Thirty-Month Outcome in Patients With Anorexia or Bulimia Nervosa and Concomitant Obsessive-Compulsive Disorder
Abstract
OBJECTIVE: The present study examines whether concomitant obsessive-compulsive disorder (OCD) indicates a poorer prognosis for patients with anorexia or bulimia nervosa. METHOD: Seventy-five female inpatients who met DSM-IV criteria for anorexia or bulimia nervosa took part in the follow-up study; 29 of these patients met criteria for concomitant OCD. All patients were investigated twice: during inpatient treatment and at follow-up 30 months after discharge. A semistructured diagnostic interview was used as well as the Eating Disorder Inventory and the Hamburg Obsession-Compulsion Inventory—Short Form. RESULTS: At follow-up, 51% (N=38) of the patients no longer fulfilled DSM-IV criteria for anorexia or bulimia nervosa, but this improvement was not significantly correlated with the earlier presence of concomitant OCD. Analysis of variance for repeated measures revealed significant improvement over time on six of the eight Eating Disorder Inventory subscales for all patients regardless of OCD presence. Furthermore, no significant group effects or group-by-time interactions were identified. Clinically significant change, as reflected by improvement in scores on the Eating Disorder Inventory, was seen somewhat more often in patients without concomitant OCD, but this trend was not statistically significant. The patients whose eating disorders were most improved at follow-up also showed the highest reduction of obsessions and compulsions. CONCLUSIONS: The results suggest that concomitant OCD does not indicate a significantly poorer prognosis for patients with anorexia or bulimia nervosa. (Am J Psychiatry 1998; 155:244–249)
Over the years, the issue of the comorbidity of eating disorders and obsessive-compulsive disorder (OCD) has been discussed often. Many authors have agreed that the lifetime prevalence of eating disorders among patients with OCD is 11%–13% (1–4). In addition, other studies have described a high lifetime prevalence of OCD (15%–33%) among patients with anorexia or bulimia nervosa (5–7) and a current prevalence of 3%–37% (5, 7–10). The reason for the comorbidity of the two disorders is unclear. Comparative studies have revealed marked similarities as well as differences in personality and psychopathological features between patients with eating disorders and those with OCD (11–18). Thus, it has been hypothesized that anorexia and bulimia nervosa belong to the family of obsessive-compulsive spectrum disorders (19, 20).
In the 1960s, it was assumed that anankastic personality traits and obsessive-compulsive symptoms in anorectic patients indicated a poorer prognosis (21). More recently, some authors have suggested that patients with comorbidity might respond differently to various types of treatment (7, 22). To date, it is still unclear which factors are crucial for the long-term outcome of eating disorders (23–25). Therefore, controlled studies on this issue have been recommended in order to isolate variables that may be critical for prognosis (24, 26).
Our objective in the present study was to investigate the question of whether concomitant OCD influences the treatment outcome of patients with anorexia or bulimia nervosa.
METHOD
Subjects
We examined female inpatients at the Eating Disorder Clinic Am Korso (Bad Oeynhausen, Germany) who were participating in a psychodynamic therapy program without psychopharmacotherapy (27). Written informed consent was obtained from all patients after the procedures had been fully explained. The local ethics committee had previously given its approval. Diagnoses were made according to DSM-IV criteria. At the beginning of inpatient treatment, 93 patients were included in the study. Thirty-three of these patients (35%) met the criteria for anorexia nervosa, and 60 patients (65%) met criteria for bulimia nervosa. Thirty-four patients (37%) also met criteria for OCD and had a clinically significant score of 16 or higher on the Yale-Brown Obsessive Compulsive Scale (28–31). A detailed description of the initial results of this study regarding the prevalence of concomitant OCD in anorexia and bulimia nervosa has already been published (9).
In this article, we present the follow-up results of the second assessment, which was performed 30 months after discharge. At follow-up we were able to assess 75 of the 93 patients. Therefore, the dropout rate was 19%. The mean age of the follow-up group was 27.4 years (SD=5.3, range=20–44). Twenty-nine of the 75 women (39%) had met the criteria for concomitant OCD before inpatient treatment.
