Effects of Age at Onset of First Lifetime Episode of Recurrent Major Depression on Treatment Response and Illness Course in Elderly Patients
Abstract
OBJECTIVE: The goal of this study was to examine treatment outcome differences in relation to age at onset of first lifetime episode of recurrent major depression in elderly patients. METHOD: Patients were grouped as having early-onset (N=129) or late-onset (N=58) depression. Early onset was defined as having a first lifetime episode of major depression at age 59 or earlier; late onset was defined as age 60 or later. The two groups of patients were compared with respect to demographic and clinical characteristics, types of treatment given (nortriptyline and interpersonal psychotherapy), and treatment outcomes. RESULTS: The groups did not differ in the percentage of patients who remitted, recovered, or relapsed during continuation treatment or in the percentage who experienced a recurrence of major depression during the first year of maintenance treatment. However, early-onset patients took 5–6 weeks longer to achieve remission than did late-onset patients, and a higher proportion had a history of suicide attempts. CONCLUSIONS: These data suggest that age at lifetime onset of recurrent major depression does not influence short- or long-term treatment response in elderly patients treated with combined interpersonal psychotherapy and nortriptyline, with the exception of slowing the speed of remission in early-onset cases. Difference in remission speed may reflect the greater number of previous episodes in the early-onset patients. Nevertheless, the likelihood of a longer time to remission, together with a higher rate of past suicide attempts, suggests that elderly depressed patients with a history of early-onset illness need particularly careful management.
There has been conflicting evidence regarding the effect of age at onset of depression on the prognosis of elderly patients, as summarized by Cole in a 1990 review of 10 studies (1). More recently, Brodaty et al. (2) found that elderly patients who experienced their first lifetime episode of major depression before age 60 were more likely to have a relapsing course. The authors concluded that “a history of recurrence and its corollary, early-onset depression, not surprisingly, predicted a poorer prognosis in the elderly” (2, p. 594). Consistent with these results, we recently reported that elderly patients who were older when they experienced their first episode of depression showed a more rapid, sustained response profile (3). By contrast, other investigators (4) have observed that lifetime illness onset after age 60 predicts a less favorable treatment response, a more chronic course, and subsequent development of dementia. Other studies (5) have also suggested that onset after age 60 may presage a stormy illness course, with frequent and early relapses, perhaps as a result of brittle treatment response. Converging with this view are data showing an association of late-onset depression with brain abnormalities such as ventriculomegaly, white matter hyperintensities, and cognitive impairment (6, 7). Cognitive impairment in late-life and late-onset depression, even if reversed by antidepressant treatment, may presage the development of irreversible dementia.
The validity of these conclusions should be tested further by taking into account variability in treatment and in treatment compliance. Specifically, the use of highly standardized or controlled treatment, together with a high level of treatment compliance, would be expected to reduce the variance in illness course that might be observed (or that is more likely) with nonstandardized (naturalistic) treatment or with poor treatment compliance. One would thus be in a better position to examine the hypothesized influence of age at first onset of depression on treatment response and illness course in the context of a double-blind, placebo-controlled, longitudinal study.
Since 1989 we have been conducting a controlled examination of the long-term, or maintenance, efficacy of nortriptyline and interpersonal psychotherapy (8) for preventing recurrence of major depressive episodes in the elderly (the Pittsburgh study of maintenance therapies in late-life depression) (9). The data accrued as part of this study permit a test of the hypothesis that onset of first lifetime episode of major depressive illness after age 60 will adversely affect rate and speed of remission as well as rates of recovery, relapse, and recurrence. We recently reported that older age at study entry is associated with a slower speed and lower rate of treatment response (3). The question addressed by the present report concerns the hypothesized effect of age at onset of first lifetime illness on treatment response and course of illness.
