Obsessive-Compulsive Disorder and Ventromedial Frontal Lesions: Clinical and Neuropsychological Findings
Abstract
OBJECTIVE: The authors sought to determine the long-term outcome of subjects with severe and refractory obsessive-compulsive disorder (OCD) who had undergone ventromedial frontal leukotomy during the 1970s. Special emphasis was given to the analysis of specific lesion sites. METHOD: Sixteen OCD subjects who had undergone ventromedial frontal leukotomy were evaluated clinically and neuropsychologically and compared to seven well comparison OCD subjects without leukotomy. The 16 leukotomized subjects were divided into three groups according to the main lesion sites as determined by current magnetic resonance imaging scans. RESULTS: The leukotomized OCD subjects showed significant improvement of obsessive-compulsive symptoms; subjects with frontostriatal lesions tended to have improved most. The subjects with combined diagnoses of OCD and obsessive personality disorder (N=3) had improved significantly less. Of 11 subjects with lesions of the ventral striatum, eight had developed substance dependence postoperatively. Intellectual functions were largely preserved in subjects with ventromedial frontal lesions only or frontostriatal lesions. However, all subjects showed subnormal performance on the Wisconsin Card Sorting Test. Subjects with lesions of the dorsolateral frontal convexity also showed memory problems, attentional slowing, and lower performance IQ. CONCLUSIONS: Restricted ventromedial frontal leukotomy should be discussed as a last-resort treatment for severe and refractory OCD but not obsessive personality disorder. Lesions of the ventral striatum were significantly related to the occurrence of substance dependence, suggesting a role of this area in human addictive behavior. (Am J Psychiatry 1998; 155:255–263)
In a minority of cases, obsessive-compulsive disorder (OCD) is refractory to all pharmacological and psychotherapeutic treatments. Extensive, but mostly uncontrolled, evidence suggests that such cases may respond to various types of psychosurgical operations. Developed in the late 1930s and extensively used in the 1940s, early radical forms of frontal leukotomy offered subjects therapeutic gains but at the price of frequent side effects, especially those related to the frontal lobe syndrome (1). More-refined methods, especially the use of stereotaxy, reduced but did not eliminate the risks of personality change and cognitive malfunction after surgery. Unfortunately, evaluation at this time was mainly restricted to assessment of the psychiatric condition treated by surgery, and little attempt was made to study alterations in other aspects of behavior. Only a minority of outcome studies used formal testing (2).
Today a limited number of such operations are still performed; they involve capsulotomy (3), cingulotomy (4, 5), subcaudate tractotomy (6), or combined orbitomedial/cingulate lesions (7). Until the 1980s modified bimedial frontal leukotomy was performed as well (8). Although efficacy and risks vary slightly over the different procedures (2), reports have confirmed their antiobsessional effect in at least 30% of subjects (4–8). Adverse side effects were rare. However, a few subjects were reported to show adverse personality changes of the frontal lobe type (9). Overall cognitive functioning remained surprisingly unaffected (7, 10, 11). Deficits frequently occurred on the Wisconsin Card Sorting Test, a commonly used measure of the ability to form and shift concepts (10, 11).
However, even with the currently used operations, little effort is made to determine the specific lesion sites mediating antiobsessional effects or possible adverse side effects or neuropsychological deficits. During subcaudate tractotomy, radioactive rods are placed beneath and in front of the caudate nucleus (6). Capsulotomy is performed by producing stereotactic lesions within the anterior limb of the internal capsules (3). Cingulotomy involves stereotactic lesions of the anterior cingulate cortex (4). In none of the published studies of these operations were lesion analyses of the respective subjects performed, although the surgical techniques most probably resulted in individually differing lesion sites and lesion sizes.
The aim of the present study was to elucidate the effects of specific lesion sites in OCD subjects with ventromedial frontal leukotomy in order to anatomically specify the antiobsessional effect and to better define the structure-function relationships of cognitive and behavioral frontal lobe functions. A long-term follow-up of subjects who had undergone ventromedial frontal leukotomy for refractory OCD during the 1970s was undertaken. This approach further offered the advantage of determining the long-term effects of the psychosurgical interventions. Usually, follow-ups of such subjects cover at most a few years, thus posing serious difficulties for the evaluation of the stability of therapeutic effects (1).
METHOD
Subjects
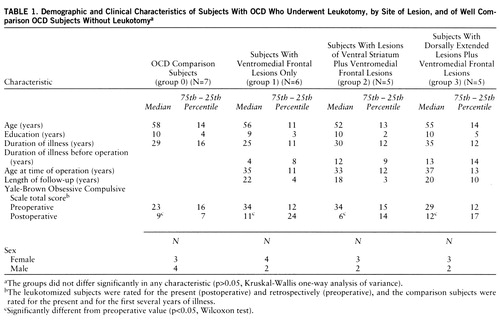
Sixteen subjects who had undergone bilateral ventromedial frontal leukotomy as a last-resort treatment for refractory OCD were evaluated in 1992. The 16 subjects were among 62 whose records had been reviewed. Of this total, current addresses of only 37 could be traced. The remainder had died (N=9), had moved to unknown new locations (N=7), or were excluded because of old age (>85 years, N=3) or presence of an additional psychiatric diagnosis (e.g., schizophrenia, N=6). Of the 37 leukotomized subjects available, 16 agreed to take part in the investigation, which involved 2 days of hospitalization in order to complete tests, interviews, and a magnetic resonance imaging (MRI) scan. Another 13 subjects accepted interviews by telephone and completed questionnaires. Those who objected to these kinds of evaluation (N=8) did so mainly because they did not want to be reminded of the worst time of their lives and feared new exacerbation of symptoms. However, these subjects provided self-ratings of improvement. The leukotomized patients were compared with seven nonleukotomized well comparison subjects (table 1) recruited from hospital inpatients and outpatients who had severe OCD of at least 10 years' duration. After complete description of the study to the subjects, written informed consent was obtained.
