Sympathoadrenal Hyperactivity and the Etiology of Neuroleptic Malignant Syndrome
Abstract
OBJECTIVE: The author’s goal was to develop a pathophysiological model for neuroleptic malignant syndrome with greater explanatory power than the alternative hypotheses of hypothalamic dopamine antagonism (elevated set point) and direct myotoxicity (malignant hyperthermia variant). METHOD: Published clinical findings on neuroleptic malignant syndrome were integrated with data from human and animal studies of muscle physiology, thermoregulation, and autonomic nervous system function. RESULTS: The data show that the sympathetic nervous system’s latent capacity for autonomous activity is expressed when tonic inhibitory inputs from higher central nervous system centers are disrupted. These tonic inhibitory inputs are relayed to preganglionic sympathetic neurons by way of dopaminergic hypothalamospinal tracts. The sympathetic nervous system mediates hypothalamic coordination of thermoregulatory activity and is a primary regulator of muscle tone and thermogenesis, augmenting both of these when stimulated. In addition, the sympathetic nervous system modulates all of the other end-organs that function abnormally in neuroleptic malignant syndrome. CONCLUSIONS: There is substantial evidence to support the hypothesis that dysregulated sympathetic nervous system hyperactivity is responsible for most, if not all, features of neuroleptic malignant syndrome. A predisposition to more extreme sympathetic nervous system activation and/or dysfunction in response to emotional or psychological stress may constitute a trait vulnerability for neuroleptic malignant syndrome, which, when coupled with state variables such as acute psychic distress or dopamine receptor antagonism, produces the clinical syndrome of neuroleptic malignant syndrome. This hypothesis provides a more comprehensive explanation for existing clinical data than do the current alternatives.
It is widely believed that dopamine D2 (D2) receptor antagonism causes hyperthermia in neuroleptic malignant syndrome by blocking heat-loss pathways in the anterior hypothalamus, by increasing heat production secondary to extrapyramidal rigidity (1), or both, but this model has been criticized as inadequate (2, 3) and lacking sufficient evidence (4). An alternative hypothesis is that neuroleptics are directly toxic to muscle tissue, as volatile anesthetics are in malignant hyperthermia (5), but neuroleptic malignant syndrome and malignant hyperthermia likely have distinct mechanisms (6, 7). Neither model enables clinicians to identify specific patients at greater risk for neuroleptic malignant syndrome or to make reliable treatment choices (8–10).
Autonomic dysfunction is a core component of neuroleptic malignant syndrome (11, 12, DSM-IV), and peripheral catecholamines are typically elevated (13–16), but a pathophysiological role for excess catecholamines in neuroleptic malignant syndrome has been relatively overlooked. This paper provides an overview of the sympathetic nervous system and its regulatory role in body temperature, muscle function, and other organ systems that are affected in neuroleptic malignant syndrome. These data are then integrated with published clinical observations in support of the hypothesis that dysregulated sympathetic nervous system hyperactivity is the pathophysiological basis of neuroleptic malignant syndrome. The central premises of this hypothesis are the intrinsic capacity of the sympathetic nervous system for autonomous, fragmented function and its ubiquitous involvement in all of the physiological processes relevant to neuroleptic malignant syndrome. Figure 1 summarizes this thesis schematically, and the reader will find it helpful to consult it frequently.
THE SYMPATHETIC NERVOUS SYSTEM: AN OVERVIEW
Anatomy of the Autonomic Nervous System
Most organs are innervated by sympathetic and parasympathetic divisions of the autonomic nervous system, but the adrenal medulla, sweat glands, and somatic blood vessels are regulated exclusively by the sympathetic nervous system (17). Preganglionic sympathetic nervous system fibers synapse within the adrenal medulla (17) and promote catecholamine secretion (18). Sympathetic nervous system and adrenomedullary responses are often dissociated (19) and can be complementary (20, 21). The relative independence of the sympathetic nervous system from central nervous system (CNS) regulation (17), its more permeable blood-nerve barrier (22), and the ability of its end-organs to continue functioning when autonomic nerves are interrupted (17) all contribute to its capacity for autonomous function.
The sympathetic nervous system is regulated by the frontal cortex and hypothalamus. The sulcal prefrontal cortex tonically influences the hypothalamus to lower body temperature (23). Sympathetic nervous system hyperactivity ensues when the hypothalamus is released from cortical control (24), and systems lower in the neuraxis operate independently following hypothalamic lesion (25). Sweating is tonically inhibited by the frontal cortex (26), and a similar hierarchical inhibitory relationship exists between spinal cervicothoracic and thoracolumbar sudomotor (sweat gland) regulatory centers (27).
The sympathetic nervous system is regulated by the lateral and posterior hypothalamus, whereas the parasympathetic division is controlled by the anterior and medial hypothalamus (17, 24). Stimulation of the lateral hypothalamus increases adrenal nerve activity (18), and the lateral hypothalamic area provides organ- or site-specific regulation of sympathetic nervous system activity (28). Most dorsal hypothalamic spinal projection neurons are dopaminergic and appear to be involved in autonomic function (29). Dopamine terminal axon density is highest in the intermediolateral cell columns of the spinal cord, where preganglionic sympathetic nervous system neurons originate, and microelectrophoretic dopamine application there inhibits sympathetic preganglionic neurons (30). Retrograde labeling has identified caudal lateral hypothalamic area neurons as likely sympathetic nervous system “central command neurons” (31).
Autopsy findings have implicated only the posterior hypothalamus in neuroleptic malignant syndrome (32). Other autopsy results are inconclusive (33) or negative (15, 34, 35) with respect to hypothalamic pathology.
Functional Neuropharmacology of the Sympathetic Nervous System
Preganglionic sympathetic nervous system neurons release acetylcholine, but postganglionic sympathetic nervous system neurons release norepinephrine. Exceptions are sudomotor neurons and vasodilator neurons in the muscle, whose postganglionic neurons release acetylcholine, and the adrenal medulla, whose preganglionic neurons release norepinephrine (17, 36). Norepinephrine acts only within the neuroeffector junction into which it is released (37). Plasma norepinephrine levels reflect overflow from sympathetic nervous system neuroeffector junctions, and there is good correlation between muscle sympathetic nerve activity and plasma norepinephrine levels (38). Norepinephrine promotes its own release by means of prejunctional β-adrenoceptors; at higher concentrations it inhibits its own release by means of prejunctional α-adrenoceptors (39). Trains of high frequency action potentials may cause norepinephrine to accumulate, potentiating its functional effects (40). Symptoms of norepinephrine toxicity include anxiety, pallor, and intense diaphoresis (41).
Epinephrine is the major catecholamine produced by the adrenal medulla; in contrast to norepinephrine, it is released into the circulation and acts at distant receptor sites (37). Symptoms of epinephrine toxicity include fear, anxiety, tenseness, restlessness, tremor, weakness, dizziness, pallor, respiratory difficulty, and palpitations (41). Norepinephrine constitutes no more than 20% of the catecholamine content of the adrenal medulla (41), and epinephrine has no significant activity at sympathetic nerve endings (36).
Norepinephrine activates predominantly α- and β1-adrenoceptors (42) and is more potent at α1 than α2 receptors (43). Epinephrine is active primarily at β-adrenoceptors (42) and is much more potent than norepinephrine at β2 receptors, where norepinephrine has minimal activity (44). Second messengers for adrenoceptors are adenylate cyclase (activated by β, inhibited by α2) and intracellular Ca2+ (increased by α1) (45). Adrenoceptors in smooth muscle and glands are predominantly α1(19), whereas vasodilator β2-adrenoceptors in skeletal muscle normally predominate over vasoconstrictor α-adrenoceptors (44). Skeletal muscle contractility is increased by β2-adrenoceptors (44), and cardiac rate and contraction strength are both increased by β-adrenoceptors (36). A newly identified β-adrenoceptor subtype, β3, promotes lipolysis and plays a functional role in sympathetically induced thermogenesis (43, 46).
High levels of D2 receptor mRNA are expressed in the normal adrenal gland (47) and increased in human pheochromocytoma tissue (48). In animals, D2 agonists inhibit catecholamine release from adrenal glands, and D2 presynaptic receptors located on norepinephrine nerve terminals inhibit norepinephrine release if activated during nerve stimulation (49). In humans, D2 agonists cause inhibition of sympathetic output that is abolished by D2 antagonists, but only at higher degrees of sympathetic stimulation (49). These data are consistent with previously discussed anatomical evidence for dopaminergic inhibition of sympathetic nervous system function and indicate that state-dependent factors mediate D2 antagonist effects.
Hierarchical and Regional Organization of the Sympathetic Nervous System
The functional components of the sympathetic nervous system exhibit considerable autonomy. For example, sympathetic vasoconstrictor pathways are distinct from pilomotor and visceromotor pathways and can be activated differentially (50). In cats, vasoconstrictor pathways for skin and muscle are independent of one another (51) and exercise-induced sympathetic discharge is regulated differently in the kidney and muscle (52). Individual peripheral sympathetic nerves exhibit a high degree of coherence at rest but respond uniquely to experimentally induced cerebral ischemia, indicating that sympathetic nervous system circuits can convert a generalized excitatory stimulus into specific and desynchronized discharge patterns (53).
Sympathoadrenomedullary responses also vary according to stressor: some stressors increase sympathetic nervous system activity but not adrenomedullary secretion, and others have the opposite effect (54). Moreover, sympathetic nervous system outflows to different organs vary depending on the nature and intensity of the stressor (54). Autonomous and uncoordinated activity of sympathetic nervous system functional components following disruption of regulatory (hierarchical) inputs, coupled with varying affinities of norepinephrine and epinephrine for diverse and widely distributed adrenoceptor subtypes, could account for many of the clinical features of neuroleptic malignant syndrome, including its fluctuating course.
