Relationship Between Dissociation, Childhood Sexual Abuse, Childhood Physical Abuse, and Mental Illness in a General Population Sample
Abstract
OBJECTIVE: The aim of this study was to examine the relationship between childhood sexual abuse, childhood physical abuse, current psychiatric illness, and measures of dissociation in an adult population. METHOD: The authors used a randomly selected sample of 1,028 individuals. Each subject completed a semistructured face-to-face interview that included measures of childhood sexual abuse, childhood physical abuse, DSM-III-R psychiatric diagnoses, and selected items from the Dissociative Experiences Scale. RESULTS: Many individuals experienced occasional dissociative symptoms, and 6.3% of the population suffered from three or more frequently occurring dissociative symptoms. Among these individuals, the rate of childhood sexual abuse was two and one-half times as high, the rate of physical abuse was five times as high, and the rate of current psychiatric disorder was four times as high as the respective rates for the other subjects. Logistic regression modeling showed that physical abuse and current psychiatric illness were directly related to a high rate of dissociative symptoms but sexual abuse was not. The influence of sexual abuse was due to its associations with current psychiatric illness and with childhood physical abuse. Childhood physical abuse was not directly related to current psychiatric illness. Its association appeared to be mediated by its link to childhood sexual abuse. CONCLUSIONS: This study confirms that a small proportion (approximately 6%) of the general population suffer from high levels of dissociative symptoms. It calls into question the hypothesized direct relationship between childhood sexual abuse and adult dissociative symptoms.
Dissociation is defined in DSM-IV as a disruption in the usually integrated functions of consciousness, memory, identity, and perception of the environment. Dissociative symptoms exist along a continuum, ranging from common experiences such as daydreaming and lapses in attention, through déjà vu phenomena, to a pathological failure to integrate thoughts, feelings, and actions (1). Dissociative symptoms have long been observed among patients with psychiatric illness. Systematic clinical surveys consistently show that around one-quarter of patients with psychiatric illness have a substantial level of dissociation (2–4). There have been two published surveys of dissociative symptoms in general population samples. These demonstrated that dissociative symptoms are common and that approximately 5% of the population suffer from high levels of dissociation (4, 5).
The hypothesis that dissociation occurs in response to trauma has a long tradition in psychiatry, beginning with Janet around the turn of the century (6). The belief is that trauma (particularly in childhood, when the capacity for dissociation may be at its highest) is responsible for inducing the defensive use of dissociative processes. The dissociation is initially used as a means of defense or an attempt to adapt to the pain; if the extent of the abuse is sufficient, then the dissociative response regularly becomes relied on as a defense mechanism and the individual's mental processes become intermittently fragmented (7).
While the past decade has seen a return to an atheo~retical descriptive perspective to depict most psychiatric symptoms, dissociation remains firmly linked with childhood trauma. Both childhood physical abuse and, more particularly, childhood sexual abuse have been said to be causally related to adult dissociative symptoms. This relationship has been studied in a variety of ways, and most studies indicate an association between proneness to dissociation and childhood abuse (2, 7–14). Although physical abuse has generally been reported to be linked with dissociative symptoms, not all studies show this (e.g., reference 14). Sexual abuse, on the other hand, is believed by many to be specifically causally linked with adult dissociative symptoms. This belief has now reached the point where some investigators assume the link has been satisfactorily demonstrated and focus their research on what characteristics of the abuse result in the use of dissociation (13). Other researchers, however, still argue about whether or not a direct link between early sexual trauma and markers of high dissociation has been compellingly established (15).
The reason for this confusion may be related to the research to date. Most studies of the relationship between childhood abuse and dissociation used clinical populations or nonclinical samples of undergraduate students. The samples were usually small and consisted only of females. The studies have used a variety of, sometimes nonstandardized, measures to quantify abuse, psychiatric illness, and dissociative experiences. Many studies have failed to control for the relationship between childhood physical and sexual abuse and their relationship to psychiatric illness, as well as to dissociative symptoms.