Instruments
Three tests were used for assessment at follow-up. 1) A personal semistructured interview was used that assesses the diagnostic criteria for eating disorders, general psychopathology, weight, and eating behavior, as well as family and occupational situation. 2) The Eating Disorder Inventory (32, 33) is a self-rating questionnaire for specific cognitive and behavioral dimensions of the psychopathology typical of patients with eating disorders. This inventory consists of the following eight subscales: drive for thinness, bulimia, body dissatisfaction, ineffectiveness, perfectionism, interpersonal distrust, interoceptive awareness, and maturity fears. The test-retest reliability for the total Eating Disorder Inventory score is excellent (r=0.96) and ranges from good to excellent (r=0.65–0.97) for the eight subscales (34). The 64 Eating Disorder Inventory items are rated on a 6-point scale. 3) The Hamburg Obsession-Compulsion Inventory—Short Form (35, 36) is used for the assessment of obsessive and compulsive behavior not related to food or dieting behavior. The Hamburg Obsession-Compulsion Inventory—Short Form is a 72-item self-rating questionnaire that consists of six subscales for different kinds of obsessions and compulsions. The test-retest reliability for the six subscales ranges from good to excellent (r=0.73–0.94) (36).
Statistical Analysis
Univariate comparisons were made by using the chi-square test with Yates's continuity correction for 2×2 tables or Fisher's exact test for differences in proportions, and the Mann-Whitney U test or Wilcoxon matched-pairs test for median differences in nonparametric data. The Eating Disorder Inventory scale scores were calculated on the basis of a 6-point rating scale. The evaluation of mean differences in total Eating Disorder Inventory score (sum of the eight Eating Disorder Inventory subscales) was performed by using Student's t test for independent samples. All tests were two-tailed. Significance was set at p<0.05. The difference score for the Hamburg Obsession-Compulsion Inventory—Short Form was calculated by subtracting the total score (sum of the six subscales) at follow-up from the pretreatment score.
To compare the outcome of patients with and without concomitant OCD, the Eating Disorder Inventory data were analyzed in two different ways. First, the scores of each Eating Disorder Inventory scale were evaluated by using a three-way repeated measures analysis of variance (ANOVA) with eating disorder (i.e., anorexia nervosa or bulimia nervosa), group (i.e., with or without concomitant OCD), and time as factors. Second, pretreatment and follow-up data from the Eating Disorder Inventory were analyzed for evidence of clinically significant change on each of the eight subscales. Clinically significant change was based on the Jacobson and Truax formula (37), which has two criteria: 1) the Eating Disorder Inventory score must decrease and traverse the probabilistic boundary between functional and dysfunctional norms, and 2) the change must be at least 1.96 times larger than the standard error of measurement of the difference scores for the Eating Disorder Inventory. When the latter is fulfilled, the probability that a score would change this much by chance is less than 5% (p<0.05). This formula has already been used successfully to assess clinically significant change in Eating Disorder Inventory scores after pharmacotherapy in patients with bulimia nervosa (38). The chi-square test of independence was used to examine the association between clinically significant change and concomitant OCD.
For analysis of the Eating Disorder Inventory data, chi-squares and ANOVAs were adjusted for multiple tests with the Bonferroni correction, i.e., by dividing the probability level of p<0.05 by the number of tests for eight Eating Disorder Inventory subscales, which resulted in a corrected significance level of p=0.006.
RESULTS
Retrospective analyses of the pretreatment data revealed no significant difference between the follow-up group (N=75) and the dropout group (N=18) for the following variables: the proportion of anorexia or bulimia nervosa diagnoses (χ2=0.01, df=1, p=0.94), the prevalence of concomitant OCD (χ2=1.50, df=1, p=0.22), and the pretreatment Eating Disorder Inventory total score (t=0.03, df=89, p=0.98).
At follow-up 30 months later, 38 women in the follow-up group (51%) no longer fulfilled DSM-IV criteria for anorexia or bulimia nervosa. Ten women (13%) and 27 women (36%) still met the diagnostic criteria for anorexia nervosa and bulimia nervosa, respectively. We found no significant differences in eating disorder diagnosis, eating behavior, and marital status between the groups with and without concomitant OCD (table 1).