MAMMALIAN THERMOREGULATION: AN OVERVIEW
The Biochemistry of Mammalian Thermogenesis
The two principal sources of thermogenesis in mammals are uncoupled oxidative phosphorylation in mitochondria and the contractile apparatus of skeletal muscle.
Brown adipose tissue is specialized to generate large amounts of heat rapidly, a process referred to as “nonshivering thermogenesis.” Brown adipose tissue is rich in mitochondria containing uncoupling protein, which permits respiratory chain oxidation to liberate energy in the form of heat (55). Norepinephrine is a major regulator of uncoupling protein synthesis (56, 57) but may also have a direct thermogenic effect on brown adipose tissue (57). Hypertrophy of brown adipose tissue and increased uncoupling protein synthesis have been induced in the skeletal muscle of mice following 2 weeks of treatment with a β3 agonist (58).
The contraction-relaxation cycle of skeletal muscle tissue is another important thermal energy source in mammals; the term for heat generated by the contractile apparatus is “shivering thermogenesis.” Contraction is initiated when Ca2+ is released from its intracellular storage site in the sarcoplasmic reticulum and binds to contractile proteins (mainly troponin) in the sarcoplasm. Relaxation begins when intracellular [Ca2+] reaches a critical level, terminating further Ca2+ release and activating Ca2+ reuptake pumps in the sarcoplasmic reticulum membrane to move Ca2+ from sarcoplasm to sarcoplasmic reticulum against a steep gradient.
Ca2+ release from the sarcoplasmic reticulum, Ca2+ binding to troponin, Ca2+ reuptake by the sarcoplasmic reticulum, and the oxidative chemical reactions of the postcontraction recovery phase all produce heat (59), and intracellular Ca2+ transport plays a role in normal thermogenesis (60). Intracellular free [Ca2+] regulates contraction-relaxation (61), and agents that lead to sustained elevation of sarcoplasmic [Ca2+] can induce persistent contraction in the absence of an action potential (59). Creatine phosphokinase participates in regenerating high-energy cellular stores during the relaxation phase (61) and is an integral component of intracellular energy metabolism.
The Hierarchical Organization of Normal Mammalian Thermoregulation
Homeothermy evolved as existing physiological reflexes were recruited for thermoregulatory functions, gradually creating a hierarchically organized collection of parallel subsystems, each of which regulates its phylogenetic predecessor. The neutral zone, defined as the body temperature range within which no thermoeffectors (heating or cooling reflexes) are activated, narrows progressively at each level of this hierarchy, so there is an illusion of a single fixed set point (in humans, about 98.6˚F) (62). However, homeothermy represents the interaction of two separate groups of neurons—warm-sensitive and cold-sensitive (63). Warm sensitivity is mediated primarily by temperature-sensitive membrane ion conductances (64), whereas cold sensitivity requires intact local synaptic networks (64, 65). Warm-sensitive neurons activate cold effectors (e.g., sweat glands) to lower body temperature, and cold-sensitive neurons activate warm effectors (e.g., brown adipose tissue) to raise body temperature. Warm and cold effectors are never activated simultaneously by an intact thermoregulatory system (63).
Thermoregulation can be dissociated in a variety of ways. The neurotoxin capsaicin disables heat-defense responses but leaves cold-defense responses intact (23). Shivering and nonshivering thermogenesis are modulated separately following CNS lesion, and stimulation of the hypothalamus and spinal cord by opposing temperatures produces mutually independent and antagonistic thermoeffector (heating and cooling) responses (62). Almost all thermoeffectors also serve nonthermoregulatory functions, so competition between thermal and nonthermal drives is likely (23, 66). Thermosensitive neurons in the hypothalamus are very sensitive to emotional and behavioral inputs, and their response is determined by perturbation magnitude rather than hedonic attributes (23). Sympathetic nervous system activity in human skin is increased by mental stress as well as thermal inputs (67), and many dorsal horn spinal neurons are excited by both mechanical and thermal stimuli (68). Emotional fever is provoked by restraint or novel stimuli in some species, and anticipation can elevate body temperature in humans. These are true fevers in that they result from coordinated thermoeffector function (heat effectors turned on, cold effectors turned off) (69, 70).
Stimulation of the preoptic hypothalamus can induce fever, but this structure is not essential because fever is under the control of multiple CNS structures (69). The mammalian spinal cord has thermosensory and thermoregulatory properties (51), but only extreme changes in body temperature elicit thermoregulatory responses in the absence of the hypothalamus (62). Humans with spinal cord transections have wider core temperature fluctuations (70), and subjects with complete cervical cord transections have increased core temperatures despite preserved regional heat-induced sweating (27). Some capacity for thermoregulation is preserved when hypothalamic regulatory inputs are interrupted, so hypothalamic dysfunction alone cannot explain the extreme hyperthermia sometimes encountered in neuroleptic malignant syndrome.
CNS Dopamine and Mammalian Thermoregulation
It is widely believed that central dopamine receptor antagonism within the hypothalamus is necessary for neuroleptic malignant syndrome to occur, but the thermoregulatory role of dopamine is more complex. d-Amphetamine (an indirect dopamine agonist) produces hypothermia or hyperthermia in rats, depending on the ambient temperature, apparently by way of independent pathways (71, 72). Acutely and chronically reserpinized rats demonstrate a reciprocal and state-dependent D1-D2 receptor interaction in their thermoregulatory responses (73). Neuroleptic malignant syndrome has followed neuroleptic dose reduction (74), discontinuation (75), and long-term stable dosing (76). Also, there is a report of severe extrapyramidal symptoms and hypothermia with fluphenazine, followed by rebound hyperthermia when this drug was discontinued (77). Body temperature is highly correlated with plasma prolactin in thermally stressed men (78), suggesting that normal heat defense is associated with decreased central dopamine, and intraventricular haloperidol produces a coordinated heat-defense response (79). These reports refute a unique or essential role for central dopamine antagonism in neuroleptic malignant syndrome hyperthermia and provide additional evidence that state-dependent factors are important mediators of dopamine antagonist effects.
THE SYMPATHETIC NERVOUS SYSTEM: NORMAL PHYSIOLOGICAL FUNCTION
The Role of the Sympathetic Nervous System in Normal Muscle Function
The sympathetic nervous system plays an integral role in normal muscle function. Force is potentiated by β-adrenoceptor agonists in mammalian skeletal muscle, and adrenoceptors on skeletal myocyte membranes are predominantly β2(80), indicating that epinephrine normally is directly involved in regulating skeletal muscle contraction. In skeletal and heart muscle fibers, β-adrenoceptor agonists promote phosphorylation of Ca2+ channels, increasing the probability of their being open (81). Epinephrine increases contraction strength by way of this altered Ca2+ influx (81), apparently by increasing the amount of Ca2+ released from the sarcoplasmic reticulum into sarcoplasm during activation (82). Epinephrine-induced Ca2+ influx by way of myocyte membrane channels also increases intracellular [Ca2+], and the same effect is seen with the α1-adrenoceptor agonist phenylephrine (82). Liver Ca2+ homeostasis and muscle Ca2+ homeostasis are similar, and norepinephrine induces a sustained rise in hepatocellular [Ca2+] (60). In rabbits, α1-adrenoceptor agonists cause dose-dependent increases in peak skeletal muscle tension (83). Thus, norepinephrine and epinephrine are both potent activators of skeletal muscle and exert this effect by altering intracellular [Ca2+].
Norepinephrine has similar effects on smooth muscle. In rabbits, norepinephrine triggers Ca2+-induced Ca2+ release (84), a process whereby a large amount of Ca2+ is released from the sarcoplasmic reticulum in response to a much smaller amount of Ca2+ outside the sarcoplasmic reticulum (85). Norepinephrine-induced Ca2+ release can activate smooth muscle contraction fully (86), and in guinea pig myocytes, norepinephrine produces spontaneous Ca2+-induced transmembrane electrical transients that can cause depolarization (87). Ca2+-induced Ca2+ release is responsible for caffeine-induced contractures in skeletal muscle (88).
The Role of the Sympathetic Nervous System in Normal Mammalian Thermoregulation
All thermoeffector activity is regulated by the sympathetic nervous system. Both the sympathetic nervous system and the adrenal medulla are capable of preventing fatal hypothermia when the other is incapacitated (89). Norepinephrine is the primary regulator of brown adipose tissue metabolic activity and growth (25), and norepinephrine also stimulates hormone-sensitive lipase, the principal lipolytic enzyme in white adipose tissue (89). Persistent β-adrenergic stimulation induces brown adipose tissue hypertrophy and accelerated uncoupling protein gene transcription in rats (58), and although brown adipose tissue is probably not a major thermogenic tissue in man (89), it does persist throughout adulthood (90) and can be reactivated following intense sympathetic stimulation (e.g., in cold acclimation or by a pheochromocytoma) (25). Repeated norepinephrine infusions potentiate thermogenesis in humans (91).