To try to better define the relationship of childhood sexual abuse, childhood physical abuse, psychiatric illness, and measures of dissociation, we used a large, randomly selected general population sample. We used standardized measures of childhood abuse, current psychiatric illness, and dissociative symptoms. We used logistic regression modeling to examine possible interrelationships between childhood abuse, psychiatric illness, and measures of dissociation. We wished to see whether there was a direct relationship between childhood abuse and dissociative symptom scores in adulthood. We were particularly interested in the relationship between sexual and physical abuse, the relationship between abuse and mental illness, and the relationship between mental illness and measures of dissociation.
METHOD
Sample
The subjects were recruited as a control group for a case-control study on suicide (16). They were randomly selected from electoral rolls for the Canterbury region of New Zealand. This is a mixed urban and rural area with a regional population of approximately 430,000. It has one city, Christchurch, with a population of 315,000. Official estimates from the National Electoral Roll Office are that 95.5% of the eligible population were enrolled on the Canterbury electoral rolls during data collection. An age- and gender-stratified sample was obtained, the selection being proportional to the known age and gender distribution of the population aged 18 years and over.
In total, 1,200 subjects were selected from electoral rolls for the population sample (no exclusion criteria were applied), and 1,028 subjects participated in the study. Ninety-three (7.8%) refused, 57 (4.8%) could not be traced, and 22 (1.8%) were unable to adequately complete the interview because of intellectual limitations, illness, or language problems. The response rate was therefore 85.7%.
Data Collection
After an introductory letter and discussion of the study, the subjects who agreed to participate were interviewed. A semistructured interview was conducted face to face with each subject by trained interviewers. The work was monitored closely, and all interviewers met weekly with the supervisor (A.L.B.) for debriefing, checking, and editing of each interview. A parallel interview was conducted with a “significant other” who knew the subject well and was nominated by the subject. This study was approved by the Ethics Committee of the Canterbury Area Health Board and the Southern Regional Health Authority. Written informed consent was obtained from all study participants after the aims and procedures of the study had been fully explained.
Measures
Dissociative symptoms. The Dissociative Experiences Scale is a 28-item self-report questionnaire that has been reported to be reliable, internally consistent, and temporally stable (17, 18). We modified it in the following ways. We used 15 items, selecting these on the basis of the face validity of individual items. Rather than a vertical slash on a continuous dimension we used a four-part scale labeled “i” (rarely or never), “ii” (occasionally), “iii” (often), and “iv” (always or almost always). Since this was part of a larger study in which subjects were interviewed, the subjects were asked about symptoms rather than being required to complete the Dissociative Experiences Scale as a self-report questionnaire.
Psychiatric diagnosis. The interview for each subject included questions from the Structured Clinical Interview for DSM-III-R—Patient Version (19) to generate DSM-III-R diagnoses of selected mental disorders. The information gathered from the subject and from the close friend or relative was integrated in a diagnostic conference to produce, for each subject, best-estimate diagnoses of mental disorders (according to DSM-III-R criteria). In this analysis the following diagnostic groups for disorders in the month before the interview were used: any mood disorder (major depression and bipolar disorder); any psychoactive substance use disorder (alcohol, cannabis, and other abuse or dependence); any anxiety disorder (panic disorder, agoraphobia, obsessive-compulsive disorder, simple phobia, social phobia); and posttraumatic stress disorder. The test-retest reliability of the best-estimate diagnostic procedure was ascertained by a reevaluation of 20% of the subjects. The test-retest agreement was high. The kappa coefficients (20) for the principal diagnostic categories (mood disorders, substance use disorders, anxiety disorders, posttraumatic stress disorder) ranged from 0.95 to 0.99.
Childhood sexual abuse. Each subject was asked whether or not during childhood he or she had been “physically or psychologically forced by anyone to engage in any unwanted sexual activity, sexually assaulted, or raped,” a definition previously used by Murphy (21). Subjects who responded positively to this question were then asked further questions relating to this activity (if they felt able to talk about the matter). Subjects were classified as having a history of childhood sexual abuse if they responded positively to the initial question and subsequent questioning established a history of childhood sexual abuse. The subjects were divided into three groups: those who had suffered no abuse or only noncontact abuse, those who had had contact abuse but not involving intercourse, and those whose sexual abuse involved attempted intercourse and/or actual intercourse.