Thirty-eight subjects (51%) reported that they had continued outpatient psychotherapy after discharge. There was no correlation between the presence or absence of concomitant OCD and outpatient continuation of psychotherapy (χ2=0.15, df=1, p=0.70).
Table 2 presents mean Eating Disorder Inventory scores at each assessment for anorectic and bulimic patients with and without concomitant OCD. ANOVAs revealed significant time effects on six of the eight subscales, which indicates a general improvement of the total group during the follow-up period. Furthermore, no significant group effects or group-by-time interactions could be identified.
At follow-up, 32 women (43%) showed clinically significant change on at least one of the eight Eating Disorder Inventory subscales, and there was no statistically significant difference between the group with concomitant OCD and the group without comorbidity: 10 of the 32 improved women (31%) had concomitant OCD and the remaining 22 (69%) did not (χ2=0.81, df=1, p=0.37).
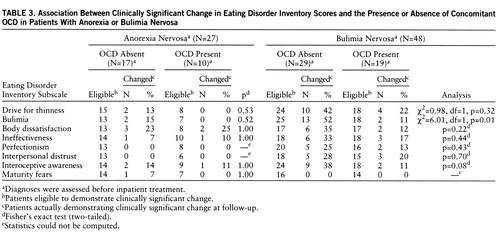
The number of patients with anorexia or bulimia nervosa who showed clinically significant change at follow-up is indicated for each Eating Disorder Inventory subscale in table 3. Patients with bulimia nervosa without concomitant OCD showed a somewhat higher percentage of clinically significant change on seven of the eight Eating Disorder Inventory subscales. This result might suggest a somewhat poorer prognosis for patients with bulimia nervosa and concomitant OCD. However, the difference between bulimic patients with and without concomitant OCD did not reach statistical significance. All in all, the anorexia nervosa group showed a poorer outcome than the bulimia nervosa group, and the correlation between clinically significant change and the presence or absence of concomitant OCD was only slight and not statistically significant.
The obsessive-compulsive behavior in each group, i.e., anorectic or bulimic patients with and without concomitant OCD, developed differently during the follow-up period. The median total score on the Hamburg Obsession-Compulsion Inventory (sum of the six subscales) decreased significantly in the group with concomitant OCD from 27 before treatment to 21 at follow-up (p=0.001, Wilcoxon matched-pairs test), while the median total score for the patients without concomitant OCD was unchanged at 19. At follow-up, the comparison of both groups revealed no significant difference in the Hamburg Obsession-Compulsion Inventory—Short Form median score (p=0.40, Mann-Whitney U test) or difference score (p=0.09, Mann-Whitney U test).
The Hamburg Obsession-Compulsion Inventory—Short Form difference score in women who showed a clinically significant change on at least one of the eight Eating Disorder Inventory subscales was higher than the difference score of those women without any clinically significant change (p=0.003, Mann-Whitney U test). This higher difference indicates a greater reduction in obsessive-compulsive symptoms in those women whose eating disorder had improved.
DISCUSSION
We examined patients with anorexia or bulimia nervosa during inpatient treatment and again 30 months after discharge to investigate whether concomitant OCD influences the prognosis of the eating disorder. Follow-up assessment revealed somewhat more clinically significant change in the group without concomitant OCD, but this trend did not reach statistical significance. In summary, the results suggest that concomitant OCD does not indicate a significantly poorer prognosis for patients with anorexia or bulimia nervosa.
To date, we are not aware of any other studies that have investigated this issue in a prospective design. Fahy and Russell (39) have reported interesting results about outcome and prognostic variables in bulimia nervosa. They used a retrospective analysis to compare pretreatment clinical features of patients with good outcome and those with poor outcome 1 year after cognitive behavior therapy and found no difference in Maudsley Obsessive-Compulsive Inventory scores between the groups. Although the method that they used was quite different from ours, the results of both studies are largely consistent.