Uncoupling protein synthesis can be induced in rat skeletal muscle following persistent adrenergic stimulation (58), and skeletal muscle is the primary site of sympathomimetic-induced thermogenesis in humans (90). Catecholamine-induced increases in intracellular [Ca2+] generate heat because chemical-mechanical transduction efficiency is low (92). Salbutamol, a selective β2-adrenergic agonist, is thermogenic in humans (93). Ephedrine, a mixed α- and β-adrenoceptor agonist, has a potent thermogenic effect in humans (90) that is mediated by norepinephrine and probably involves β3-adrenoceptors (46). Isoproterenol, a nonselective β-adrenoceptor agonist, substantially increases the metabolic rate in humans, apparently through β1- and β3-adrenoceptors (94). In one mammal, norepinephrine substantially increases skeletal muscle thermogenesis through α1-adrenoceptors, independent of uncoupling protein (95).
Nonsteroidal anti-inflammatory agents are ineffective against the hyperthermia of neuroleptic malignant syndrome, and dantrolene provides only inconsistent benefit, so it is worth noting that both indomethacin and dantrolene fail to inhibit phenylephrine-stimulated thermogenesis in small mammals (95). These treatments would not be expected to reverse hyperthermia caused by a hyperadrenergic state in which unregulated thermogenesis, due to uncoupled phosphorylation and/or disrupted intracellular Ca2+ homeostasis, predominates.
The following general principles should now be evident:
| 1. | Hierarchically organized thermoregulatory centers are located at all levels of the CNS. | ||||
| 2. | The sympathetic nervous system is intimately involved in all aspects of thermoregulation. | ||||
| 3. | The sympathetic nervous system consists of potentially autonomous components whose functions are normally coordinated and integrated by the hypothalamus, but which function independently when these regulatory inputs are disrupted. | ||||
| 4. | Dopamine antagonists interrupt tonic inhibitory modulation of sympathetic nervous system function at the spinal cord level, an effect that is most evident when the sympathetic nervous system is hyperactive. | ||||
| 5. | Sympathetic nervous system hyperactivity is associated with intense emotional stress and frontal cortical dysfunction. | ||||
| 6. | The sympathetic nervous system can augment or initiate skeletal muscle contractile activity by means of adrenoceptor-mediated increases in intracellular Ca2+ levels. | ||||
The following sections explore the role of sympathetic nervous system hyperactivity in the clinical presentation of neuroleptic malignant syndrome. Again, the reader will find figure 1 helpful in following the discussion.
SYMPATHETIC NERVOUS SYSTEM DYSREGULATION AND THE PATHOPHYSIOLOGY OF NEUROLEPTIC MALIGNANT SYNDROME
Neuroleptic Malignant Syndrome Risk Factors
Organic brain disease is a risk factor for neuroleptic malignant syndrome (8, 96– 98) and for increased morbidity and mortality from this disorder (97, 99). Mental retardation is relatively frequent among cases of neuroleptic malignant syndrome (8, 33, 100), and in one small series the most severe syndrome was associated with bilateral frontal lesions (101). Catatonia, considered a harbinger of neuroleptic malignant syndrome by some (102), is likely a frontal lobe syndrome (103, 104).
Affective illness is another risk factor for neuroleptic malignant syndrome (98, 99, 105, 106). Sympathetic nervous system activity is increased in major depression (107); the relative contributions of the sympathetic nervous system and adrenomedullary components vary by depression subtype (108). In manic patients, adrenomedullary activity is associated with affective and behavioral symptoms but sympathetic nervous system activity is correlated more strongly with agitation (20). Rhabdomyolysis has been observed in mania (109). Plasma catecholamines and their metabolites are elevated in periodic catatonia (110, 111), which may be a variant of bipolar disorder (103) and bears a strong clinical resemblance to neuroleptic malignant syndrome.
Illness Onset and Course
The temporal pattern in which specific features of neuroleptic malignant syndrome emerge is inconsistent across cases (99, 101, 112), but autonomic hyperactivity is often the earliest clinical finding. Although fulminant neuroleptic malignant syndrome may present suddenly, more often the course is indolent, with unexplained episodic tachycardia and blood pressure fluctuations observed early on (112). In particular, elevated diastolic blood pressure may be antecedent (113). In the prodrome that frequently precedes a full-blown syndrome (114), dysautonomic features typically predominate (99, 115, 116). Dysautonomia can appear without hyperthermia (117) or precede hyperthermia (75, 113, 116, 118), which sometimes emerges relatively late (101, 112). Individual differences in the rates of catecholamine release and clearance, which are the primary determinants of their physiological effect (119), may contribute to the variability of the clinical course. Opposing effects of α- and β-adrenoceptor stimulation, as well as differing affinities of epinephrine and norepinephrine for these receptors, provide additional sources of variability in clinical presentation over time.
Major Clinical Features
Altered mental status
Altered consciousness is considered by some (120) to be a sine qua non for the diagnosis of neuroleptic malignant syndrome. In one relatively large series (98), “a striking, frightened facial expression was observed in all cases,” accompanied by “a sense of doom” and “overwhelming anxiety” (p. 719). Tollefson (6) described a mute and akinetic patient with neuroleptic malignant syndrome as having “an exaggerated startle response.” Catatonic patients retrospectively report intense, uncontrollable anxieties (104). Healthy volunteers viewing a frightening film have increased plasma norepinephrine, but their other catecholamine and endocrine levels are normal (121). Psychological stress is positively correlated with plasma vanillylmandelic acid but not 3-methoxy-4-hydroxyphenylglycol, homovanillic acid, or 5-hydroxyindoleacetic acid, suggesting that the sympathetic nervous system is activated more by transient emotional stress than by persistent emotional conditions (122).
Acute, but not subacute or chronic, psychosis and Brief Psychiatric Rating Scale scores indicating global psychopathology and anxiety are positively correlated with serum creatine phosphokinase levels (123). Catatonic excitement has been promoted as a highly reliable risk factor for neuroleptic malignant syndrome (102), and labile mood and insomnia consistently precede lethal catatonia (124). “Emotional disturbance” can trigger hyperthermia and many of the clinical features usually associated with neuroleptic malignant syndrome (125), as can acute phencyclidine-induced psychosis (126). Intense emotional or psychological disturbance, with altered frontal cortical function, could be a pathophysiological link between these syndromes and neuroleptic malignant syndrome.
Dysautonomia
Diaphoresis is common in neuroleptic malignant syndrome (124), with rates from 50% to 100% (98, 99, 105), and is due to direct sympathetic nervous system stimulation rather than circulating catecholamines (17, 36). In contrast to its role in true fever, diaphoresis in neuroleptic malignant syndrome is not part of a coordinated effort to lower body temperature (127). Eccrine sweat glands are the only mammalian organs with a purely thermoregulatory function (23) and have the capacity to dissipate heat faster than it can be generated (128), so hyperthermia in neuroleptic malignant syndrome implicates a defective heat-loss mechanism in addition to any increase in thermogenesis. Excessive sweat gland activity is probably responsible for neuroleptic-malignant-syndrome-associated dehydration in some cases (129), and dehydration may contribute to hyperthermia.
Tachypnea and tachycardia in neuroleptic malignant syndrome reflect a hyperadrenergic state, but increased metabolism makes additional demands on the cardiopulmonary system. In one drug-induced syndrome similar to neuroleptic malignant syndrome, body temperature increased in tandem with blood pressure and heart rate (130), and body temperature accounts for as much as 16% of the respiratory rate variance in neuroleptic malignant syndrome (127).
Urinary incontinence is another clinical manifestation of autonomic dysfunction in neuroleptic malignant syndrome. The bladder base and internal sphincter consist of smooth muscle innervated exclusively by predominantly α-adrenergic sympathetic nervous system fibers. Voluntary restraint of micturition requires the frontal lobes, and lesions in either hemisphere can cause bladder incontinence (17, 67). In spinal cord patients, diaphoresis and bladder incontinence are associated with flexor spasms of the lower extremities, suggesting an intrinsic relationship among these motor responses (27).
Catecholamine excess alone can produce a syndrome similar to neuroleptic malignant syndrome, as illustrated by the case of a 34-year-old woman who experienced the sudden onset of palpitations, inability to move or speak, and labile postural tachycardia and hypertension (111). Mutism, increased muscle tone, hyperactive tendon reflexes, and catalepsy were reproduced reliably by physical activity and anxiety-provoking situations and were always associated with hypertension and tachycardia. Plasma epinephrine and norepinephrine were markedly elevated and correlated with amount of time upright, but urine 24-hour catecholamine and monoamine metabolite levels were normal. She was found to have a hyperactive sympathetic response and peripheral α1-adrenoceptor subsensitivity (111).
Hyperthermia
Hyperthermia can occur when the heat-loss apparatus is defective or when intact thermoeffectors are poorly coordinated. The ineffectiveness of diaphoresis, normally a potent cold effector, in neuroleptic malignant syndrome has already been discussed. The simultaneous activation of both warm and cold effectors in neuroleptic malignant syndrome indicates that although thermoeffectors remain operational, their activities are not coordinated (76, 127, 131). This condition alone would be sufficient for hyperthermia to supervene, but in addition there are two likely sources of excess thermogenesis in neuroleptic malignant syndrome: accelerated brown-adipose-tissue-like metabolism (uncoupled phosphorylation) and excessive catecholamine-induced Ca2+ release from the sarcoplasmic reticulum.
Persistent stimulation of sarcoplasmic reticulum Ca2+ release would lead to continuous activation of Ca2+ reuptake mechanisms, releasing heat as a by-product. This could account for the observation that serum creatine phosphokinase levels are positively correlated with 24-hour urinary catecholamine metabolite excretion in neuroleptic malignant syndrome (16). The appearance of elevated muscle enzyme levels in neuroleptic malignant syndrome before clinical signs of autonomic instability are evident indicates that hypermetabolism may precede the full syndrome (132). Hypermetabolism related to hyperthyroidism, in the absence of central dopamine blockade, can produce a syndrome similar to neuroleptic malignant syndrome (133).