Childhood physical abuse. The subjects were questioned as to whether or not they believed they had experienced physical abuse during childhood. The subjects who responded positively to this question were then asked to provide specific examples of the abusive behavior they had experienced. Subjects were classified as having a history of physical abuse if they responded positively to the initial question and the responses to subsequent questions established a history of physical abuse.
RESULTS
Dissociative Symptoms
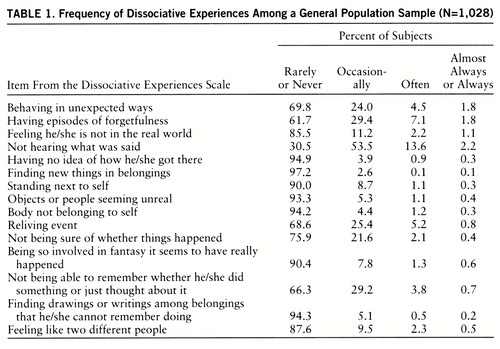
Table 1 shows the base frequencies of the Dissociative Experiences Scale symptoms in the general population sample. Most symptoms were rarely or never experienced, with the exception of not hearing what was said, which is, not surprisingly, occasionally experienced by 53.5% of normal individuals. Few people always or almost always experience dissociative symptoms.
To represent variation in dissociation scores, the items in table 1 were summed to produce, for each subject, an overall dissociation score. The reliability of this score was assessed by coefficient alpha (22) and was found to be acceptable (alpha=0.78). However, for the purposes of the subsequent analysis it was found useful to dichotomize these scores so as to divide the subjects into those having marked symptoms of dissociation and those without high symptom levels. Previous studies have suggested that approximately 5% of the population suffer from high levels of dissociation, and we found that using a criterion of three dissociative symptoms (occurring often, almost always, or always) resulted in classification of 6.3% of the sample as having high dissociation scores. Among those classified as having high dissociation scores, the mean number of dissociation symptoms was 4.77, and the range was three to 13.
Characteristics of Subjects With High Dissociation Scores
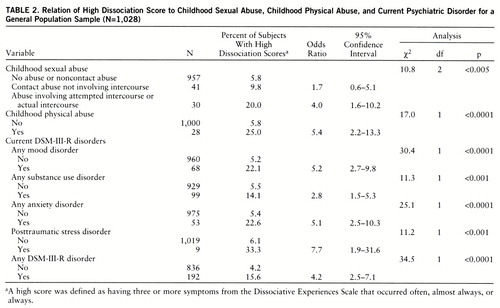
Table 2 shows the relationship of childhood sexual abuse, childhood physical abuse, and the selected DSM-III-R disorders to a high dissociation score (i.e., three or more symptoms occurring often, almost always, or always). Each comparison was tested for statistical significance by using the chi-square test of independence, and the test of association between a high dissociation score and each risk factor was made by using the odds ratio and 95% confidence interval. The odds ratio for any childhood contact sexual abuse (i.e., including both contact abuse not involving intercourse and abuse involving attempted or actual intercourse) was 2.6 (confidence interval=1.3–5.4).
The table shows that the rate of high dissociation scores was significantly higher among the individuals reporting childhood physical abuse and childhood sexual abuse than among the other subjects.
In addition, the subjects who met the DSM-III-R criteria for a current mental disorder (any mood disorder, any substance use disorder, any anxiety disorder, or posttraumatic stress disorder) also showed higher rates of high dissociation scores. The odds ratios for the specific diagnostic groups ranged from 2.8 (for any substance use disorder) to 7.7 (for posttraumatic stress disorder).
In general, these results clearly suggest that the odds of having a high dissociation score were high for individuals reporting a history of childhood abuse and for those with a current mental disorder.