Leukotomy
The surgery had been performed by F. Roeder and H. Orthner (departments of neurosurgery and neuropathology at the University of Göttingen). Thermocoagulation lesions were made by stereotaxy with the aid of high-pressure pneumoventriculography. The lesions were always made bilaterally, with 13 to 25 coagulations (mean=18) per hemisphere. The intention was to destroy with each coagulation about 230 mm3 of tissue. Basically, the procedure involved coagulations restricted to the mediobasal angle of the frontal white matter, in order to isolate the ventromedial cortex from its subcortical connections. In some subjects, the leukotomy was extended posteriorly into the white matter of the orbital cortex underlying the caudate nucleus and to the fundus of the striatum. In other subjects, the leukotomy was extended dorsally to the ventromedial lesion in order to isolate the precallosal part of the cingular gyrus. All subjects except two were operated on between 1970 and 1976. Subjects operated on in 1973 and later received lesions extended to the fundus of the striatum, and subjects operated on earlier received ventromedial or dorsally extended lesions. Details of the surgical technique are described in reference 12.
Lesion Groups
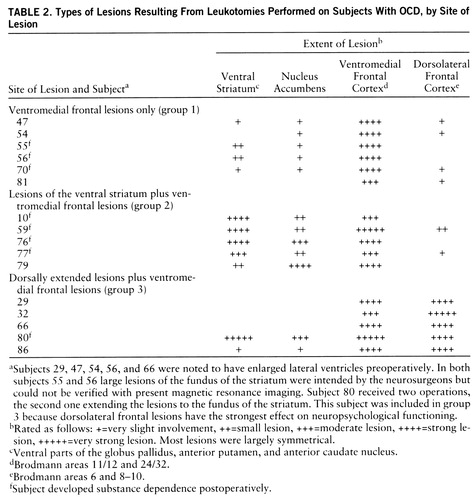
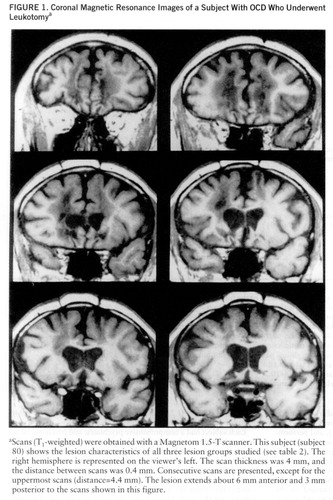
In order to investigate the influence of different lesion sites, the 16 leukotomized subjects were divided into three groups according to the main sites of the lesions as determined by current MRI scans. All subjects had ventromedial frontal lesions (Brodmann areas 11/12 and 24/32). Subjects with lesions mainly restricted to these areas constitute group 1 (N=6). Subjects with a posterior extension of the leukotomy also had lesions of the most posterior parts of areas 11/12 and also lesions of the ventral striatum (ventral parts of the putamen, caudate nucleus, and globus pallidus, and nucleus accumbens) and, to a minor degree, of the substantia innominata. This group is referred to as group 2 (N=5). Subjects with dorsally extended lesions, referred to as group 3 (N=5), showed in addition to the ventromedial frontal lesions marked atrophy and necrosis of the dorsolateral convexity (Brodmann areas 6 and 8–10). The lesion characteristics of all subjects are described in table 2. Figure 1 illustrates the lesions of subject 80. The three lesion groups did not differ significantly in the number of coagulations performed.
Neuropsychological Testing
The following tests were administered to each subject according to standard procedures. By using the German version of the Wechsler Adult Intelligence Scale—Revised (WAIS-R), measures of full-scale IQ, verbal IQ, and performance IQ were derived with a short form that comprised the subtests comprehension, similarities, arithmetic, block design, picture completion, picture arrangement, and digit symbol. Mnemonic functions were assessed with a German translation of the Wechsler Memory Scale—Revised. This battery includes subtests of visual and verbal memory. The memory quotient was obtained on the basis of the standardized scoring systems. Further, a paired-associate learning test (13) was applied. This measure requires subjects to subsequently learn two lists of semantically associated word pairs. Intrusions from the first list elicit proactive interference tendencies. The Wisconsin Card Sorting Test (14) was administered to study impairment of abstract conceptualization and shifting ability. Furthermore, a sorting test for emotional stimuli (pictures from the Ekman series) was applied (paper in preparation by Weniger et al.). For testing attentional performance and psychomotor speed, the Trail Making Test (parts A and B) and a computer-driven test battery (15) comprising various subtests (divided attention, go/no-go, flexibility, working memory) were used.