Peripheral catecholamines also directly stimulate uncoupled phosphorylation in mitochondria, as occurs in some cases of pheochromocytoma, cold exposure, and treatment with sympathomimetic agents. As in these other examples, prolonged elevation of peripheral catecholamine levels in neuroleptic malignant syndrome may even lead to induction of uncoupling protein mRNA and increased thermogenic tissue mass, suggesting a possible physiological basis for persistent hyperthermia during recovery from neuroleptic malignant syndrome. This thermogenic mechanism is distinct from that related to intracellular Ca2+ homeostasis. Hyperthermia in neuroleptic malignant syndrome can be dissociated from muscle rigidity (33, 134) and creatine phosphokinase levels (135), precede extrapyramidal signs (115), and persist despite curarization-induced flaccidity (33). The lack of glycogen and lipid stores in muscle biopsies strongly suggests that uncoupled phosphorylation contributes to hyperthermia in neuroleptic malignant syndrome (136).
Rigidity, elevated creatine phosphokinase, and rhabdomyolysis
Asymptomatic creatine phosphokinase elevations occur in patients with psychotic disorders, whether clinically stable or acutely ill, following oral treatment with typical or atypical neuroleptics (137–139). Clozapine is associated with more frequent and higher creatine phosphokinase elevations than are typical neuroleptics (139); this is noteworthy because clozapine has significantly greater α2-adrenoceptor activity (140), which is probably the cause of de novo diabetes mellitus in clozapine-treated patients (141). Substantial creatine phosphokinase elevations accompanied only by tachycardia and elevated blood pressure may follow neuroleptic treatment (142), suggesting a hypermetabolic effect mediated by the sympathetic nervous system.
Cardiac lesions caused by elevated catecholamines are indistinguishable from atherosclerotic lesions (143). Short-term hypoxia permits creatine phosphokinase-MB to escape without necrosis (144), and intravenous isoproterenol causes elevated creatine phosphokinase-MB in childhood asthmatics (145). Elevated creatine phosphokinase and focal skeletal myositis occur in pheochromocytoma (146), which releases mainly norepinephrine (119). Ischemia mediated by catecholamine-induced vasoconstriction in skeletal muscle is probably the cause of muscle injury in pheochromocytoma (147). Creatine phosphokinase elevations and myoglobinuria in neuroleptic malignant syndrome may exist without rigidity or tremor (148), and haloperidol-induced rhabdomyolysis is associated with autonomic dysfunction but not rigidity (149).
Urinary catecholamines and catecholamine metabolites are positively correlated with blood creatine phosphokinase levels in acute neuroleptic malignant syndrome, but other clinical features are not (16). In patients with neuroleptic malignant syndrome, serum creatine phosphokinase covaries nonlinearly with other muscle enzymes and exceeds by as much as 15-fold the normal extracellular-intracellular gradient, indicating that muscle necrosis alone cannot account for elevated creatine phosphokinase levels (150). Experimental tissue injury models suggest that increased enzyme synthesis represents a reparative response to a noxious agent (151). The noxious event in neuroleptic malignant syndrome could be a relative hypoxia created by a metabolism-perfusion mismatch caused by a hyperactive and unregulated sympathetic nervous system.
Catecholamine-induced Ca2+ release from the sarcoplasmic reticulum may also cause cell death (152). Focal myocardial necrosis occurs in patients with pheochromocytoma (153), in rats infused with epinephrine and norepinephrine (143), and in dogs infused with inotropic amines (154). Muscle necrosis in these settings is apparently due to a direct effect of catecholamines on Ca2+ influx (81, 153). Oxidation of excess catecholamines to catecholamine-O-quinones, with subsequent formation of superoxide radicals that attack cellular membrane and protein constituents essential to energy metabolism, is another mechanism by which excess catecholamines can damage myocytes (155).
Muscle biopsy findings in patients with neuroleptic malignant syndrome have yielded minimal or inconsistent results (compare references 6 and 156 with references 34, 120, 136, and 157). Muscle abnormalities that have been detected in neuroleptic malignant syndrome resemble those found in malignant hyperthermia (157) or consist of endomysial edema with a striking absence of both glycogen and lipid substrate stores (136). Profound depletion of intracellular energy stores strongly implicates uncoupled phosphorylation as the source of hyperpyrexia (136), and the resemblance to malignant hyperthermia in these cases implicates Ca2+ overload as a common etiological factor. A majority of patients with severe neuroleptic malignant syndrome have documented serum hypocalcemia (98), which could reflect a sudden net influx of Ca2+ into myocytes that coincides with a “malignant” phase of the syndrome.
Extrapyramidal signs associated with neuroleptic malignant syndrome include rigidity, tremor, cogwheeling, dystonia, chorea, dyskinesia, opisthotonos, opsoclonus, and posturing (3, 5, DSM-IV). As the data presented here indicate, rigidity in neuroleptic malignant syndrome could be caused by catecholamine-induced changes in intracellular [Ca2+], and tremors could also reflect elevated peripheral catecholamines. Increased muscle tone caused by sympathetic nervous system hyperactivity is independent of, but may coexist with, effects of neuroleptics on the extrapyramidal system, and the presence of more complex motor signs implicates concomitant basal ganglia involvement in some cases of neuroleptic malignant syndrome.
Associated Clinical Findings
Granulocytosis is a feature of neuroleptic malignant syndrome (3, 97), and sympathetic nervous system fibers innervate lymphoid tissue (158). Catecholamines stimulate lymphocytes at low concentrations, but at high concentrations they are inhibitory (158). Lymphocyte circulation is mediated mainly by plasma membrane β2-adrenoceptors, whereas granulocyte circulation increases are mediated by α-adrenoceptor stimulation (42). An injection of norepinephrine can raise neutrophil levels to two to three times normal (159), and increased peripheral norepinephrine turnover is associated with reduced lymphocyte proliferation (160). The net effect of sympathetic nervous system stimulation is leukocytosis with a “shift to the left.”
Blood sugar homeostasis is regulated by the sympathetic nervous system and can be impaired in neuroleptic malignant syndrome. A 44-year-old man with no previous history of diabetes mellitus developed neuroleptic malignant syndrome and fatal diabetic ketoacidosis precipitously following a test dose of zuclopenthixol decanoate (161). Under normal physiological circumstances, the sympathetic nervous system tonically suppresses insulin release through α-adrenoceptors (162); stimulation of the pancreatic sympathetic nerve decreases insulin secretion and increases glucagon secretion (163).
Bilateral E coli anterior tibial fasciitis in one case of neuroleptic malignant syndrome (164) may have resulted from ischemic muscle necrosis. Noncardiogenic pulmonary edema in neuroleptic malignant syndrome (165) could be caused by excess sympathetic nervous system activity because pheochromocytomas can cause pulmonary edema (147). Necrotizing colitis without fever, possibly a result of sympathetic-nervous-system-mediated vasoconstriction, has been attributed to neuroleptic treatment (166), and ischemic bowel followed respiratory failure in another case of neuroleptic malignant syndrome (114). Paralytic ileus in neuroleptic malignant syndrome (167) may be the result of intense sympathetic nervous system activation (44).
DISCUSSION
The intrinsic capacity of the sympathetic nervous system for fragmented, autonomous activity normally is suppressed by inhibitory regulatory inputs originating in the frontal cortex and mediated by hypothalamic nuclei. The hypothalamus integrates afferent thermosensory information and coordinates thermoeffector responses by means of dopaminergic modulation of preganglionic sympathetic nervous system neurons. Disruption of these inhibitory inputs leads to dysregulated sympathetic nervous system hyperactivity with uncoordinated, excessive stimulation of end-organs by autonomous functional components of the sympathetic nervous system—vasomotor, sudomotor, inotropic, thermogenic, and others. In particular, extreme psychic distress (altered frontal lobe function) or acute dopamine antagonism (of hypothalamospinal tracts) may alter sympathetic nervous system function and lead to profound disturbances of homeostasis. Manifestations of dysregulated sympathetic nervous system hyperactivity include increased muscle metabolism and tone (due to increased intracellular [Ca2+]), of which elevated creatine phosphokinase is one indicator; increased mitochondrial thermogenesis (caused by uncoupled oxidative phosphorylation); ineffective heat dissipation related to unregulated vasomotor and sudomotor activity; fluctuations in vasomotor tone leading to labile blood pressure, flushing, and pallor; granulocytosis; and urinary incontinence.
The inherent autonomy of these circuits permits these effects to be produced independently of one another, but they may interact to destabilize homeothermic and hemodynamic systems, producing the clinical syndrome of neuroleptic malignant syndrome. Figure 1 illustrates how such a pathophysiological cascade might occur. The relative mutual independence of neural and adrenal segments of the sympathetic nervous system, and the differential effects of norepinephrine and epinephrine at adrenoceptors, contribute to the unpredictable course and fluctuating clinical signs and symptoms that characterize this disorder. Direct effects of neuroleptics on extrapyramidal systems may interact with sympathetic nervous system dysfunction to produce the final clinical picture.
Presented in part at the 53rd Annual Scientific Convention of the Society of Biological Psychiatry, Toronto, May 27–31, 1998. Received March 2, 1998; revision received July 30, 1998; accepted Aug. 25, 1998. From the Department of Psychiatry, Harvard Medical School, Brockton-West Roxbury DVA Medical Center. Address reprint requests to Dr. Gurrera, Brockton DVAMC (116A), 940 Belmont St., Brockton, MA 02301; [email protected] (e-mail). Supported by DVA Medical Research Funds.
