C: Personality pathology in adolescence: a review. Adolesc Psychiatry 2000; 25:61–100Google Scholar
38. Kernberg O: Borderline Conditions and Pathological Narcissism. Northvale, NJ, Jason Aronson, 1975Google Scholar
39. Kernberg O: Severe Personality Disorders: Psychotherapeutic Strategies. New Haven, Conn, Yale University Press, 1984Google Scholar
40. Kohut H: The Analysis of the Self: A Systematic Approach to the Treatment of Narcissistic Personality Disorders. New York, International Universities Press, 1971Google Scholar
41. Clark LA: SNAP (Schedule for Nonadaptive and Adaptive Personality): Manual for Administration, Scoring, and Interpretation. Minneapolis, University of Minnesota Press, 1993Google Scholar
42. Cleckley H: The Mask of Sanity. St Louis, Mosby Co, 1941Google Scholar
43. Hare RD, Hart SD, Harpur TJ: Psychopathy and the DSM-IV criteria for antisocial personality disorder. J Abnorm Psychol 1991; 100:391–398Crossref, Medline, Google Scholar
44. Shapiro D: Neurotic Styles. New York, Basic Books, 1965Google Scholar
45. MacKinnon R, Michels R: The Psychiatric Interview in Clinical Practice. Philadelphia, WB Saunders, 1971Google Scholar
46. McCrae R: Psychopathology from the perspective of the five-factor model, in Differentiating Normal and Abnormal Personality. Edited by Strack S, Lorr M. New York, Springer, 1994, pp 26–39Google Scholar
47. Mischel W: Personality and Assessment. New York, John Wiley & Sons, 1968Google Scholar
48. Passini FT, Norman WT: A universal conception of personality structure. J Pers Soc Psychol 1966; 4:44–49Crossref, Medline, Google Scholar
49. Clark LA, Livesley WJ, Schroeder M, Irish S: Convergence of two systems for assessing specific traits of personality disorder. Psychol Assess 1996; 5:81–91Crossref, Google Scholar
50. Morey LC: Personality disorders in DSM-III and DSM-III-R: convergence, coverage, and internal consistency. Am J Psychiatry 1988; 145:573–577Link, Google Scholar
51. Oldham JM, Skodol AE, Kellman HD, Hyler SE, Rosnick L, Davies M: Diagnosis of DSM-III-R personality disorders by two semistructured interviews: patterns of comorbidity. Am J Psychiatry 1992; 149:213–220Link, Google Scholar
52. Pilkonis PA, Heape CL, Proietti JM, Clark SW, McDavid JD, Pitts TE: The reliability and validity of two structured diagnostic interviews for personality disorders. Arch Gen Psychiatry 1995; 52:1025–1033Crossref, Medline, Google Scholar
53. Westen D: Divergences between clinical and research methods for assessing personality disorders: implications for research and the evolution of axis II. Am J Psychiatry 1997; 154:895–903Link, Google Scholar
54. Livesley WJ, Jang KL, Vernon PA: Phenotypic and genetic structure of traits delineating personality disorder. Arch Gen Psychiatry 1998; 55:941–948Crossref, Medline, Google Scholar
55. Livesley W: The DSM-IV Personality Disorders. New York, Guilford, 1995Google Scholar
56. Jang KL, Livesley WJ: Why do measures of normal and disordered personality correlate? a study of genetic comorbidity. J Personal Disord 1999; 13:10–17Crossref, Medline, Google Scholar
57. McWilliams N: Psychoanalytic Diagnosis. New York, Guilford, 1994Google Scholar
58. Shedler J, Westen D: Refining personality disorder diagnosis: integrating science and practice. Am J Psychiatry 2004; 161:1350–1365Link, Google Scholar