Clinical Assessment
A German version (16) of the Structured Clinical Interview for DSM-III-R—Patient Version (SCID-P) (17) was administered to assess current and previous psychiatric diagnoses. Obsessive-compulsive symptoms were rated for the present and were retrospectively assessed for the preoperative state by using the German authorized translation (18) of the Yale-Brown Obsessive Compulsive Scale (19). Subjects in groups 1, 2, and 3 completed a German version (short form) of the MMPI (20).
Each subject had a comprehensive psychiatric and psychosocial assessment by means of two independent interviews (performed by E.I. and E.R.). A detailed history of the pre- and postoperative course of illness and the current level of psychosocial functioning were recorded. The subjects rated severity and improvement of obsessive-compulsive symptoms on visual analogue scales. Further, obsessive-compulsive symptoms and other complaints were self-rated by the subjects for the entire lifespan, and the subjects were asked to comment on possible causes for major changes. The information obtained was validated by the detailed case notes and by information obtained from current psychotherapists. For each psychiatric diagnosis there was complete correspondence between the two interviews, the SCID-P, and the case notes and information obtained from current psychotherapists.
Statistical Analyses
Statistical computations were based on scaled scores (WAIS-R, revised Wechsler Memory Scale) or raw scores. Because of the small number of subjects in each group, only nonparametric statistical methods were used (Kruskal-Wallis one-way analysis of variance, Wilcoxon test, Mann-Whitney U test, Spearman rank correlation). Frequencies were compared by using the binomial test because of the small number of subjects. All analyses were two-tailed, and the alpha was defined as 0.05. Bonferroni corrections were applied for neuropsychological measurements (e.g., measures of the Wisconsin Card Sorting Test). All statistical comparisons were performed by using SPSS for Windows, version 6.0.1.
RESULTS
Neuropsychological Testing
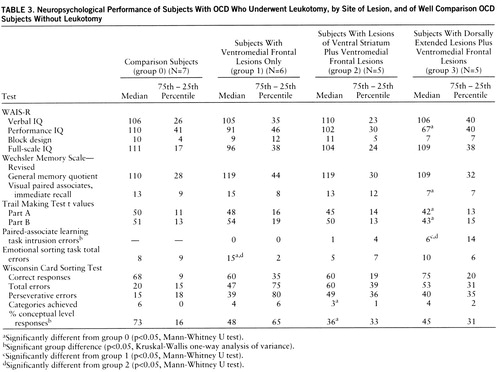
The neuropsychological test results of all groups are summarized in table 3. No significant group differences were found for verbal or full-scale IQ (WAIS-R) among any of the groups, including the comparison group. However, group 3 (with dorsally extended lesions plus ventromedial frontal lesions) had a significantly lower performance IQ than the comparison group (U=5.0, p<0.05). Three of the five subjects in group 3 performed poorly on performance-related tasks, achieving performance IQ scores of more than two standard deviations below average.
There was no significant group difference for the overall memory quotient yielded by the revised Wechsler Memory Scale, although group 3 scored significantly below the comparison subjects on one subtest of nonverbal memory—visual paired associates, immediate recall (U=5.5, p<0.05). Significant group differences were seen for the number of intrusion errors in the paired-associate learning task (χ2=7.8, df=2, p<0.05). Post hoc analyses revealed that group 3 made significantly more intrusion errors than group 1 (U=1.5, p<0.04) and group 2 (U=0.0, p<0.03). All of the subjects in group 3, one subject in group 2, and none of the subjects in group 1 had scores on this test below the 16th percentile of a normal comparison population.
All three lesion groups showed marked difficulties with the Wisconsin Card Sorting Test. Significant group differences were seen for the percentage of conceptual level responses (χ2=8.2, df=3, p<0.05). The subjects in group 2 (lesions of the ventral striatum plus ventromedial frontal lesions) were the most impaired, producing significantly fewer categories (U=3.0, p<0.02) and more perseverative and total errors than the comparison subjects. However, on a sorting test for emotional stimuli (pictures from the Ekman series), the performance of the group 2 subjects was similar to that of the comparison subjects (group 0), but group 1 (with ventromedial frontal lesions only) performed significantly worse than group 0 (U=3.0, p<0.02) and group 2 (U=2.0, p<0.02).
All groups, including the comparison group, showed reaction times below the 16th percentile of a normal control population on the computerized tests of attentional performance, except for the go/no-go subtest. The subtest for divided attention yielded the worst results; i.e., 16 of the 22 study subjects (including six out of the seven comparison subjects) showed reaction times below the 16th percentile. The performance on the Trail Making Test was for most subjects within the normal range for a comparison population. However, the group 3 subjects were significantly slower than the comparison subjects (part A: U=5.5, p<0.05; part B: U=5.0, p<0.05). Group 3 also had longer reaction times than group 2 on two of the computerized tests of attentional performance, divided attention (U=2.0, p<0.04) and go/no-go (U=1.5, p<0.02). Reaction time on the go/no-go task was also significantly longer for group 1 than for group 2 (U=1.5, p<0.02).