METHOD
Subjects
Demographic characteristics. Data were available for all 187 elderly patients entered into the Pittsburgh study of maintenance therapies in late-life depression protocol from its inception on Feb. 1, 1989, to the close of intake 7 years later on Jan. 31, 1996 (intent-to-treat sample); 687 patients were screened to yield the final sample of 187. The major reasons for exclusion were 1) other psychiatric diagnosis (N=135); 2) major depressive disorder, single episode (N=119); 3) interepisode wellness interval greater than 2.5 years (N=63); 4) medical contraindications to use of nortriptyline (N=43); and 5) presence of delusional (N=24) or intermittent (N=23) depressive disorders. Patients meeting eligibility criteria entered the study after providing written informed consent following full explanation of procedures.
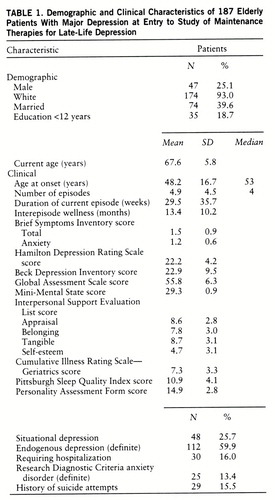
Demographic and clinical measures of the final study group are summarized in table 1. To be consistent with other reports in the literature (2, 4), we grouped patients by early versus late age at onset. Early onset was defined a priori as having a first lifetime episode of major depression at age 59 or earlier; late onset was defined as age 60 or later. All patients were required to have recurrent unipolar major depression (nonpsychotic), as determined by structured interview with the Schedule for Affective Disorders and Schizophrenia—Lifetime Version (SADS-L) (10). A score of 17 or higher on the 17-item Hamilton Depression Rating Scale (11) and a score of 27 or greater on the Folstein Mini-Mental State (12) were also required for study entry. There were 129 patients in the early-onset group and 58 in the late-onset group. The late-onset group were on average 3 years older than the early-onset group at study entry (mean=69.6, SD=5.8, versus mean=66.7, SD=5.6) (t=–3.2, df=185, p=0.002). The groups did not differ in sex, race, marital status, or years of education.
Clinical characteristics. The groups also were similar on most clinical characteristics, such as severity of current episode, percent who required hospitalization during acute treatment, percent with endogenous episodes, duration of episodes, length of wellness interval before the index episode, functional impairment, percent with lifetime histories of anxiety disorders, chronic medical illness burden, personality dysfunction, perceived interpersonal support, and self-reported sleep quality. With respect to specific organ system scores on the Cumulative Illness Rating Scale—Geriatrics (13), late-onset patients scored significantly higher on the measure of systemic vascular impairment (mean=1.2, SD=1.1, versus mean=0.8, SD=1.0) (t=–2.6, df=170, p=0.01) but lower on focal neurological impairment (mean=0.2, SD=0.6, versus mean=0.5, SD=0.8) (t=2.6, df=141, p=0.01).
By design, the groups differed in age at onset of first lifetime episode, with a group difference of 26 years: mean=40.2 (SD=13.4) versus mean=66.0 (SD=5.9) (t=–18.2, df=185, p=0.0001). Not surprisingly, early-onset patients reported a greater number of lifetime episodes of major depression: mean=5.8 (SD=5.1) versus mean=2.7 (SD=1.3) (t=6.5, df=160.9, p=0.0001). Therefore, we chose to use number of lifetime episodes (as well as age at study entry) as a covariate in the Cox proportional hazards model of time to remission to determine if any difference observed as a function of age at first illness onset remained after we controlled for difference in number of episodes and age at study entry. Finally, a higher proportion of early-onset patients reported a history of suicide attempts (22.5% [N=29] versus 1.7% [N=1]) (p=0.0006, Fisher's exact test).
Treatments
All subjects received nortriptyline ti~trated to plasma steady-state levels of 80–120 ng/ml. Final plasma nortriptyline steady-state levels did not differ between early-onset (mean=91.4 ng/ml, SD=26.1) and late-onset (mean=86.5 ng/ml, SD=24.8) groups (t=0.9, df=117, n.s.), but a significantly higher dose of nortriptyline was needed in the early-onset group (mean=84.6 mg/day, SD=34.9) than in the late-onset group (mean=67.0 mg/day, SD=22.9) (t=2.8, df=117, p=0.007), probably reflecting age-dependent differences in metabolic rate. (The early-onset group was younger at study entry than the late-onset group.) However, the groups did not differ in the time required to reach the 80 ng/ml threshold concentration, nor in the percentage who received adjunctive psy~chotropic medications. Thus, pharmaco~logical parity was achieved in the treatment of the two groups.