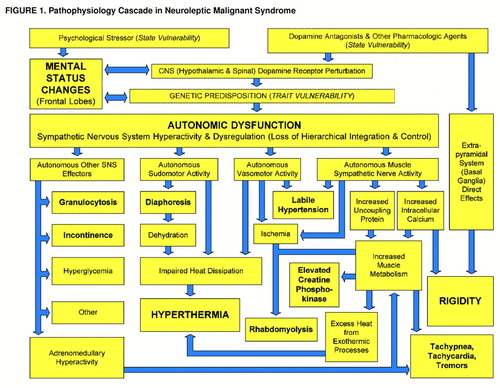
Figure 1. Pathophysiology Cascade in Neuroleptic Malignant Syndrome
1. Mann SC, Caroff SN, Lazarus A: Pathogenesis of neuroleptic malignant syndrome. Psychiatr Annals 1991; 21:175–180Crossref, Google Scholar
2. Greenberg LB, Gujavarty K: The neuroleptic malignant syndrome: review and report of three cases. Compr Psychiatry 1985; 26:63–70Crossref, Medline, Google Scholar
3. Caroff SN, Mann SC: Neuroleptic malignant syndrome. Med Clin North Am 1993; 77:185–202Crossref, Medline, Google Scholar
4. Fink M: Neuroleptic malignant syndrome and catatonia: one entity or two? Biol Psychiatry 1996; 39:1–4Google Scholar
5. Lazarus A, Mann SC, Caroff SN: The Neuroleptic Malignant Syndrome and Related Conditions. Washington, DC, American Psychiatric Press, 1989Google Scholar
6. Tollefson G: A case of neuroleptic malignant syndrome: in vitro muscle comparison with malignant hyperthermia. J Clin Psychopharmacol 1982; 2:266–270Medline, Google Scholar
7. Miyatake R, Iwahashi K, Matsushita M, Nakamura K, Suwaki H: No association between the neuroleptic malignant syndrome and mutations in the RYR1 gene associated with malignant hyperthermia. J Neurol Sci 1996; 143:161–165Crossref, Medline, Google Scholar
8. Shalev A, Hermesh H, Munitz H: Mortality from neuroleptic malignant syndrome. J Clin Psychiatry 1989; 50:18–25Medline, Google Scholar
9. Sakkas P, Davis JM, Janicak PG, Wang Z: Drug treatment of the neuroleptic malignant syndrome. Psychopharmacol Bull 1991; 27:381–384Medline, Google Scholar
10. Rosebush PI, Stewart T, Mazurek MF: The treatment of neuroleptic malignant syndrome. Br J Psychiatry 1991; 159:709–712Crossref, Medline, Google Scholar
11. Gurrera RJ, Chang SS, Romero JA: A comparison of diagnostic criteria for neuroleptic malignant syndrome. J Clin Psychiatry 1992; 53:56–62Medline, Google Scholar
12. Adityanjee, Singh S, Singh G, Ong S: Spectrum concept of neuroleptic malignant syndrome. Br J Psychiatry 1988; 153:107–111Crossref, Medline, Google Scholar
13. Feibel JH, Schiffer RB: Sympathoadrenomedullary hyperactivity in the neuroleptic malignant syndrome: a case report. Am J Psychiatry 1981; 138:1115–1116Link, Google Scholar
14. Hashimoto F, Sherman CB, Jeffery WH: Neuroleptic malignant syndrome and dopaminergic blockade. Arch Intern Med 1984; 144:629–630Crossref, Medline, Google Scholar
15. Ansseau M, Reynolds CF III, Kupfer DJ, Poncelet P-F, Franck G, Dresse AE, Reznik M: Central dopaminergic and noradrenergic receptor blockade in a patient with neuroleptic malignant syndrome. J Clin Psychiatry 1986; 47:320–321Medline, Google Scholar
16. Gurrera R, Romero J: Sympathoadrenomedullary activity in neuroleptic malignant syndrome. Biol Psychiatry 1992; 32:334–343Crossref, Medline, Google Scholar
17. Adams RD, Victor M: Disorders of the autonomic nervous system, in Principles of Neurology, 5th ed. New York, McGraw-Hill, 1993, pp 457–479Google Scholar
18. Yoshimatsu H, Oomura Y, Katafuchi T, Niijima A: Effects of hypothalamic stimulation and lesion on adrenal nerve activity. Am J Physiol 1987; 253(3, part 2):R418–R424Google Scholar
19. Lake CR, Chernow B, Feuerstein G, Goldstein DS, Ziegler MG: The sympathetic nervous system in man: its evaluation and the measurement of plasma NE, in Norepinephrine: Frontiers of Clinical Neuroscience, vol 2. Edited by Ziegler MG, Lake CR. Baltimore, Williams & Wilkins, 1984, pp 1–26Google Scholar
20. Swann AC, Secunda SK, Koslow SH, Katz MM, Bowden CL, Maas JW, Davis JM, Robins E: Mania: sympathoadrenal function and clinical state. Psychiatry Res 1991; 37:195–205Crossref, Medline, Google Scholar
21. Takahashi A, Ikarashi Y, Ishimaru H, Maruyama Y: Compensation between sympathetic nerves and adrenal medullary activity: effects of adrenodemedullation and chemical sympathectomy on catecholamine turnover. Life Sci 1993; 53:1567–1572Crossref, Medline, Google Scholar
22. Kiernan JA: Vascular permeability in the peripheral autonomic and somatic nervous systems: controversial aspects and comparisons with the blood-brain barrier. Microsc Res Tech 1996; 35:122–136Crossref, Medline, Google Scholar
23. Hori T: An update on thermosensitive neurons in the brain: from cellular biology to thermal and non-thermal homeostatic functions. Jpn J Physiol 1991; 41:1–22Crossref, Medline, Google Scholar
24. Carpenter MB: Core Text of Neuroanatomy. Baltimore, Williams & Wilkins, 1972Google Scholar
25. Himms-Hagen J: Thermogenesis in brown adipose tissue as an energy buffer: implications for obesity. N Engl J Med 1984; 311:1549–1558Crossref, Medline, Google Scholar
26. Korpelainen JT, Tolonen U, Sotaniemi KA, Myllyla VV: Suppressed sympathetic skin response in brain infarction. Stroke 1993; 24:1389–1392Crossref, Medline, Google Scholar
27. Silver JR, Randall WC, Guttmann L: Spinal mediation of thermally induced sweating. J Neurol Neurosurg Psychiatry 1991; 54:297–304Crossref, Medline, Google Scholar
28. Yoshimatsu H, Egawa M, Bray GA: Sympathetic nerve activity after discrete hypothalamic injections of L-glutamate. Brain Res 1993; 601:121–128Crossref, Medline, Google Scholar
29. Cechetto DF, Saper CB: Neurochemical organization of the hypothalamic projection to the spinal cord in the rat. J Comp Neurol 1988; 272:579–604Crossref, Medline, Google Scholar
30. Lindvall O, Bjorklund A, Skagerberg G: Dopamine-containing neurons in the spinal cord: anatomy and some functional aspects. Ann Neurol 1983; 14:255–260Crossref, Medline, Google Scholar
31. Jansen ASP, Nguyen XV, Karpitskiy V, Mettenleiter TC, Loewy AD: Central command neurons of the sympathetic nervous system: basis of the fight-or-flight response. Science 1995; 270:644–646Crossref, Medline, Google Scholar
32. Horn E, Lach B, Lapierre Y, Hrdina P: Hypothalamic pathology in the neuroleptic malignant syndrome. Am J Psychiatry 1988; 145:617–620Link, Google Scholar
33. Morris HH III, McCormick WF, Reinarz JA: Neuroleptic malignant syndrome. Arch Neurol 1980; 37:462–463Crossref, Medline, Google Scholar
34. Lee S, Merriam A, Kim T-S, Liebling M, Dickson DW, Moore GRW: Cerebellar degeneration in neuroleptic malignant syndrome: neuropathologic findings and review of the literature concerning heat-related nervous system injury. J Neurol Neurosurg Psychiatry 1989; 52:387–391Crossref, Medline, Google Scholar
35. Kish SJ, Kleinert R, Minauf M, Gilbert J, Walter GF, Slimovitch C, Maurer E, Rezvani Y, Myers R, Hornykiewicz O: Brain neurotransmitter changes in three patients who had a fatal hyperthermia syndrome. Am J Psychiatry 1990; 147:1358–1363Link, Google Scholar
36. deGroot J, Chusid JG: Correlative Neuroanatomy, 20th ed. Stamford, Conn, Appleton & Lange, 1988Google Scholar
37. Kopin IJ: Biochemical evaluation of sympatho-adrenal medullary activity—an overview, in Catecholamines as Hormone Regulators: Serono Symposia Publications, vol 18. Edited by Ben-Jonathan N, Bahr JM, Weiner RI. New York, Raven Press, 1985, pp 175–188Google Scholar
38. Wallin BG: Sympathetic activity in human extremity nerves and its relationship to plasma NE, in Norepinephrine: Frontiers of Clinical Neuroscience, vol 2. Edited by Ziegler MG, Lake CR. Baltimore, Williams & Wilkins, 1984, pp 431–438Google Scholar
39. Sneddon P, McLaren GJ, Kennedy C: Purinergic cotransmission: sympathetic nerves. Semin Neurosci 1996; 8:201–205Crossref, Google Scholar
40. Gonon F, Msghina M, Stjarne L: Kinetics of noradrenaline released by sympathetic nerves. Neuroscience 1993; 56:535–538Crossref, Medline, Google Scholar
41. Weiner N: Norepinephrine, epinephrine, and the sympathomimetic amines, in Goodman and Gilman’s The Pharmacological Basis of Therapeutics, 6th ed. Edited by Gilman AG, Goodman LS, Gilman A. New York, Macmillan, 1980, pp 138–175Google Scholar