Clinical Assessment
On the basis of detailed reviews of case notes, the SCID-P, and two independent psychiatric interviews, it could be established that at the time of their operations all of the leukotomized subjects had met the DSM-III-R criteria for severe and chronic OCD and that the OCD had been refractory to extensive trials with nonsurgical psychiatric treatments (e.g., antidepressant medication, various kinds of psychotherapy, electroconvulsive shock, sleep therapy). The clinical records of eight subjects contained reports of at least one suicide attempt. Three subjects (numbers 47 and 81 in group 1 and number 80 in group 3) additionally met the DSM-III-R criteria for obsessive personality disorder. All of the subjects in the comparison group met the criteria for OCD, and none had an additional diagnosis of obsessive personality disorder.
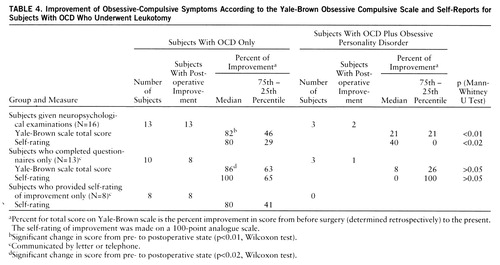
According to Wilcoxon tests, the three lesion groups had significant improvements in their scores on the Yale-Brown Obsessive Compulsive Scale between the (retrospectively rated) presurgical state and the current postsurgical state (group 1: z=–2.2, p<0.03; group 2: z=–2.0, p<0.05; group 3: z=–2.0, p<0.05) (see table 1). The subjects in the comparison group significantly improved as well (z=–2.02, p<0.05). Groups 1 and 2 had strong, similar median levels of improvement on the Yale-Brown Obsessive Compulsive Scale (73% and 75%, respectively), but group 3 improved less (56%). However, these differences did not reach conventional levels of significance. The scores of the subjects with both OCD and obsessive personality disorder (N=3) differed from those of the subjects with OCD only (N=13), and the subjects with both OCD and obsessive personality disorder showed significantly less improvement (U=1.0, p<0.01) (table 4). Two of the OCD subjects with obsessive personality disorder (subjects 47 and 80) and two subjects with OCD (subjects 66 and 77) were receiving clomipramine at the time of the study. The present scores on the Yale-Brown Obsessive Compulsive Scale of the two OCD subjects (16 and 10, respectively) were well within the range of the scores for the other OCD subjects, lending further support to the idea that the clinical outcomes of the leukotomized subjects were mainly related to the surgery.
Outcome categories were formed on the basis of pre- and postoperative scores on the Yale-Brown Obsessive Compulsive Scale, as described by Jenike et al. (5). Marked improvement (>75%) was shown by 44% of the subjects (N=7), and another 25% (N=4) showed moderate improvement (>50%). Only one subject (6%) experienced less than 25% improvement in obsessive-compulsive symptoms. Eleven (85%) of the 13 subjects with OCD but not obsessive personality disorder were convinced that the surgery was the cause for all or most of their improvement, which appeared in eight subjects 3–12 months after surgery and in three subjects 1–2 years postoperatively. Two of the subjects with both OCD and obsessive personality disorder experienced less intense improvement 3–8 months postoperatively, and one subject with OCD and obsessive personality disorder experienced no operation effect.
Table 4 contains the rates of improvement for the 16 leukotomized study subjects and for the contacted subjects who did not receive neuropsychological examinations. The OCD subjects completing only questionnaires showed strong improvements (86%) (Wilcoxon test: z=–2.4, p<0.02) on the Yale-Brown Obsessive Compulsive Scale similar to those of the study subjects (82%) (z=–3.2, p<0.01). The self-ratings of outcome on the visual analogue scale were similar for the study subjects, the subjects completing only questionnaires, and the subjects not available for these kinds of evaluation (table 4). The improvement reported by self-rating was significantly related to the improvement in Yale-Brown Obsessive Compulsive Scale scores for the study subjects (rs=0.68, N=16, p<0.005) and for the subjects completing only questionnaires (rs=0.68, N=13, p<0.01).
Changes on measures of psychosocial functioning can be seen from table 5. The postoperative scores of the OCD subjects on the Global Assessment of Functioning Scale (axis V of DSM-III-R) were significantly better than the preoperative scores (determined retrospectively). Further, there was a significant increase after surgery in the number of OCD subjects who were able to work. Also, significantly fewer OCD subjects suffered from dysthymic disorder after leukotomy. Sexual problems were reduced postoperatively in five of the seven subjects complaining of them preoperatively. However, for three subjects (numbers 32, 56, and 59) a loss of drive and initiative clearly occurred after surgery. These subjects, as well as those with combined OCD and obsessive personality disorder, also had higher depression scores (t value >70) on the MMPI after surgery.
There was a significant increase in the number of subjects who became addicted to alcohol (N=6) or to alcohol and benzodiazepines (N=2) after psychosurgery, and there was no case of substance dependence before surgery (table 5). The addicted subjects started to drink between 3 and 9 years postoperatively and in most cases during severe psychosocial stress (e.g., divorce, accident). Five of these subjects experienced remissions of their substance dependence during long-term inpatient psychotherapy. The remaining three subjects (numbers 10, 56, and 59) had extraordinarily severe courses of chronic alcohol disorder, being refractory to numerous and protracted inpatient psychotherapies. Subjects 56 and 77 had family histories of alcoholism and had occasionally showed signs of substance abuse before psychosurgery.