Similarly, all patients participated in weekly interpersonal psychotherapy for at least 12 consecutive weeks (8). The groups did not differ in the distribution of primary foci of interpersonal psychotherapy, such as bereavement, interpersonal conflict, or role transitions.
Definition of Primary Treatment Outcomes
With respect to the primary treatment outcome measures, we followed the convention of Frank et al. (14) for defining remission, recovery, relapse (during continuation therapy), and recurrence (during the first year of maintenance therapy). Specifically, after patients achieved a Hamilton depression score of 10 or less for 3 consecutive weeks, their index episodes were declared to be remitted. Patients with “partial” remission (N=6) were defined by a Hamilton score of 11–14 at the end of acute therapy. We chose a Hamilton score of 10 or less as the criterion for remission in order to be consistent with the geriatric literature (e.g., Georgotas et al. [15]; Frank et al. [14] used a score of 7 in midlife studies). A 16-week period of continuation therapy began, during which patients continued to receive the same dose of nortriptyline used during acute therapy and every-other-week interpersonal psychotherapy.
After completing 16 weeks of continuation pharmacotherapy and interpersonal psychotherapy, patients were declared “recovered,” as long as they had not experienced relapses of their major depressive episodes. Of the 187 patients who entered the study, 124 recovered and were randomly assigned to maintenance therapy (nortriptyline with monthly maintenance interpersonal psychotherapy, nortriptyline in a medication clinic without interpersonal psychotherapy, placebo with monthly maintenance interpersonal psychotherapy, or placebo in a medication clinic without interpersonal psychotherapy). There was no significant difference in the distribution of random maintenance treatment assignments across the two groups (χ2=1.65, df=3, p=0.65). Patients were seen monthly during double-blind, placebo-controlled maintenance therapy to determine continued wellness or the recurrence of a major depressive episode, defined by using the SADS-L and confirmed by an independent senior psychiatrist.
RESULTS
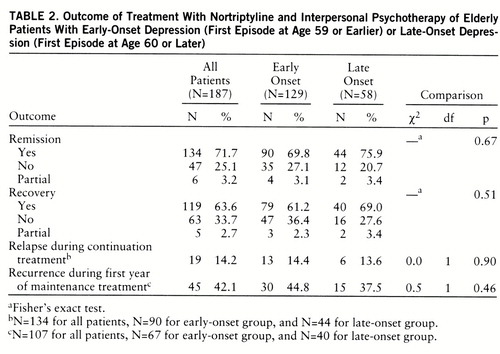
Early- and late-onset groups did not differ in absolute rates of remission, recovery, relapse (during 16 weeks of continuation therapy), or recurrence (during the first year of maintenance therapy) (table 2). However, the median time to remission of the index episode was significantly longer in the early-onset group (12.9 weeks) than in the late-onset group (7.3 weeks) (figure 1). This result remained significant after the number of episodes was used as a covariate in the Cox proportional hazards model: 11.6 weeks in early-onset patients compared with 9.0 weeks in late-onset patients (χ2=4.58, df=1, p=0.03). Age at study entry was not a significant covariate in the Cox proportional hazards model.
To examine further the relative influences of number of previous episodes and age at onset of first lifetime episode, we performed a median split of the early-onset group by number of lifetime episodes of major depression, comparing early-onset patients with four or fewer lifetime episodes and early-onset patients with more than four episodes. We then examined treatment outcomes, stratifying on two early-onset subgroups and the late-onset group. We detected no differences in percent of patients who remitted, recovered, relapsed, or experienced a recurrence. Kaplan-Meier survival analysis showed a median time to remission of 14 weeks in early-onset patients with more than four lifetime episodes, 11.0 weeks in early-onset patients with four or fewer episodes, and 7.3 weeks in late-onset patients (figure 2). There was a significant difference in remission times between the late-onset group and each of the two early-onset subgroups (Wilcoxon χ2=8.69, df=1, p=0.003, Wilcoxon χ2=6.82, df=1, p=0.009, respectively) but not between the two early-onset subgroups (Wilcoxon χ2=0.32, df=1, p=0.57).