The women who participated in our study were treated with psychodynamic therapy. Our results, therefore, indicate long-term outcome figures following this type of treatment alone. The question remains whether a different type of therapy might lead to different results. Cognitive therapy and treatment with selective serotonin reuptake inhibitors have been recommended for patients with eating disorders as well as for those with OCD (40–42). Thus, it would be interesting to investigate whether patients with eating disorders and concomitant OCD might be more responsive to these types of therapy than patients without comorbidity. Without reaching statistical significance, our results suggest that concomitant OCD predicts a somewhat poorer prognosis for patients with anorexia nervosa and particularly for patients with bulimia nervosa. A similar study that used a different type of therapy might demonstrate a clearer result.
At follow-up, the Hamburg Obsession-Compulsion Inventory scores of both patient groups were surprisingly lower than one would expect to find in patients with OCD. The decrease in obsessive-compulsive symptoms was closely correlated to the clinical improvement reflected by the scores on the Eating Disorder Inventory scales. The patients whose eating disorders were most improved at follow-up also showed the highest reduction of obsessions and compulsions. Our results are consistent with the findings of Channon and deSilva (43), who found in anorectic patients a significant reduction in Maudsley Obsessive-Compulsive Inventory scores after treatment and weight restoration.
To date, two issues remain unclear (19, 44). First, what is the reason for the association between OCD and eating disorders? Is there a connecting link or a common cause underlying both disorders? If so, is it biological or psychological in nature? Second, are obsessive-compulsive symptoms antecedents or consequences of eating disorders? We agree with Holden (15) that obsessions and compulsions may be provoked or accentuated during the course of an eating disorder, possibly as a consequence of psychological stress or biological factors, e.g., as a result of starvation. Our data demonstrated that an improvement in the eating disorder was correlated with a reduction in obsessive-compulsive symptoms. We hypothesize that the decrease in obsessive-compulsive behavior was a consequence of this improvement. Swift et al. (45, 46) have made similar observations about the relationship between depression and bulimia nervosa. Further research on this issue, including longitudinal follow-up studies and detailed psychopathological and biological assessment, might provide new insight into the relationship between eating disorders and OCD.
 |
 |
 |
Received Feb. 5, 1997; revision received May 22, 1997; accepted July 17, 1997. From the Department of Psychological Medicine and Psychotherapy, University of Innsbruck. Address reprint requests to Dr. T hiel, Department of Psychological Medicine and Psychothera p y, U niversity of Innsbruck, Sonnenburgstra<217>e 9, A-6020 Innsbruc k, Austria.
1. Fahy TA, Osacar A, Marks I: History of eating disorders in female patients with obsessive-compulsive disorder. Int J Eating Disorders 1993; 14:439–443Crossref, Medline, Google Scholar
2. Kasvikis YG, Tsakiris F, Marks IM, Basoglu M, Noshirvani HF: Past history of anorexia nervosa in women with obsessive-compulsive disorder. Int J Eating Disorders 1986; 5:1069–1075Google Scholar
3. Noshirvani HF, Kasvikis Y, Marks IM, Tsakiris F, Monteiro WO: Gender-divergent aetiological factors in obsessive-compulsive disorder. Br J Psychiatry 1991; 158:260–263Crossref, Medline, Google Scholar