Lesion analysis revealed that all of the addicted subjects had lesions in the ventral striatum. Of the 11 subjects with lesions of the ventral striatum (table 2), eight developed substance dependence postoperatively (p<0.01, binomial test). There was no case of postoperative addiction in the subjects without striatal lesions. Accordingly, the extent of ventral striatal lesions (as indicated in table 2) was significantly different for the addicted and nonaddicted subjects (U=3.0, p<0.002).
DISCUSSION
Before the results are discussed it seems appropriate to mention the limitations of this study. First, the number of subjects was relatively small, especially as three different types of lesions were studied. Second, the preoperative data were limited to case records; no formal prospective assessment was made. Thus, all measures of improvement were based on the retrospective judgment of the patients and may therefore be confounded. Third, as psychosurgery was a treatment of last resort, obtaining a comparison group retrospectively that matched the leukotomized subjects in terms of severity and chronicity of illness was extremely difficult. As a consequence, our comparison group mostly contained subjects who were not recommended for leukotomy because of less severe OCD or better responsiveness to other kinds of therapy.
In view of these limitations, our conclusions are tentative. However, the subjects were thoroughly assessed by means of an extensive battery of neuropsychological tests. All subjects were personally interviewed, and the interviewers had not been involved in the treatment of the subjects. The comparison subjects did match the leukotomized subjects well in terms of age, sex, education, duration of illness, and current (although not preoperative) severity of symptoms.
Neuropsychological Findings
A comprehensive neuropsychological test battery was administered to the leukotomized subjects and comparison subjects. We found largely preserved intellectual functions (see table 3), a finding that is consistent with previous results for subjects who had been treated with subcaudate tractotomy (10) or cingulotomy (7). However, group 3 (with dorsolateral frontal lesions) had a significantly lower performance IQ (median=67) than the OCD comparison subjects (median=110) (see table 3). This finding is consistent with the literature, which indicates that loss on WAIS-R scales is more often associated with lesions of the dorsolateral convexity (21). It must, however, be noted that poor performance on visual-spatial tasks, which mainly contribute to the Wechsler performance scale, has been found relatively consistently in OCD subjects who have not received psychosurgery (see, for instance, references 22 and 23), a finding that we could not confirm in our study.
With regard to the data for memory tasks, we could not find a general memory impairment in the leukotomized subjects. However, the dorsolateral group (group 3) performed significantly poorer than the nonleukotomized comparison subjects on a visual and a verbal paired-associate learning task. Our finding of significantly more intrusion errors, thus greater susceptibility to proactive interference, in group 3 is in line with previous reports on effects of frontal lesions on memory and learning. Resistance to interference is often reported to be the aspect of mnestic activity that is most likely to be disturbed after dorsolateral prefrontal pathology (21, 24).
Poor performance on the Wisconsin Card Sorting Test is consistently reported in OCD subjects not receiving surgery (22), as well as in those who do receive surgery (7, 10, 11). We could not confirm the deficit in our nonleukotomized comparison subjects but did find such a deficit in varying degrees for the three lesion groups, with group 2 (lesions of the ventral striatum plus ventromedial frontal lesions) showing the poorest performance. This finding was somewhat unexpected since Wisconsin Card Sorting Test performance has been associated with dorsolateral prefrontal activation of regional cerebral blood flood (25, 26). Additionally, the group 2 subjects showed the best results in a task requiring the sorting and categorization of emotional stimuli (see table 3). Probably the planning and sequencing behavior required for the Wisconsin Card Sorting Test was especially impaired in our group 2 subjects because of their striatal lesions. Lesions of the caudate nucleus have been reported to impair these kinds of behavior, including performance of the Wisconsin Card Sorting Test (27).
Clinical Outcome
In the majority of our subjects obsessive-compulsive symptoms were greatly improved after surgery and so was social adjustment (see tables 4 and 5). Improvement of more than 50% on the Yale-Brown Obsessive Compulsive Scale was found for 69% of the subjects. This improvement rate roughly matches rates found in other studies. In a prospective study of 26 OCD subjects who underwent psychosurgery involving orbitomedial and/or cingulate lesions, Hay et al. (7) demonstrated obvious improvement in 38% of the subjects and mild improvement in an additional 23% according to a 6-point global rating scale based on the Goktepe scale (28).
Jenike et al. (5) retrospectively studied 35 OCD subjects two decades after cingulotomy and established that at least 30% benefited substantially from the procedure, i.e., showed more than 50% improvement on the Yale-Brown Obsessive Compulsive Scale. In a review of all patients who had received stereotactic subcaudate tractotomy in Great Britain, Bridges et al. (6) found 33%–45% of OCD subjects to be in outcome category I or II of Goktepe's 5-point rating scale.
Our study has demonstrated the long-term antiobsessional effect of bifrontal leukotomy in severe OCD. Most subjects show clearly reduced obsessive-compulsive symptoms and improved psychosocial function. Both were sustained for more than two decades. Restricted ventromedial frontal leukotomy should therefore be discussed as a last-resort treatment for severe and refractory OCD but not obsessive personality disorder. However, it seems difficult to judge whether the long-term outcome of leukotomized OCD subjects is significantly better than the natural course of the illness (1). Since psychosurgery was always a treatment of last resort, obtaining a comparison group without psychosurgery that matched our leukotomized subjects in terms of severity and chronicity of illness was extremely difficult. However, most of our leukotomized subjects were convinced that they would have tried to commit suicide if their severe illness had persisted (eight subjects had attempted suicide before their operations).