42. Benschop RJ, Rodriguez-Feuerhahn M, Schedlowski M: Catecholamine-induced leukocytosis: early observations, current research, and future directions. Brain Behav Immun 1996; 10:77–91Crossref, Medline, Google Scholar
43. Insel PA: Adrenergic receptors—evolving concepts and clinical implications. N Engl J Med 1996; 334:580–585Crossref, Medline, Google Scholar
44. Lefkowitz RJ, Hoffman BB, Taylor P: Neurohumeral transmission: the autonomic and somatic motor nervous systems, in Goodman and Gilman’s The Pharmacological Basis of Therapeutics, 8th ed. Edited by Goodman AG, Rall TW, Nies AS, Taylor P. New York, Pergamon Press, 1990, pp 84–121Google Scholar
45. Motulsky HJ, Insel PA: Adrenergic receptors in man: direct identification, physiologic regulation, and clinical alterations. N Engl J Med 1982; 307:18–29Crossref, Medline, Google Scholar
46. Liu Y-L, Toubro S, Astrup A, Stock MJ: Contribution of beta3-adrenoceptor activation to ephedrine-induced thermogenesis in humans. Int J Obesity 1995; 19:678–685Google Scholar
47. Civelli O: Molecular biology of the dopamine receptor subtypes, in Psychopharmacology: The Fourth Generation of Progress. Edited by Bloom FE, Kupfer DJ. New York, Raven Press, 1995, pp 155–161Google Scholar
48. Pupilli C, Lanzillotti R, Fiorelli G, Selli C, Gomez RA, Carey RM, Serio M, Mannelli M: Dopamine D2 receptor gene expression and binding sites in adrenal medulla and pheochromocytoma. J Clin Endocrinol Metab 1994; 79:56–61Medline, Google Scholar
49. Mannelli M, Lazzeri C, Ianni L, Villa G La, Pupilli C, Bellini F, Serio M, Franchi F: Dopamine and sympathoadrenal activity in man. Clin Exp Hypertens 1997; 19:163–179Crossref, Medline, Google Scholar
50. Gibbins IL, Matthew SE, Bridgman N, Morris JL: Sympathetic vasoconstrictor neurons projecting from the guinea-pig superior cervical ganglion to cutaneous or skeletal muscle vascular beds can be distinguished by soma size. Neurosci Lett 1996; 213:197–200Crossref, Medline, Google Scholar
51. Grewe W, Janig W, Kummel H: Effects of hypothalamic thermal stimuli on sympathetic neurones innervating skin and skeletal muscle of the cat hindlimb. J Physiol 1995; 488:139–152Crossref, Medline, Google Scholar
52. Hill JM, Adreani CM, Kaufman MP: Muscle reflex stimulates sympathetic postganglionic efferents innervating triceps surae muscles of cats. Am J Physiol 1996; 271(1, part 2):H38–H43Google Scholar
53. Kocsis B, Fedina L, Gyimesi-Pelczer K, Ladocsi T, Pasztor E: Differential sympathetic reactions during cerebral ischemia in cats: the role of desynchronized nerve discharge. J Physiol (Lond) 1993; 469:37–50Crossref, Google Scholar
54. Goldstein DS: The sympathetic nervous system and the “fight-or-flight” response: outmoded ideas? Mol Psychiatry 1996; 1:95–97Google Scholar
55. Klingenberg M: Mechanism and evolution of the uncoupling protein of brown adipose tissue. Trends Biochem Sci 1990; 15:108–112Crossref, Medline, Google Scholar
56. Rabelo R, Reyes C, Schifman A, Silva JE: A complex retinoic acid response element in the uncoupling protein gene defines a novel role for retinoids in thermogenesis. Endocrinology 1996; 137:3488–3496Crossref, Medline, Google Scholar
57. Arancibia S, Rage F, Astier H, Tapia-Arancibia L: Neuroendocrine and autonomous mechanisms underlying thermoregulation in cold environment. Neuroendocrinology 1996; 64:257–267Crossref, Medline, Google Scholar
58. Nagase I, Yoshida T, Kumamoto K, Umekawa T, Sakane N, Nikami H, Kawada T, Saito M: Expression of uncoupling protein in skeletal muscle and white fat of obese mice treated with thermogenic beta3-adrenergic agonist. J Clin Invest 1996; 97:2898–2904Crossref, Medline, Google Scholar
59. Kirchberger MA: Excitation and contraction of skeletal muscle, in Best and Taylor’s Physiological Basis of Medical Practice, 12th ed. Edited by West JB. Baltimore, Williams & Wilkins, 1990, pp 62–107Google Scholar
60. Clausen T, van Hardeveld C, Everts ME: Significance of cation transport in control of energy metabolism and thermogenesis. Physiol Rev 1991; 71:733–774Crossref, Medline, Google Scholar
61. Gergely J: Biochemical aspects of muscular structure and function, in Disorders of Voluntary Muscle, 4th ed. Edited by Walton J. London, Longman Group, 1981, pp 102–150Google Scholar
62. Satinoff E: Neural organization and evolution of thermal regulation in mammals: several hierarchically arranged integrating systems may have evolved to achieve precise thermoregulation. Science 1978; 201:16–22Crossref, Medline, Google Scholar
63. Bligh J: The central neurology of mammalian thermoregulation. Neuroscience 1979; 4:1213–1236Crossref, Medline, Google Scholar
64. Boulant JA: Cellular and synaptic mechanisms of thermosensitivity in hypothalamic neurons, in Thermal Balance in Health and Disease: Recent Basic Research and Clinical Progress. Edited by Zeisberger E, Schonbaum E, Lomax P. Basel, Switzerland, Birkhauser Verlag, 1994, pp 19–29Google Scholar
65. Boulant JA: Hypothalamic mechanisms in thermoregulation. Fed Proc 1981; 40:2843–2850Medline, Google Scholar
66. Zeisberger E: Central modulators of thermoregulation. J Basic Clin Physiol Pharmacol 1990; 1:277–289Crossref, Medline, Google Scholar
67. Lance JW, McLeod JG: Autonomic nervous system, in A Physiologic Approach to Clinical Neurology, 3rd ed. London, Butterworths, 1981, pp 263–285Google Scholar
68. Burton H: Responses of spinal cord neurons to systematic changes in hindlimb skin temperatures in cats and primates. J Neurophysiol 1975; 38:1060–1079Crossref, Medline, Google Scholar
69. Moltz H: Fever: causes and consequences. Neurosci Biobehav Rev 1993; 17:237–269Crossref, Medline, Google Scholar
70. Kurz A, Sessler DI, Schroeder M, Kurz M: Thermoregulatory response thresholds during spinal anesthesia. Anesth Analg 1993; 77:721–726Medline, Google Scholar
71. Yehuda S, Wurtman RJ: Release of brain dopamine as the probable mechanism for the hypothermic effect of d-amphetamine. Nature 1972; 240:477–478Crossref, Medline, Google Scholar
72. Youdim MBH, Yehuda S, Ben-Uriah Y: Iron deficiency-induced circadian rhythm reversal of dopaminergic-mediated behaviors and thermoregulation in rats. Eur J Pharmacol 1981; 74:295–301Crossref, Medline, Google Scholar
73. Verma A, Kulkarni SK: Differential role of dopamine receptor subtypes in thermoregulation and stereotypic behavior in naive and reserpinized rats. Arch Int Pharmacodyn 1993; 324:17–32Medline, Google Scholar
74. Spivak B, Weizman A, Wolovick L, Hermesh H, Tyano S, Munitz H: Neuroleptic malignant syndrome during abrupt reduction of neuroleptic treatment. Acta Psychiatr Scand 1990; 81:168–169Crossref, Medline, Google Scholar
75. Cape G: Neuroleptic malignant syndrome—a cautionary tale and a surprising outcome. Br J Psychiatry 1994; 164:120–122Crossref, Medline, Google Scholar
76. Kurlan R, Hamill R, Shoulson I: Review: neuroleptic malignant syndrome. Clin Neuropharmacol 1984; 7:109–120Crossref, Medline, Google Scholar
77. Noto T, Hashimoto H, Sugae S, Okamoto K, Nakao J, Kamimura H, Nakajima T: Hypothermia caused by antipsychotic drugs in a schizophrenic patient. J Clin Psychiatry 1987; 48:77–78Medline, Google Scholar
78. Mills DE, Robertshaw D: Response of plasma prolactin to changes in ambient temperature and humidity in man. J Clin Endocrinol Metab 1981; 52:279–283Crossref, Medline, Google Scholar
79. Kennedy MS, Burks TF: Dopamine receptors in the central thermoregulatory mechanisms of the cat. Neuropharmacology 1974; 13:119–128Crossref, Medline, Google Scholar
80. Cairns SP, Dulhunty AF: The effects of beta-adrenoceptor activation on contraction in isolated fast- and slow-twitch skeletal muscle fibers of the rat. Br J Pharmacol 1993; 110:1133–1141Crossref, Medline, Google Scholar
81. Garcia MC, Escamilla-Sanchez J: Positive inotropic effect of adrenaline on potassium contractures in tonic skeletal muscle fibres of the frog. Can J Physiol Pharmacol 1994; 72:1580–1585Crossref, Medline, Google Scholar