Links Among Childhood Abuse, Mental Disorder, and Dissociation
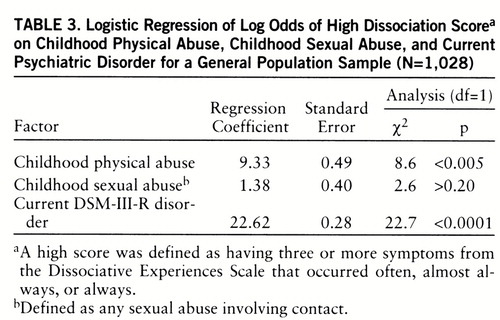
To explore the relationships between high dissociation score, childhood abuse, and current psychiatric disorder, a logistic regression model was fitted to the data. The log odds of a high dissociation score was modeled as a linear function of exposure to childhood sexual abuse, exposure to childhood physical abuse, and current mental disorder. Age and gender were entered into the equation to take account of possible variations. The results of this analysis are shown in table 3, which shows, for each predictor variable 1) the logistic regression coefficient, 2) the standard error of the logistic regression coefficient, and 3) the results of the log likelihood ratio chi-square test of significance of the regression coefficient.
The table shows that both childhood physical abuse and current mental disorder were predictive of high dissociation. However, childhood sexual abuse was unrelated to dissociation score when due allowance was made for current mental disorder and childhood physical abuse.
To examine why childhood sexual abuse was not predictive of a high dissociation score when allowance was made for current mental disorder and childhood physical abuse, the data were further analyzed by using log linear modeling methods. This analysis suggested that linkages between childhood sexual abuse and dissociation arose by two indirect routes:
1. Childhood sexual abuse was related to current mental state (χ2=18.0, df=1, p<0.0001), which was in turn related to dissociation (χ2=22.7, df=1, p<0.0001).
2. Childhood sexual abuse was related to childhood physical abuse (χ2=11.0, df=1, p<0.005), which was in turn related to dissociation (χ2=8.6, df=1, p<0.005).
When these indirect linkages between childhood sexual abuse and high dissociation score were taken into account, childhood sexual abuse had no direct effect on dissociation score (χ2=2.6, df=1, p>0.20). Substantively, these results suggest that childhood sexual abuse was unrelated to the level of dissociation when allowance was made for the linkages between 1) childhood sexual abuse and current mental disorder and 2) childhood sexual abuse and childhood physical abuse.
DISCUSSION
In this study, childhood sexual abuse, childhood physical abuse, and current psychiatric illness were all related to high scores on the Dissociative Experiences Scale. However, when multivariate methods were used to explore the relationships between these factors, some surprising effects emerged. The effects of sexual abuse were not direct but were due to the association of childhood sexual abuse with current psychiatric disorder and the association of childhood sexual abuse with childhood physical abuse. Childhood physical abuse, on the other hand, was directly related to high scores on the Dissociative Experiences Scale. It is also clear that having current psychiatric illness is strongly related to high dissociative symptom scores.
These findings call into question the hypothesized direct effects of childhood sexual abuse on dissociation and suggest that any causal influence of childhood sexual abuse on dissociation is likely to be indirect and mediated by more general linkages between childhood sexual abuse and risks of mental disorder. These findings contradict most published results from studies that have looked at this relationship. An important reason for this may be that our study is one of few, to our knowledge, that have examined this relationship in randomly selected general population samples. Using a clinical sample, as most studies have done, may introduce substantial bias. It is possible that individuals with childhood sexual abuse and psychiatric symptoms are more likely to seek treatment than those who suffer similar symptoms but have not been sexually abused. It has also been suggested that treatment for sexual abuse may produce an increase of dissociative symptoms, giving rise to an apparent but spurious relationship. Using student groups, as some studies have done, also introduces bias: students are not representative of a general population and may self-select for certain courses.
In addition, few studies have examined the effect of current psychiatric illness on dissociative symptoms. This is surprising since there is consistent evidence that dissociative symptoms are highly correlated with psychopathology (2–4). It is likely that several of the items on the Dissociative Experiences Scale will be responded to positively by people suffering from anxiety or depressive disorders. Since most studies have shown that sexual abuse causes higher rates of psychiatric disorders in adults (23–25), persons with childhood sexual abuse will have higher scores on the Dissociative Experiences Scale. This relationship implies that the higher rate of dissociative symptoms among those exposed to childhood sexual abuse may reflect their greater vulnerability to psychiatric disorder in general rather than the direct and specific effects of childhood sexual abuse on dissociation.