Comparing the efficacy of the different psychosurgical procedures has proved difficult. However, the existing data suggest that the different procedures (i.e., tractotomy, capsulotomy, cingulotomy) have roughly comparable degrees of efficacy. Also, we could not find significantly different effects of the different surgical approaches, despite detailed analyses of the lesions of each subject. Nevertheless, group 2 (lesions of the ventral striatum plus ventromedial frontal lesions) tended to show the most improvement (scores on the Yale-Brown Obsessive Compulsive Scale are given in table 1).
Evidence is converging that the projection of allocortical frontal regions onto the ventral striatum (reference 29 provides an overview) is a critical route for obsessive-compulsive behavior: the serotonergic innervation of the most anterior ventral striatum is profound (30), and serotonin reuptake inhibitors have been shown to be effective for many OCD subjects (31). Successful behavior therapy or pharmacotherapy with fluoxetine was shown to reduce the metabolic activity of the caudate nucleus and orbitofrontal cortex of OCD subjects (32). On the other hand, provocation of obsessive-compulsive symptoms may increase the orbitofrontal cortex activity of OCD subjects (33). Thus, the common feature of our three lesion groups may be that all lesions effectively interrupted the frontal/basal ganglia/thalamic/frontal loop in our subjects at some stage. However, quantitative morphometric studies point to widely distributed structural brain abnormalities in the OCD subjects as well, e.g., low white matter volume, high ventricle-to-brain ratio (34).
Surprisingly, the ventromedial frontal lesions of our subjects were followed by many fewer deficits in the domain of emotion and personality than would be assumed from human neuropsychological lesion studies (e.g., references 21, 35). Our psychiatric assessment indicated that many subjects had difficulties in relating their emotional state to self-cognition, but none of these subjects seemed to be obviously impaired in his or her personal life. An explanation for this could be that the ventromedial frontal cortex of our OCD subjects was hyperfunctional in the preoperative state and that lesioning part of this cortex returned the activity of its functional loops toward normal levels. Similar proposals have been made by the neurosurgeons performing the lesions in our subjects.
Substance Dependence
A serious finding was the occurrence of addiction in eight subjects (50%) after surgery; the addictions of three subjects were untreatable. Although there is a generally higher than normal risk for OCD subjects to become addicted in the long course of a debilitating illness, the reported prevalence rates are not higher than 12%–15% (36, 37). Our figures are clearly higher than this. Other reports do not mention any case of postoperative-onset addiction among OCD subjects (3, 5, 7–9), even after subcaudate tractotomy.
All of the addicted subjects in our study had lesions of the ventral striatum (see table 2 and Results section, “Clinical Assessment”). Research suggests that the ventral striatum (including the nucleus accumbens) is the main link between the limbic system and motor output (29). Information derived from limbic system circuits may reach the caudate nucleus and putamen by several routes, including inputs from the amygdala/hippocampus complex and from the reward-related dopamine-containing neurons in the substantia nigra pars compacta and the ventral tegmental area (29, 38). The ventral striatal lesions in our subjects most probably led to a disturbance or interruption of information flow between the limbic and motor systems.
There is now an extensive literature from animal research that points to the involvement of the ventral striatum in the regulation of motivation and reward and its role in addiction (reference 39 provides an overview). For example, creation of lesions in the region of the nucleus accumbens in rats leads to a decrease in the self-administration of cocaine (40), which possibly reflects an anhedonia due to disturbance of the mesocorticolimbic dopamine system. It might be speculated that our subjects with ventral striatal lesions developed anhedonia, facilitating drug abuse and dependence in the presence of psychosocial stress. However, little is known about the role of the ventral striatum and nucleus accumbens in humans because specific lesions of this area are extremely rare. Our findings could indicate a role of this area in human addictive behavior, although the exact mechanisms remain to be elicited.
 |
 |
 |
 |
 |
Received May 13, 1996; revision received June 16, 1997; accepted July 17, 1997. From the Department of Psychiatry, University of G<148>ttingen. Address reprint requests to Dr. Irle, Department of Psychiatry, University of G<148>ttingen, Von-Siebold-Strasse 5, D-37075 G<148>ttingen, Federal Republic of Germany; [email protected] (e-mail). The authors thank the participating subjects, Hans Orthner for case notes and surgical data, Hans-Ulrich Wittchen for advice concerning clinical assessment of subjects, and Tatjana Dietrich for performance of neuropsychological testing.
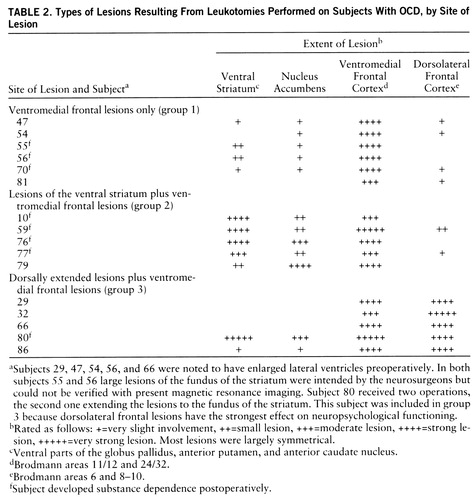 |
FIGURE 1. Coronal Magnetic Resonance Images of a Subject With OCD Who Underwent Leukotomya
aScans (T1-weighted) were obtained with a Magnetom 1.5-T scanner. This subject (subject 80) shows the lesion characteristics of all three lesion groups studied (see table 2. ). The right hemisphere is represented on the viewer's left. The scan thickness was 4 mm, and the distance between scans was 0.4 mm. Consecutive scans are presented, except for the uppermost scans (distance=4.4 mm). The lesion extends about 6 mm anterior and 3 mm posterior to the scans shown in this figure.