DISCUSSION
The current data suggest that age at onset of first lifetime episode of recurrent major depression in elderly patients does not affect absolute rates of remission, relapse, recovery, or recurrence during the first year of maintenance therapy. However, they do suggest that early onset is associated with a slower speed of remission from the index episode. Patients with early-onset depression did not differ from those with late onset in treatment intensity or focus, either pharmacological or psychotherapeutic. It may be the similarity of combined treatment received that was the strongest determinant of similar outcomes.
Age at onset of first lifetime episode of depression is linked inextricably to the number of previous illness episodes, thus making it difficult (and perhaps impossible in clinical practice) to distinguish effects attributable to age at onset from those attributable to number of episodes (or chronicity of illness). Perhaps age at onset should be considered a proxy for other variables that can affect course of illness and treatment response. For example, later onset of depression has been associated with greater neuropsychological impairment and more structural brain abnormalities, with vascular and other medical diseases, and with a less frequent family history of mood disorders (4, 6, 7). In our study group, late-onset patients were characterized by higher levels of systemic vascular pathology and lower focal neurological impairment according to rating on the Cumulative Illness Rating Scale—Geriatrics than the early-onset group, but not by greater cognitive impairment or overall medical burden.
Our findings agree with those of Brodaty et al. (2), who also reported that early age at initial onset of depression predicted a worse outcome for elderly patients who go on to have recurrent depression. By contrast, Alexopoulos et al. (16) reported that late onset of first depressive episode in elderly patients is the strongest predictor of chronicity but that weak social support best predicts chronicity in younger patients. This pattern of discrepant results is probably due to differences in patient populations studied by Alexopoulos et al. and our current study (as well as the use of combined interpersonal psychotherapy and medication in a defined treatment protocol rather than naturalistic follow-up).
The patients studied by Alexopoulos et al. were older at study entry, not all had recurrent depressive illness, many were psychotic and had greater levels of cognitive impairment, and treatment was naturalistic rather than a standardized protocol. All of our patients were required to have a Mini-Mental State score of 27 or greater, and all were required to have nonpsychotic recurrent unipolar depression. Only two of our 187 patients have developed dementia on follow-up, but more than 40% of the patients of Alexopoulos et al. have developed irreversible dementia. Thus, age at onset may not be as important a determinant of illness course and treatment response in elderly patients with well-established nonpsychotic recurrent major depression as it is in more heterogeneous older populations of elderly patients with depression who have varying levels of preexisting cognitive impairment and delusional thinking. In contrast to age at onset of first lifetime episode of illness, our analyses have found that older age at study entry is associated with longer time to remission (3)—a finding in agreement with that of Alexopoulos et al. (16), Keller et al. (17), and Georgotas and McCue (18).
In addition to subject selection criteria, which may limit the generalizability of the current findings, the reliability with which age at onset can be identified is limited. Wiener et al. (19) recently reported that interrater agreement did not exceed 85% in patients with geriatric depression. Therefore, these authors have recommended (and we concur) that additional clinical, biological, and psychosocial function measures (other than age at onset) be used to characterize the variability of geriatric depression in respect to illness course and treatment response. Our data also suggest, however, that using a highly standardized, intense combination of psychopharmacological and psychosocial treatment may suppress variability in treatment response and long-term course, resulting in better outcomes for geriatric patients with recurrent major depression, comparable to those observed in midlife adults (9). Finally, it is clinically important to note that early-onset patients not only took longer to remit but also had a higher rate of past suicide attempts. Such patients merit particular attention during the acute phase of treatment.