One argument might be that our modifications of the Dissociative Experiences Scale might have influenced the results. We feel that this is unlikely; the proportion of individuals with high scores on the Dissociative Experiences Scale in our study was similar to previously reported rates for community samples (4, 5), and the questions we chose were evenly distributed among the three factors reported by the authors of these studies (26). Interviewing patients, rather than using a self-report method, may enhance the validity of the answers. Horen et al. (11), for example, suggested that many patients have difficulty completing the self-administered Dissociative Experiences Scale, and these authors commented that this problem was not well addressed.
A more provocative argument is that the Dissociative Experiences Scale is an unsuitable instrument for measuring dissociation. Our study cannot address this issue, but it is important to note that the Dissociative Experiences Scale is considered a reliable and valid way to measure dissociation in many groups (17, 18), that it performs well as a screening instrument for dissociative disorders (5, 26), and that it has been used in most studies linking sexual abuse to dissociative symptoms (e.g., references 2, 8–11, 13).
It is also possible that our definition of sexual abuse may have influenced the findings. We believe that our rather narrow view of what constituted sexual abuse (i.e., confining our analysis to contact abuse) should have strengthened rather than weakened any potential direct relationship between sexual abuse and dissociation scores.
Waller et al. (27) recently rescaled the Dissociative Experiences Scale to produce an eight-item scale that may more accurately reflect pathological dissociation. Since six of their criteria were also included in the 15 items we used, we reanalyzed the data by using these six items to check our association. The result was that the association between dissociation and childhood sexual abuse (any contact sexual abuse) was smaller and, in fact, no longer significant (odds ratio=2.1, 95% confidence interval=0.9–4.7, p>0.05).
In summary, this study replicates the two previous general population studies using the Dissociative Experiences Scale. It shows that dissociative symptoms as measured by the Dissociative Experiences Scale are common and that approximately 6% of the population have three or more frequently occurring symptoms. These individuals also have higher rates of childhood physical abuse, childhood sexual abuse, and current psychiatric illness. When the associations between these factors are allowed for, the hypothesized direct relationship between childhood sexual abuse and dissociative symptoms is not present. This association is due to the relationships of sexual abuse to physical abuse and to psychiatric illness. Childhood physical abuse and current psychiatric illness each has a strong direct association with high dissociation scores. Because our sample was a large randomly selected community sample, we believe that these results need to be carefully considered.
 |
 |
 |
Received Dec. 16, 1996; revision received Aug. 15, 1997; accepted Dec. 1, 1997. From the Department of Psychological Medicine and the Christchurch Health and Development Study, Christchurch School of Medicine. Address reprint requests to Dr. Mulder, Department of Psychological Medicine, Christchurch School of Medicine, P.O. Box 4345, Christchurch, New Zealand.
1 Atchison M, McFarlane AC: A review of dissociation and dissociative disorders. Aust NZ J Psychiatry 1994; 28:591–599Crossref, Medline, Google Scholar
2 Saxe GN, van der Kolk BA, Berkowitz R, Chinman G, Hall K, Lieberg G, Schwartz J: Dissociative disorders in psychiatric inpatients. Am J Psychiatry 1993; 150:1037–1042Link, Google Scholar
3 Rauschenberger SL, Lynn SJ: Fantasy proneness, DSM-III-R axis I psychopathology, and dissociation. J Abnorm Psychol 1995; 194:373–380Crossref, Google Scholar
4 Putnam FW, Carlson EB, Ross CA, Anderson G, Clark P, Torem M, Bowman ES, Coons P, Chu JA, Dill L, Loewenstein RJ, Braun BG: Patterns of dissociation in clinical and nonclinical samples. J Nerv Ment Dis 1996; 184:673–679Crossref, Medline, Google Scholar