1. Swayze VW II: Frontal leucotomy and related psychosurgical procedures in the era before antipsychotics (1935–1954): a historical overview. Am J Psychiatry 1995; 152:505–515Link, Google Scholar
2. Diering SL, Bell WO: Functional neurosurgery for psychiatric disorders: a historical perspective. Stereotact Funct Neurosurg 1991; 57:175–194Crossref, Medline, Google Scholar
3. Mindus P, Nyman H: Normalization of personality characteristics in patients with incapacitating anxiety disorders after capsulotomy. Acta Psychiatr Scand 1991; 83:283–291Crossref, Medline, Google Scholar
4. Baer L, Rauch SL, Ballantine HT Jr, Martuza R, Cosgrove R, Cassem E, Giriunas I, Manzo PA, Dimino C, Jenike MA: Cingulotomy for intractable obsessive-compulsive disorder: prospective long-term follow-up of 18 patients. Arch Gen Psychiatry 1995; 52:384–392Crossref, Medline, Google Scholar
5. Jenike MA, Baer L, Ballantine T, Martuza RL, Tynes S, Giriunas I, Buttolph ML, Cassem NH: Cingulotomy for refractory obsessive-compulsive disorder: a long-term follow-up of 33 patients. Arch Gen Psychiatry 1991; 48:548–555Crossref, Medline, Google Scholar
6. Bridges PK, Bartlett JR, Hale AS, Poynton AM, Malizia AL, Hodgkiss AD: Psychosurgery: stereotactic subcaudate tractotomy: an indispensable treatment. Br J Psychiatry 1994; 165:599–611Crossref, Medline, Google Scholar
7. Hay P, Sachdev P, Cumming S, Smith JS, Lee T, Kitchener P, Matheson J: Treatment of obsessive-compulsive disorder by psychosurgery. Acta Psychiatr Scand 1993; 87:197–207Crossref, Medline, Google Scholar
8. Hussain ES, Freeman H, Jones RAC: A cohort study of psychosurgery cases from a defined population. J Neurol Neurosurg Psychiatry 1988; 51:345–352Crossref, Medline, Google Scholar
9. Sachdev P, Hay P: Does neurosurgery for obsessive-compulsive disorder produce personality change? J Nerv Ment Dis 1995; 183:408–413Google Scholar
10. Kartsounis LD, Poynton A, Bridges PK, Bartlett JR: Neuropsychological correlates of stereotactic subcaudate tractotomy: a prospective study. Brain 1991; 114:2657–2673Google Scholar
11. Nyman H, Mindus P: Neuropsychological correlates of intractable anxiety before and after capsulotomy. Acta Psychiatr Scand 1995; 91:23–31Crossref, Medline, Google Scholar
12. Orthner H, Müller D, Roeder F: Stereotactic psychosurgery: techniques and results since 1955, in Psychosurgery. Edited by Hitchcock E, Laitinen L, Vaernet K. Springfield, Ill, Charles C Thomas, 1972, pp 377–390Google Scholar
13. Winocur G, Weiskranitz L: An investigation of paired-associate learning in amnesic patients. Neuropsychologia 1976; 14:97–110Crossref, Medline, Google Scholar
14. Heaton RK, Chelune GJ, Talley JL, Kay GG, Curtiss G: Wisconsin Card Sorting Test Manual. Odessa, Fla, Psychological Assessment Resources, 1993Google Scholar
15. Zimmermann P, Fimm B: Testbatterie zur Aufmerksamkeitsprüfung, version 1.02. Freiburg, Germany, Psytest, 1993Google Scholar
16. Wittchen HU, Zaudig M, Schramm E, Spengler P, Mombour W, Klug J, Horn R: Strukturiertes Klinisches Interview für DSM-III-R. Weinheim, Germany, Beltz, 1991Google Scholar
17. Spitzer RL, Williams JBW, Gibbon M, First MB: Structured Clinical Interview for DSM-III-R—Patient Version 1.0 (SCID-P). Washington, DC, American Psychiatric Press, 1990Google Scholar
18. Hand I, Büttner-Westphal H: Die Yale-Brown Obsessive Compulsive Scale (Y-BOCS): ein halbstrukturiertes Interview zur Beurteilung des Schweregrades von Denk-und HandlungszwÄngen. Verhaltenstherapie 1991; 1:223–225Crossref, Google Scholar
19. Goodman WK, Price LH, Rasmussen SA, Mazure C, Fleischmann RL, Hill CL, Heninger GR, Charney DS: The Yale-Brown Obsessive Compulsive Scale, I: development, use, and reliability. Arch Gen Psychiatry 1989; 46:1006–1011Google Scholar
20. Gehring A, Blaser A: MMPI—Minnesota Multiphasic Personality Inventory: Deutsche Kurzfassung für Handauswertung. Bern, Switzerland, CH Huber, 1989Google Scholar
21. Stuss DT, Benson DF: The Frontal Lobes. New York, Raven Press, 1986Google Scholar