 |
 |
Received July 25, 1997; revision received Oct. 27, 1997; accepted Dec. 11, 1997. From the Mental Health Clinical Research Center for Late-Life Mood Disorders and the Mental Health Clinical Research Center for Affective Disorders, Department of Psychiatry, and the Department of Biostatistics, Graduate School of Public Health, University of Pittsburgh Medical Center. Address reprint requests to Dr. Reynolds, Western Psychiatric Institute and Clinic, Rm. E1135, 3811 O'Hara St., Pittsburgh, PA 15213. Supported in part by NIMH grants MH-52247, MH-30915, MH-43832, and MH-00295. The authors thank Dr. Stanley D. Imber for his collaboration in the design and conduct of this study and the staff of the Late-Life Mood Disorders Clinical Core for their care of the patients participating in this study.
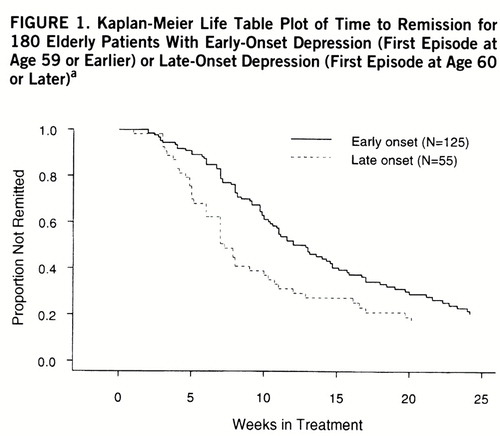
FIGURE 1. Kaplan-Meier Life Table Plot of Time to Remission for 180 Elderly Patients With Early-Onset Depression (First Episode at Age 59 or Earlier) or Late-Onset Depression (First Episode at Age 60 or Later)a
aData for the patients who actually began treatment were analyzed. Time to remission was significantly longer in the early-onset group (Wilcoxon χ2=11.04, df=1, p=0.001). Median time to remission was 12.9 weeks (95% confidence interval=10.6–14.7) for the early-onset group and 7.3 weeks (95% confidence interval=6.0–10.3) for the late-onset group.
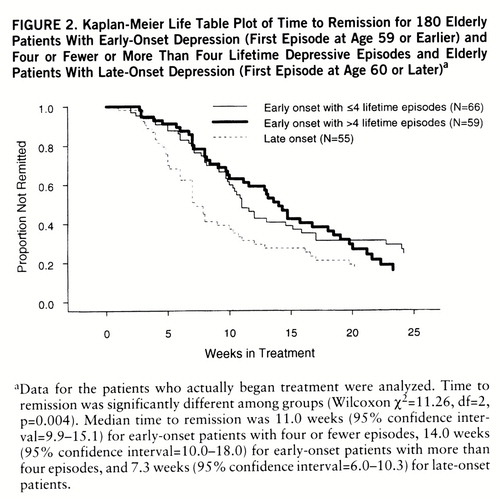
FIGURE 2. Kaplan-Meier Life Table Plot of Time to Remission for 180 Elderly Patients With Early-Onset Depression (First Episode at Age 59 or Earlier) and Four or Fewer or More Than Four Lifetime Depressive Episodes and Elderly Patients With Late-Onset Depression (First Episode at Age 60 or Later)a
aData for the patients who actually began treatment were analyzed. Time to remission was significantly different among groups (Wilcoxon χ2=11.26, df=2, p=0.004). Median time to remission was 11.0 weeks (95% confidence interval=9.9–15.1) for early-onset patients with four or fewer episodes, 14.0 weeks (95% confidence interval=10.0–18.0) for early-onset patients with more than four episodes, and 7.3 weeks (95% confidence interval=6.0–10.3) for late-onset patients.