82. Zacharova D, Lipska E, Hencek M, Hochmannova J, Sajter V: Modulation by adrenaline of electrophysiological membrane parameters and contractility in intact and internally perfused single muscle fibers of the crayfish. Gen Physiol Biophys 1993; 12:543–577Medline, Google Scholar
83. Grassi C, Deriu F, Roatta S, Santarelli R, Azzena GB, Passatore M: Sympathetic control of skeletal muscle function: possible co-operation between noradrenaline and neuropeptide Y in rabbit jaw muscles. Neurosci Lett 1996; 212:204–208Crossref, Medline, Google Scholar
84. Leijten P, Saida K, van Breemen C: Norepinephrine‐induced intracellular Ca2+ release from vascular smooth muscle. J Cardiovasc Pharmacol 1985; 7(suppl 6):S38–S42Google Scholar
85. Fletcher JE, Tripolitis L, Erwin K, Hanson S, Rosenberg H, Conti PA, Beech J: Fatty acids modulate calcium‐induced calcium release from skeletal muscle heavy sarcoplasmic reticulum fractions: implications for malignant hyperthermia. Biochem Cell Biol 1990; 68:1195–1201Crossref, Medline, Google Scholar
86. Kowarski D, Shuman H, Somlyo AP, Somlyo AV: Calcium release by noradrenaline from central sarcoplasmic reticulum in rabbit main pulmonary artery smooth muscle. J Physiol (Lond) 1985; 366:153–175Crossref, Google Scholar
87. Janiak R, Lewartowski B: Early after‐depolarizations induced by noradrenaline may be initiated by calcium released from sarcoplasmic reticulum. Mol Cell Biochem 1996; 163/164:125–130Google Scholar
88. Lorkovic H: Acetylcholine contractures of skeletal muscles: inhibition by chlorpromazine and diltiazem. Neuropharmacology 1995; 34:695–700Crossref, Medline, Google Scholar
89. Landsberg L, Saville ME, Young JB: Sympathoadrenal system and regulation of thermogenesis. Am J Physiol 1984; 247(2, part 1):E181–E189Google Scholar
90. Astrup A, Bulow J, Madsen J, Christensen NJ: Contribution of BAT and skeletal muscle to thermogenesis induced by ephedrine in man. Am J Physiol 1985; 248(5, part 1):E507–E515Google Scholar
91. Kurpad AV, Kulkarni RN, Rodriguez D, Shetty PS: Characteristics of norepinephrine stimulated thermogenesis in undernourished subjects. J Biosci 1992; 17:293–303Crossref, Google Scholar
92. Simon HB: Current concepts: hyperthermia. N Engl J Med 1993; 329:483–487Crossref, Medline, Google Scholar
93. Burdet L, de Muralt B, Schutz Y, Fitting J-W: Thermogenic effect of bronchodilators in patients with chronic obstructive pulmonary disease. Thorax 1997; 52:130–135Crossref, Medline, Google Scholar
94. Wheeldon NM, McDevitt DG, Lipworth BJ: Do beta3-adrenoceptors mediate metabolic responses to isoprenaline? Q J Med 1993; 86:595–600Google Scholar
95. Ye J-M, Edwards SJ, Rose RW, Steen JT, Clark MG, Colquhoun EQ: Alpha-adrenergic stimulation of thermogenesis in a rat kangaroo (Marsupialia, Bettongia gaimardi). Am J Physiol 1996; 271(3, part 2):R586–R592Google Scholar
96. Caroff SN: The neuroleptic malignant syndrome. J Clin Psychiatry 1980; 41:79–83Medline, Google Scholar
97. Shalev A, Munitz H: The neuroleptic malignant syndrome: agent and host interaction. Acta Psychiatr Scand 1986; 73:337–347Crossref, Medline, Google Scholar
98. Rosebush P, Stewart T: A prospective analysis of 24 episodes of neuroleptic malignant syndrome. Am J Psychiatry 1989; 146:717–725Link, Google Scholar
99. Addonizio G, Susman VL, Roth SD: Neuroleptic malignant syndrome: review and analysis of 115 cases. Biol Psychiatry 1987; 22:1004–1020Crossref, Medline, Google Scholar
100. Levenson JL: Neuroleptic malignant syndrome. Am J Psychiatry 1985; 142:1137–1145Link, Google Scholar
101. Modestin J, Toffler G, Drescher JP: Neuroleptic malignant syndrome: results of a prospective study. Psychiatry Res 1992; 44:251–256Crossref, Medline, Google Scholar
102. White DAC, Robins AH: Catatonia: harbinger of the neuroleptic malignant syndrome. Br J Psychiatry 1991; 158:419–421Crossref, Medline, Google Scholar
103. Taylor MA: Catatonia: a review of a behavioral neurologic syndrome. Neuropsychiatry, Neuropsychology and Behavioral Neurology 1990; 3:48–72Google Scholar
104. Northoff G: Neuroleptic malignant syndrome and catatonia: one entity or two? Biol Psychiatry 1996; 40:431–432Google Scholar
105. Addonizio G, Susman VL, Roth SD: Symptoms of neuroleptic malignant syndrome in 82 consecutive inpatients. Am J Psychiatry 1986; 143:1587–1590Link, Google Scholar
106. Keck PE Jr, Pope HG Jr, Cohen BM, McElroy SL, Nierenberg AA: Risk factors for neuroleptic malignant syndrome. Arch Gen Psychiatry 1989; 46:914–918Crossref, Medline, Google Scholar
107. Veith RC, Lewis N, Linares OA, Barnes RF, Raskind MA, Villacres EC, Murburg MM, Ashleigh EA, Castillo S, Peskind ER, Pascualy M, Halter JB: Sympathetic nervous system activity in major depression: basal and desipramine-induced alterations in plasma norepinephrine kinetics. Arch Gen Psychiatry 1994; 51:411–422Crossref, Medline, Google Scholar
108. Maas JW, Katz MM, Koslow SH, Swann A, Davis JM, Berman N, Bowden CL, Stokes PE, Landis H: Adrenomedullary function in depressed patients. J Psychiatr Res 1994; 28:357–367Crossref, Medline, Google Scholar
109. Manchip SM, Hurel SJ: Rhabdomyolysis due to mania (letter). Br J Psychiatry 1995; 167:118Crossref, Medline, Google Scholar
110. Gjessing LR: A review of periodic catatonia. Biol Psychiatry 1974; 8:23–45Medline, Google Scholar
111. Wheeler AH, Ziegler MG, Insel PA, Motulsky HJ: Episodic catatonia, hypertension, and tachycardia: elevated plasma catecholamines. Neurology 1985; 35:1053–1055Crossref, Medline, Google Scholar
112. Velamoor VR, Norman RMG, Caroff SN, Mann SC, Sullivan KA, Antelo RE: Progression of symptoms in neuroleptic malignant syndrome. J Nerv Ment Dis 1994; 182:168–173Crossref, Medline, Google Scholar
113. Zubenko G, Pope HG Jr: Management of a case of neuroleptic malignant syndrome with bromocriptine. Am J Psychiatry 1983; 140:1619–1620Link, Google Scholar
114. Weinberg SE, Twerski RS: Neuroleptic malignant syndrome. Anesth Analg 1983; 62:848–850Crossref, Medline, Google Scholar
115. Price DK, Turnbull GJ, Gregory RP, Stevens DG: Neuroleptic malignant syndrome in a case of post-partum psychosis. Br J Psychiatry 1989; 155:849–852Crossref, Medline, Google Scholar
116. Singh SP, Giridhar C, Avasthi A: Neuroleptic malignant syndrome with trifluperidol. Br J Psychiatry 1989; 155:561–563Crossref, Medline, Google Scholar
117. Price WA, Giannini AJ: A paradoxical response to chlorpromazine—a possible variant of the neuroleptic malignant syndrome. J Clin Pharmacol 1983; 23:567–569Crossref, Medline, Google Scholar
118. Guze BH, Baxter LR Jr: Current concepts: neuroleptic malignant syndrome. N Engl J Med 1985; 313:163–166Crossref, Medline, Google Scholar
119. Cryer PE: Physiology and pathophysiology of the human sympathoadrenal neuroendocrine system. N Engl J Med 1980; 303:436–444Crossref, Medline, Google Scholar
120. Adityanjee PD, Chawla HM: Neuroleptic malignant syndrome and psychotic illness. Br J Psychiatry 1989; 155:852–854Crossref, Medline, Google Scholar
121. Santagostino G, Amoretti G, Frattini P, Zerbi F, Cucchi ML, Preda S, Corona GL: Catecholaminergic, neuroendocrine and anxiety responses to acute psychological stress in healthy subjects: influence of alprazolam administration. Neuropsychobiology 1996; 34:36–43Crossref, Medline, Google Scholar
122. Fukuda M, Hata A, Niwa S-I, Hiramatsu K-I, Honda H, Nakagome K, Iwanami A: Plasma vanillylmandelic acid level as an index of psychological stress response in normal subjects. Psychiatry Res 1996; 63:7–16Crossref, Medline, Google Scholar
123. Meltzer HY: Neuromuscular dysfunction in schizophrenia. Schizophr Bull 1976; 2:106–135Crossref, Medline, Google Scholar
124. Mann SC, Caroff SN, Bleier HR, Welz WKR, Kling MA, Hayashida M: Lethal catatonia. Am J Psychiatry 1986; 143:1374–1381Link, Google Scholar