4. Rubenstein CS, Pigott TA, L'Heureux F, Hill JL, Murphy DL: A preliminary investigation of the lifetime prevalence of anorexia and bulimia nervosa in patients with obsessive compulsive disorder. J Clin Psychiatry 1992; 53:309–314Medline, Google Scholar
5. Schwalberg MD, Barlow DH, Alger SA, Howard LJ: Comparison of bulimics, obese binge eaters, social phobics and individuals with panic disorder on comorbidity across DSM-III-R anxiety disorders. J Abnorm Psychol 1992; 101:675–681Crossref, Medline, Google Scholar
6. Hudson JI, Pope HG Jr, Yurgelun-Todd D, Jonas JM, Frankenburg FR: A controlled study of lifetime prevalence of affective and other psychiatric disorders in bulimic outpatients. Am J Psychiatry 1987; 144:1283–1287Google Scholar
7. Halmi KA, Eckert E, Marchi P, Sampugnaro V, Apple R, Cohen J: Comorbidity of psychiatric diagnoses in anorexia nervosa. Arch Gen Psychiatry 1991; 48:712–718Crossref, Medline, Google Scholar
8. Formea GM, Burns GL: Relation between the syndromes of bulimia nervosa and obsessive compulsive disorder. J Psychopathol Behav Assess 1995; 17:167–176Crossref, Google Scholar
9. Thiel A, Broocks A, Ohlmeier M, Jacoby GE, Schüáler G: Obsessive-compulsive disorder among patients with anorexia nervosa and bulimia nervosa. Am J Psychiatry 1995; 152:72–75Link, Google Scholar
10. Thornton C, Russell J: Obsessive compulsive comorbidity in the dieting disorders. Int J Eating Disorders 1997; 21:83–87Crossref, Medline, Google Scholar
11. Bulik CM, Beidel DC, Duchmann E, Weltzin TE, Kaye WH: Comparative psychopathology of women with bulimia nervosa and obsessive-compulsive disorder. Compr Psychiatry 1992; 33:262–268Crossref, Medline, Google Scholar
12. Pigott TA, Altemus M, Rubenstein CS, Hill JL, Bihari K, L'Heureux F, Bernstein S, Murphy DL: Symptoms of eating disorders in patients with obsessive-compulsive disorder. Am J Psychiatry 1991; 148:1552–1557Google Scholar
13. Joffe RT, Swinson RP: Eating Attitudes Test scores of patients with obsessive-compulsive disorder (letter). Am J Psychiatry 1987; 144:1510–1511Google Scholar
14. Solyom L, Freeman RJ, Miles JE: A comparative psychometric study of anorexia nervosa and obsessive neurosis. Can J Psychiatry 1982; 27:282–286Crossref, Medline, Google Scholar
15. Holden NL: Is anorexia nervosa an obsessive-compulsive disorder? Br J Psychiatry 1990; 157:1–5Google Scholar
16. Hsu LKG, Kaye W, Weltzin T: Are the eating disorders related to obsessive compulsive disorder? Int J Eating Disorders 1993; 14:305–318Google Scholar
17. Lee S: Anorexia nervosa and OCD (letter). Br J Psychiatry 1990; 157:778–779Crossref, Medline, Google Scholar
18. Rothenberg A: Eating disorder as a modern obsessive-compulsive syndrome. Psychiatry 1986; 49:45–53Crossref, Medline, Google Scholar
19. McElroy SL, Phillips KA, Keck PE: Obsessive compulsive spectrum disorder. J Clin Psychiatry 1994; 55(suppl 10):33–51Google Scholar
20. Stein DJ, Hollander E: The spectrum of obsessive-compulsive related disorders, in Obsessive-Compulsive-Related Disorders. Edited by Hollander E. Washington, DC, American Psychiatric Press, 1993, pp 241–271Google Scholar
21. Halmi KA, Broadland G, Lony J: Prognosis in anorexia nervosa. Ann Intern Med 1973; 78:907–909Crossref, Medline, Google Scholar
22. Hall RCW, Blakey RE, Hall AK: Bulimia nervosa: four uncommon subtypes. Psychosomatics 1992; 33:428–436Crossref, Medline, Google Scholar
23. Theander S: Outcome and prognosis in anorexia nervosa and bulimia. J Psychiatr Res 1985; 19:493–508Crossref, Medline, Google Scholar
24. Garner DM: Psychotherapy outcome research with bulimia nervosa. Psychother Psychosom 1987; 48:129–140Crossref, Medline, Google Scholar
25. Herzog W, Deter HC, Vandereycken W (eds): The Course of Eating Disorders. New York, Springer, 1992Google Scholar