1 Cole MG: The prognosis of depression in the elderly. Can Med Assoc J 1990; 143:633–639Google Scholar
2 Brodaty H, Harris L, Peters K, Wilhelm K, Hickie I, Boyce P, Mitchell P, Parker G, Eyers K: Prognosis of depression in the elderly: a comparison with younger patients. Br J Psychiatry 1993; 163:589–596Crossref, Medline, Google Scholar
3 Dew MA, Reynolds CF III, Houck PR, Hall MH, Buysse DJ, Frank E, Kupfer DJ: Temporal profiles of the course of depression during treatment: predictors of pathways toward recovery in the elderly. Arch Gen Psychiatry 1997; 54:1016–1024Crossref, Medline, Google Scholar
4 Alexopoulos GS, Meyers BS, Young RC, Mattis S, Kakuma T: The course of geriatric depression with reversible dementia: a controlled study. Am J Psychiatry 1993; 150:1693–1699Link, Google Scholar
5 Murphy E: The prognosis of depression in old age. Br J Psychiatry 1983; 142:111–119Crossref, Medline, Google Scholar
6 Coffey CE, Wilkinson WE, Weiner RD, Parashos IA, Djang WT, Webb MC, Figiel GS, Spritzer CE: Quantitative cerebral anatomy in depression: a controlled magnetic resonance imaging study. Arch Gen Psychiatry 1993; 50:7–16Crossref, Medline, Google Scholar
7 Krishnan KRR, Gadde KM: The pathophysiologic basis for late-life depression—imaging studies of the aging brain. Am J Geriatr Psychiatry 1996; 4(4 suppl):S22–S33Google Scholar
8 Klerman GL, Weissman MM, Rounsaville BJ, Chevron ES: Interpersonal Psychotherapy of Depression. New York, Basic Books, 1984Google Scholar
9 Reynolds CF III, Frank E, Kupfer DJ, Thase ME, Perel JM, Ma~zumdar S, Houck PR: Treatment outcome in recurrent major depression: a post hoc comparison of elderly (“young old”) and midlife patients. Am J Psychiatry 1996; 153:1288–1292Link, Google Scholar
10 Spitzer RL, Endicott J: Schedule for Affective Disorders and Schizophrenia—Lifetime Version. New York, New York State Psychiatric Institute, Biometrics Research, 1978Google Scholar
11 Hamilton M: A rating scale for depression. J Neurol Neurosurg Psychiatry 1960; 23:56–62Crossref, Medline, Google Scholar
12 Folstein MF, Folstein SE, McHugh PR: “Mini-Mental State”: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 1975; 12:189–198Crossref, Medline, Google Scholar
13 Miller MD, Paradis CF, Houck PR, Mazumdar S, Stack JA, Rifai AH, Mulsant B, Reynolds CF III: Rating chronic medical illness burden in geropsychiatric practice and research: application of the Cumulative Illness Rating Scale. Psychiatry Res 1992; 41:237–248Crossref, Medline, Google Scholar
14 Frank E, Prien RF, Jarrett RB, Keller MB: Conceptualization and rationale for consensus definitions of terms in major depressive disorder: remission, recovery, relapse, and recurrence. Arch Gen Psychiatry 1991; 48:851–855Crossref, Medline, Google Scholar
15 Georgotas A, McCue RE, Hapworth W, Friedman E, Kim OH, Welkowitz J, Chang I, Cooper TB: Comparative efficacy and safety of MAOI's vs TCA's in treating depression in the elderly. Biol Psychiatry 1986; 21:1155–1166Crossref, Medline, Google Scholar
16 Alexopoulos GS, Meyers BS, Young RC, Kakuma T, Feder M, Einhorn A, Rosendahl E: Recovery in geriatric depression. Arch Gen Psychiatry 1996; 53:305–312Crossref, Medline, Google Scholar
17 Keller MB, Lavori PW, Collins CE, Klerman GL: Predictors of relapse in major depressive disorder. JAMA 1983; 250:3299–3304Crossref, Medline, Google Scholar
18 Georgotas A, McCue RE: The additional benefit of extending an antidepressant trial past seven weeks in the depressed elderly. Int J Geriatr Psychiatry 1989; 4:191–195Crossref, Google Scholar
19 Wiener P, Alexopoulos GS, Kakuma T, Meyers BS, Rosenthal E, Chester J: The limits of history-taking in geriatric depression. Am J Geriatr Psychiatry 1997; 5:116–125Crossref, Medline, Google Scholar