125. Wolff SM, Adler RC, Buskirk ER, Thompson RH: A syndrome of periodic hypothalamic discharge. Am J Med 1964; 36:956–967Crossref, Medline, Google Scholar
126. Armen R, Kanel G, Reynolds T: Phencyclidine-induced malignant hyperthermia causing submassive liver necrosis. Am J Med 1984; 77:167–172Crossref, Medline, Google Scholar
127. Gurrera RJ, Chang SS: Thermoregulatory dysfunction in neuroleptic malignant syndrome. Biol Psychiatry 1996; 39:207–212Crossref, Medline, Google Scholar
128. Schmidt KD, Chan CW: Thermoregulation and fever in normal persons and in those with spinal cord injuries. Mayo Clin Proc 1992; 67:469–475Crossref, Medline, Google Scholar
129. Gurrera RJ: Diaphoresis and dehydration during neuroleptic malignant syndrome: preliminary findings. Psychiatry Res 1996; 64:137–145Crossref, Medline, Google Scholar
130. Chayasirisobhon S, Cullis P, Veeramasuneni RR: Unusual case reports: occurrence of neuroleptic malignant syndrome in a narcoleptic patient. Hosp Community Psychiatry 1983; 34:548–550Abstract, Google Scholar
131. Henderson VW, Wooten GF: Neuroleptic malignant syndrome: a pathogenetic role for dopamine receptor blockade? Neurology (NY) 1981; 31:132–137Google Scholar
132. Goldwasser HD, Hooper JF, Spears NM: Concomitant treatment of neuroleptic malignant syndrome and psychosis. Br J Psychiatry 1989; 154:102–104Crossref, Medline, Google Scholar
133. Hoffman WH, Chodoroff G, Piggott LR: Haloperidol and thyroid storm. Am J Psychiatry 1978; 135:484–486; correction, 135:762Link, Google Scholar
134. Conlon P: The spectrum concept of neuroleptic toxicity (letter). Am J Psychiatry 1986; 143:811Medline, Google Scholar
135. Dhib‐Jalbut S, Hesselbrock R, Mouradian MM, Means ED: Bromocriptine treatment of neuroleptic malignant syndrome. J Clin Psychiatry 1987; 48:69–73Medline, Google Scholar
136. Martin DT, Swash M: Muscle pathology in the neuroleptic malignant syndrome. J Neurol 1987; 235:120–121Crossref, Medline, Google Scholar
137. Pearlman C, Wheadon D, Epstein S: Creatine kinase elevation after neuroleptic treatment. Am J Psychiatry 1988; 145:1018–1019Link, Google Scholar
138. Meltzer HY, Cola PA, Parsa M: Marked elevations of serum creatine kinase activity associated with antipsychotic drug treatment. Neuropsychopharmacology 1996; 15:395–405Crossref, Medline, Google Scholar
139. Scelsa SN, Simpson DM, McQuistion HL, Fineman A, Ault K, Reichler B: Clozapine-induced myotoxicity in patients with chronic psychotic disorders. Neurology 1996; 47:1518–1523Crossref, Medline, Google Scholar
140. van Kammen DP, Marder SR: Dopamine receptor antagonists, in Comprehensive Textbook of Psychiatry, 6th ed, vol 2. Edited by Kaplan HI, Sadock BJ. Baltimore, Williams & Wilkins, 1995, pp 1987–2022Google Scholar
141. Popli AP, Konicki PE, Jurjus GJ, Fuller MA, Jaskiw GE: Clozapine and associated diabetes mellitus. J Clin Psychiatry 1997; 58:108–111Crossref, Medline, Google Scholar
142. Keshavan MS, Stecker J, Kambhampati RK: Creatine kinase elevations with clozapine. Br J Psychiatry 1994; 164:118–120Crossref, Medline, Google Scholar
143. van Vliet PD, Burchell HB, Titus JL: Focal myocarditis associated with pheochromocytoma. N Engl J Med 1966; 274:1102–1108Crossref, Medline, Google Scholar
144. Guthrie RM, Lott JA: Abnormal serum creatine kinase and MB fraction following an amitriptyline overdose. J Fam Pract 1986; 22:554–555Google Scholar
145. Maguire JF, Geha RS, Umetsu DT: Myocardial specific creatine phosphokinase isoenzyme elevation in children with asthma treated with intravenous isoproterenol. J Allergy Clin Immunol 1986; 78:631–636Crossref, Medline, Google Scholar
146. Bhatnagar D, Carey P, Pollard A: Focal myositis and elevated creatine kinase levels in a patient with pheochromocytoma. Postgrad Med J 1986; 62:197–198Crossref, Medline, Google Scholar
147. Shemin D, Cohn PS, Zipin SB: Pheochromocytoma presenting as rhabdomyolysis and acute myoglobinuric renal failure. Arch Intern Med 1990; 150:2384–2385Crossref, Medline, Google Scholar
148. Newman M, Adityanjee, Jampala C: Atypical neuroleptic malignant syndrome associated with risperidone treatment (letter). Am J Psychiatry 1997; 154:1475Link, Google Scholar
149. Marsh SJ, Dolson GM: Rhabdomyolysis and acute renal failure during high-dose haloperidol therapy. Ren Fail 1995; 17:475–478Crossref, Medline, Google Scholar
150. Gurrera R, Romero J: Enzyme elevations in the neuroleptic malignant syndrome. Biol Psychiatry 1993; 34:634–640Crossref, Medline, Google Scholar
151. Pappas NJ Jr: Theoretical aspects of enzymes in diagnosis: why do serum enzymes change in hepatic, myocardial, and other diseases? Clin Lab Med 1989; 9:595–626Google Scholar
152. Wrogemann K, Pena SDJ: Mitochondrial calcium overload: a general mechanism for cell-necrosis in muscle diseases. Lancet 1976; 1:672–674Crossref, Medline, Google Scholar
153. Bloom S: Catecholamine cardiomyopathy (letter). N Engl J Med 1987; 317:900–901Crossref, Medline, Google Scholar
154. Sandusky GE, Means JR, Todd GC: Comparative cardiovascular toxicity in dogs given inotropic agents by continuous intravenous infusion. Toxicol Pathol 1990; 18:268–278Crossref, Medline, Google Scholar
155. Dhalla KS, Rupp H, Beamish RE, Dhalla NS: Mechanisms of alterations in cardiac membrane Ca2+ transport due to excess catecholamines. Cardiovasc Drugs Ther 1996; 10(suppl 1):231–238Google Scholar
156. Downey GP, Rosenberg M, Caroff S, Beck S, Rosenberg H, Gerber JC, Heiman-Patterson TD, Aronson MD: Neuroleptic malignant syndrome: patient with unique clinical and physiologic features. Am J Med 1984; 77:338–340Crossref, Medline, Google Scholar
157. Jones EM, Dawson A: Neuroleptic malignant syndrome: a case report with post-mortem brain and muscle pathology. J Neurol Neurosurg Psychiatry 1989; 52:1006–1009Crossref, Medline, Google Scholar
158. Felten DL, Felten SY, Carlson SL, Olschowka JA, Livnat S: Noradrenergic and peptidergic innervation of lymphoid tissue. J Immunol 1985; 135(2 suppl):755s–765sGoogle Scholar
159. Guyton AC: Resistance of the body to infection—the leukocytes, the tissue macrophage system, and inflammation, in Textbook of Medical Physiology, 6th ed. Philadelphia, WB Saunders, 1981, pp 65–73Google Scholar
160. Okamoto S, Ibaraki K, Hayashi S, Saito M: Ventromedial hypothalamus suppresses splenic lymphocyte activity through sympathetic innervation. Brain Res 1996; 739:308–313Crossref, Medline, Google Scholar
161. de Boer C, Gaete HP: Neuroleptic malignant syndrome and diabetic keto-acidosis. Br J Psychiatry 1992; 161:856–858Crossref, Medline, Google Scholar
162. Steinberg D: The endocrine pancreas, in Best and Taylor’s Physiological Basis of Medical Practice, 12th ed. Edited by West JB. Baltimore, MD, Williams & Wilkins, 1990, pp 754–769Google Scholar
163. Porte D Jr, Woods SC: Neural regulation of islet hormones and its role in energy balance and stress hyperglycemia, in Diabetes Mellitus: Theory and Practice, 4th ed. Edited by Rifkin H, Porte D Jr. New York, Elsevier, 1990, pp 175–197Google Scholar
164. Sherman CB, Hashimoto F, Davidson EJ: Gas‐producing Escherichia coli fasciitis in a patient with the neuroleptic malignant syndrome (letter). JAMA 1983; 250:361Crossref, Medline, Google Scholar
165. Eles GR, Songer JE, DiPette DJ: Neuroleptic malignant syndrome complicated by disseminated intravascular coagulation. Arch Intern Med 1984; 144:1296–1297Crossref, Medline, Google Scholar
166. Feneyrou B, Alauzen M, Bourgine N, Carabalona P: Colite necrosante due aux neuroleptiques (Necrotizing colitis due to neuroleptics). Gastroenterol Clin Biol 1985; 9:635–636Medline, Google Scholar
167. Otani K, Horiuchi M, Kondo T, Kaneko S, Fukushima Y: Is the predisposition to neuroleptic malignant syndrome genetically transmitted? Br J Psychiatry 1991; 158:850–853Google Scholar