26. Vandereycken W, Meermann R: The significance of follow-up investigation, in The Course of Eating Disorders: Long-Term Follow-Up Studies of Anorexia and Bulimia Nervosa. Edited by Herzog W, Deter H-C, Vandereycken W. Berlin, Springer-Verlag, 1992, pp 3–14Google Scholar
27. Herzog W, Munz D, KÄchele H: Analytische Psychotherapie bei Eátörungen. Stuttgart, Germany, Schattauer, 1996Google Scholar
28. Goodman WK, Price LH, Rasmussen SA, Mazure C, Fleischmann RL, Hill CL, Heninger GR, Charney DS: The Yale-Brown Obsessive Compulsive Scale, I: development, use, and reliability. Arch Gen Psychiatry 1989; 46:1006–1011Google Scholar
29. Goodman WK, Price LH, Rasmussen SA, Mazure C, Delgado P, Heninger GR, Charney DS: The Yale-Brown Obsessive Compulsive Scale, II: validity. Arch Gen Psychiatry 1989; 46:1012–1016Google Scholar
30. Hand I, Büttner-Westphal H: Die Yale-Brown Obsessive Compulsive Scale (Y-BOCS): ein halbstrukturiertes Interview zur Beurteilung des Schweregrades von Denk—und HandlungszwÄngen. Verhaltenstherapie 1991; 1:223–225Crossref, Google Scholar
31. Goodman W, Rasmussen S, Price L, Mazure L, Heninger G, Charney D: Yale-Brown Obsessive Compulsive Scale (Y-BOCS): autorisierte deutsche Übersetzung und Bearbeitung. Verhaltenstherapie 1991; 1:226–233Crossref, Google Scholar
32. Garner DM, Olmsted MP, Polivy J: Development and validation of a multidimensional eating disorder inventory for anorexia nervosa and bulimia. Int J Eating Disorders 1983; 2:15–34Crossref, Google Scholar
33. Thiel A, Paul T: Entwicklung einer deutschsprachigen Version des Eating-Disorder-Inventory (EDI). Zeitschrift für Differentielle und Diagnostische Psychologie 1988; 9:267–278Google Scholar
34. Wear RW, Pratz O: Test-retest reliability for the Eating Disorder Inventory. Int J Eating Disorders 1987; 6:767–769Crossref, Google Scholar
35. Klepsch R, Zaworka W, Hand I, Lünenschloá K, Jauernig G: Derivation and validation of the Hamburg Obsession/Compulsion Inventory—Short Form (HOCI-S). Psychol Assessment 1991; 3:196–201Crossref, Google Scholar
36. Klepsch R, Zaworka W, Hand I, Lünenschloá K, Jauernig G: Hamburger Zwangsinventar—Kurzform (HZI-K). Weinheim, Beltz Test, 1993Google Scholar
37. Jacobson NS, Truax P: Clinical significance: a statistical approach to defining meaningful change in psychotherapy research. J Consult Clin Psychol 1991; 59:12–19Crossref, Medline, Google Scholar
38. Goldbloom DS, Olmsted MP: Pharmacotherapy of bulimia nervosa with fluoxetine: assessment of clinically significant attitudinal change. Am J Psychiatry 1993; 150:770–774Link, Google Scholar
39. Fahy TA, Russell GFM: Outcome and prognostic variables in bulimia nervosa. Int J Eating Disorders 1993; 14:135–145Crossref, Medline, Google Scholar
40. American Psychiatric Association: Practice guideline for eating disorders. Am J Psychiatry 1993; 150:207–228; correction, 150:685Link, Google Scholar
41. Hand I, Goodman WK, Evers U (eds): Obsessive-Compulsive Disorders: New Research Results. Berlin, Springer-Verlag, 1992Google Scholar
42. Garner DM, Garfinkel PE (eds): Handbook of Psychotherapy for Anorexia Nervosa and Bulimia. New York, Guilford Press, 1985Google Scholar
43. Channon S, deSilva WP: Psychological correlates of weight gain in patients with anorexia nervosa. J Psychiatr Res 1985; 19:267–271Crossref, Medline, Google Scholar
44. Davis C, Kennedy SH, Ralevski E, Dionne M, Brewer H, Neitzert C, Ratusny D: Obsessive compulsiveness and physical activity in anorexia nervosa and high-level exercising. J Psychosom Res 1995; 39:967–976Crossref, Medline, Google Scholar
45. Swift WJ, Kalin NH, Wamboldt FS, Kaslow N, Ritholz M: Depression in bulimia at 2- to 5-year followup. Psychiatry Res 1985; 16:111–122Crossref, Medline, Google Scholar
46. Swift WJ, Andrews D, Barklage NE: The relationship between affective disorder and eating disorders: a review of the literature. Am J Psychiatry 1986; 143:290–299Link, Google Scholar