22. Head D, Bolton D, Hymas N: Deficits in cognitive shifting ability in patients with obsessive-compulsive disorder. Biol Psychiatry 1989; 25:929–937Crossref, Medline, Google Scholar
23. Insel TR, Donnelly EF, Lalakea ML, Alterman IS, Murphy DL: Neurological and neuropsychological studies of patients with obsessive-compulsive disorder. Biol Psychiatry 1983; 18:741–751Medline, Google Scholar
24. Irle E, Wowra B, Kunert HJ, Hampl J, Kunze S: Memory disturbances following anterior communicating artery rupture. Ann Neurol 1992; 31:473–480Crossref, Medline, Google Scholar
25. Weinberger DR, Berman KF, Zec RF: Physiologic dysfunction of dorsolateral prefrontal cortex in schizophrenia, I: regional cerebral blood flow evidence. Arch Gen Psychiatry 1986; 43:114–124Crossref, Medline, Google Scholar
26. Rezai K, Andreasen NC, Alliger R, Cohen G, Swayze V II, O'Leary DS: The neuropsychology of the prefrontal cortex. Arch Neurol 1993; 50:636–642Crossref, Medline, Google Scholar
27. Mendez MF, Adams NL, Skoog Lewandowski K: Neurobehavioral changes associated with caudate lesions. Arch Neurol 1989; 39:349–354Google Scholar
28. Bridges PK, Goktepe EO, Maratos J: A comparative review of patients with obsessional neurosis and with depression treated by psychosurgery. Br J Psychiatry 1973; 123:663–674Crossref, Medline, Google Scholar
29. Parent A, Hazrati L-N: Functional anatomy of the basal ganglia, I: the cortico-basal ganglia-thalamo-cortical loop. Brain Res Brain Res Rev 1995; 20:91–127Crossref, Medline, Google Scholar
30. Insel TR: Toward a neuroanatomy of obsessive-compulsive disorder. Arch Gen Psychiatry 1992; 49:739–744Crossref, Medline, Google Scholar
31. Goodman WK, Price LH, Rasmussen SA, Delgado PL, Heninger GR, Charney DS: Efficacy of fluvoxamine in obsessive-compulsive disorder. Arch Gen Psychiatry 1989; 46:36–44Crossref, Medline, Google Scholar
32. Baxter LR, Schwartz JM, Bergman KS, Szuba MP, Guze BH, Mazziotta JC, Alazraki A, Selin CE, Ferng H-K, Munford P, Phelps ME: Caudate glucose metabolic rate changes with both drug and behavior therapy for obsessive-compulsive disorder. Arch Gen Psychiatry 1992; 49:681–689Crossref, Medline, Google Scholar
33. Breiter HC, Rauch SL, Kwong KK, Baker JR, Weisskoff RM, Kennedy DN, Kendrick AD, Davis TL, Jiang A, Cohen MS, Stern CE, Belliveau JW, Baer L, O'Sullivan RL, Savage CR, Jenike MA, Rosen BR: Functional magnetic resonance imaging of symptom provocation in obsessive-compulsive disorder. Arch Gen Psychiatry 1996; 53:595–606Crossref, Medline, Google Scholar
34. Jenike MA, Breiter HC, Baer L, Kennedy DN, Savage CR, Olivares MJ, O'Sullivan RL, Shera DM, Rauch SL, Keuthen N, Rosen BR, Caviness VS, Filipek PA: Cerebral structural abnormalities in obsessive-compulsive disorder. Arch Gen Psychiatry 1996; 53:625–632Crossref, Medline, Google Scholar
35. Irle E, Peper M, Wowra B, Kunze S: Mood changes after surgery for tumors of the cerebral cortex. Arch Neurol 1994; 51:164–174Crossref, Medline, Google Scholar
36. Eisen JL, Rasmussen SA: Coexisting obsessive-compulsive disorder and alcoholism. J Clin Psychiatry 1989; 50:96–98Medline, Google Scholar
37. Fals-Stewart W, Angarano K: Obsessive-compulsive disorder among patients entering substance abuse treatment. J Nerv Ment Dis 1994; 182:715–719Crossref, Medline, Google Scholar
38. Kimura M, Graybiel AM: Role of basal ganglia in sensory motor association learning, in Functions of the Cortico-Basal Ganglia Loop. Edited by Kimura M, Graybiel AM. Tokyo, Springer, 1995, pp 2–17Google Scholar
39. Robbins TW, Cador M, Taylor JR, Everitt BJ: Limbic-striatal interactions in reward-related processes. Neurosci Biobehav Rev 1989; 13:155–162Crossref, Medline, Google Scholar
40. Koob GF, Vaccarino FJ, Amalric M, Bloom FE: Positive reinforcement properties of drugs: search for neural substrates, in Brain Reward Systems and Abuse. Edited by Engel J, Oreland L. New York, Raven Press, 1987, pp 35–50Google Scholar