5 Ross CA, Joshi S, Currie R: Dissociative experiences in the general population. Am J Psychiatry 1990; 147:1547–1552Link, Google Scholar
6 van der Kolk BA, van der Hart O: The dissociation theory of Pierre Janet. J Traumatic Stress 1989; 2:397–412Crossref, Google Scholar
7 Irwin HJ: Proneness to dissociation and traumatic childhood events. J Nerv Ment Dis 1994; 182:456–460Crossref, Medline, Google Scholar
8 Kirby JS, Chu JA, Dill DL: Correlates of dissociative symptomatology in patients with physical and sexual abuse histories. Compr Psychiatry 1993; 34:258–263Crossref, Medline, Google Scholar
9 Zlotnick C, Shea MT, Zakriski A, Costello E, Begin A, Pearlstein T, Simpson E: Stressors and close relationships during childhood and dissociative experiences in survivors of sexual abuse among inpatient psychiatric women. Compr Psychiatry 1995; 36:207–212Crossref, Medline, Google Scholar
10 Chu JA, Dill DL: Dissociative symptoms in relation to childhood physical and sexual abuse. Am J Psychiatry 1990; 147:887–892Link, Google Scholar
11 Horen SA, Leichner PP, Lawson JS: Prevalence of dissociative symptoms and disorders in an adult psychiatric inpatient population in Canada. Can J Psychiatry 1995; 40:185–191Crossref, Medline, Google Scholar
12 DiTomasso MJ, Routh DK: Recall of abuse in childhood and three measures of dissociation. Child Abuse Negl 1993; 17:477–485Crossref, Medline, Google Scholar
13 Zlotnick C, Begin A, Shea MT, Pearlstein T, Simpson E, Costello E: The relationship between characteristics of sexual abuse and dissociative experiences. Compr Psychiatry 1994; 35:465–470Crossref, Medline, Google Scholar
14 Waldinger RJ, Swett C Jr, Frank A, Miller K: Levels of dissociation and histories of reported abuse among women outpatients. J Nerv Ment Dis 1994; 182:625–630Crossref, Medline, Google Scholar
15 Nash MR, Hulsey TL, Sexton MC, Harralson TL, Lambert W: Long-term sequelae of childhood sexual abuse: perceived family environment, psychopathology, and dissociation. J Consult Clin Psychol 1993; 61:276–283Crossref, Medline, Google Scholar
16 Beautrais AL, Joyce PR, Mulder RT, Fergusson DM, Deavoll BJ, Nightingale SK: Prevalence and comorbidity of mental disorders in persons making serious suicide attempts: a case-control study. Am J Psychiatry 1996; 153:1009–1014Link, Google Scholar
17 Bernstein EM, Putnam FW: Development, reliability, and validity of a dissociation scale. J Nerv Ment Dis 1986; 174:727–735Crossref, Medline, Google Scholar
18 Dubester KA, Braun BG: Psychometric properties of the Dissociative Experiences Scale. J Nerv Ment Dis 1995; 183:231–235Crossref, Medline, Google Scholar
19 Spitzer RL, Williams JBW, Gibbon M, First MB: Structured Clinical Interview for DSM-III-R—Patient Version (SCID-P). New York, New York State Psychiatric Institute, Biometrics Research, 1989Google Scholar
20 Fleiss JL: Statistical Methods for Rates and Proportions, 2nd ed. New York, John Wiley & Sons, 1981Google Scholar
21 Murphy JE: News release. St Cloud, Minn, St Cloud State University, June 1988Google Scholar
22 Cronbach LJ: Coefficient alpha and the internal structure of tests. Psychometrika 1951; 16:297–334Crossref, Google Scholar
23 Fergusson DM, Horwood LJ, Lynskey MT: Child sexual abuse and psychiatric disorders in young people, part II: psychiatric outcomes of childhood sexual abuse. J Am Acad Child Adolesc Psychiatry 1996; 35:1365–1374Crossref, Medline, Google Scholar
24 Mullen PE, Martin JL, Anderson JC, Romans SE, Herbison GP: Childhood sexual abuse and mental health in adult life. Br J Psychiatry 1993; 163:721–732Crossref, Medline, Google Scholar
25 Briere J, Runtz M: Symptomatology associated with child sexual victimisation in a nonclinical adult sample. Child Abuse Negl 1988; 12:51–59Crossref, Medline, Google Scholar
26 Ross CA, Joshi S, Currie R. Dissociative experiences in the general population: a factor analysis. Hosp Community Psychiatry 1991; 42:927–930Google Scholar
27 Waller NG, Putnam FW, Carlson EB: Types of dissociation and dissociative types: a taxometric analysis of dissociative experiences. Psychol Methods 1996; 1:300–321Crossref, Google Scholar



