Cognitive Substrates of Thought Disorder, I: The Semantic System
Abstract
Objective:Few studies have explored in detail the relation of cognitive deficits in attention, working memory, and semantics to thought disorder. The authors sought to determine whether thought disorder resides in the semantic system or elsewhere. Method:Twenty-three normal comparison subjects and 23 patients with schizophrenia participated in the study. All subjects received tests of executive function and working memory, including the Wisconsin Card Sorting Test and the Letter-Number Span test; a test of deployment of attentional resources; and tests of semantic processing and language comprehension, including the Peabody Picture Vocabulary Test, the Speed and Capacity of Language-Processing Test, the Boston Naming Test, and tests of semantic verbal fluency and phonologic verbal fluency, from which was derived a difference score. All patients were also administered the Scale for the Assessment of Thought, Language, and Communication to assess thought disorder. Results:The normal subjects were compared with the schizophrenic patients who were rated as having mild thought disorder (N=13) or moderate to severe thought disorder (N=10). While differences between the schizophrenic subgroups and the comparison subjects were observed on nearly all tests, a large difference in effect size between the two schizophrenic subgroups was apparent only in the verbal fluency difference score. In a series of multiple regression analyses, two variables made significant contributions to the prediction of positive thought disorder: the verbal fluency difference score and the Peabody Picture Vocabulary Test score. Conclusions:These results suggest that clinically rated thought disorder is associated with and may result from semantic processing abnormalities. In particular, patients with more severe thought disorder may have difficulty accessing semantic items because of disorganization of the semantic systems and, to a more limited degree, may also lack a semantic or conceptual knowledge base. Am J Psychiatry 1998; 155: 1671-1676
Thought disorder, a cardinal clinical symptom of schizophrenia, refers to abnormalities in the form of thought but not the content. It is defined by improper use of semantic and relational aspects of language and is experienced by the listener as disorganized speech. It is evident in loose associations or derailments, irrelevant or tangential responses, circumstantiality or loss of goal, and intrinsic illogicalities. When thought disorder is severe, speech can be incoherent. Bleuler believed that “peculiar association disturbances” were a most fundamental indicator of schizophrenia (1).
Current cognitive approaches to understanding thought disorder have emphasized two types of deficits. The first view involves impairments in working memory and discourse planning (2–4). From this perspective, controlled effortful processing that involves consciously organizing statements is considered to be important in the production of coherent speech. When such processing is impaired, fragmented and seemingly goalless discourse is produced. However, there are a number of difficulties with this view. First, from an introspective standpoint, much of speech is experienced as automatic, without conscious computation and formulation. Second, although working memory—the cognitive function thought to be most closely allied to strategic planning and retrieval—is impaired in schizophrenia, working memory deficits are unresponsive to neuroleptic medications, while thought disorder significantly improves with neuroleptic medications (5–9). Third, impairments in patients with thought disorder are present even in single-word association and comprehension paradigms, neither of which involves discourse planning. Moreover, patients with acquired frontal lobe lesions and concomitant working memory impairments do not exhibit thought disorder.
The second approach to thought disorder has involved attempts to define a relationship with attentional impairments. It is assumed from this perspective that patients are unable to maintain focus during language production (10). However, some of the evidence in support of this perspective is weak. For example, Nuechterlein et al. (11) found that impairments on a difficult version of the Continuous Performance Test measured during subjects’ hospitalization were associated with thought disorder only in the posthospitalization period. Some putative tests of attention may actually measure response preparation or working memory rather than distractibility (12). Patients with attention deficit hyperactivity disorder, who often exhibit impulsivity and distractibility, do not exhibit thought disorder. Last, thought disorder does not appear to maintain a strong statistical association with the presence of hallucinations and delusions, which might be thought to interfere with planning and organization in speech (13).
A variety of other approaches have been taken to examine language disturbances in schizophrenia. While schizophrenic speech may occasionally bear a resemblance to Wernicke’s aphasia because of circumstantiality or jargon, patients with such characteristics do not suffer the degree of comprehension problems associated with posterior aphasia, and they differ in other respects as well (e.g., naming ) (14, 15). Other studies have suggested that patients with schizophrenia suffer from a multilevel language disturbance that involves misuse of semantic features and phonologic features of words, as well as syntax (16). Cutting and Murphy (17) suggested that schizophrenic patients sometimes lack knowledge of the real world and thus can produce incoherent, illogical speech. Clare et al. (18) found that patients with schizophrenia performed strikingly worse than normal comparison subjects on semantic tests of sentence verification and category judgment. However, the relation between thought disorder and cognitive performance was not examined.
Despite the large number of experiments from a variety of different disciplines and perspectives, few studies have directly examined what type of cognition might be most strongly associated with thought disorder in schizophrenia. In the present study we sought to determine whether thought disorder reflects a dysfunction of the semantic system or is a result of dysfunction elsewhere. We went about this in two ways. First, we performed a series of analysis of variance (ANOVA) procedures in groups grossly distinguished clinically by greater or lesser thought disorder to determine whether semantic tests indeed showed impairment in the group of patients with thought disorder. Second, we used a series of “horse race” multiple regression equations to determine which cognitive measures best predicted thought disorder. We found that semantic processing measures, but not executive function or attentional measures, were strongly associated with thought disorder. In the second part of the study (19), we attempted to specify a cognitive mechanism that might explain this finding by using a semantic priming paradigm, and we found that aberrant spreading semantic activation was selectively correlated with other measures of semantic processing and clinically rated thought disorder.
METHOD
Twenty-three normal comparison subjects (13 male and 10 female) and 23 patients with schizophrenia (18 male and five female) participated in this study. All subjects provided written informed consent. The normal individuals had no history of current or past psychiatric treatment, no history of diagnosable substance abuse, and no history of neurologic disorder (e.g., head injury with loss of consciousness, seizures, cerebrovascular accident). All of the schizophrenic subjects were inpatients on National Institute of Mental Health research wards and met the DSM-III-R criteria for schizophrenia according to the Structured Clinical Interview for DSM-III-R (20). Fourteen patients were considered to have undifferentiated schizophrenia, five paranoid, three schizoaffective depressed, and one disorganized. Patients in the study had had multiple hospital admissions and demonstrated incomplete response to treatment. All patients were receiving neuroleptic medications at the time of the study (clozapine, N=9; risperidone, N=4; high-potency drugs, i.e., haloperidol, fluphenazine, or loxapine, N=10, of whom seven also received anticholinergic medication). The mean duration of illness in this group was 17.1 years (SD=8.6).
The mean age of the normal group was 35.5 years (SD=8.5), and the mean age of the schizophrenic group was 35.0 years (SD=14.4); the difference was not significant (t=0.14, df=44, p>0.10). The mean putative intellectual level (measured by the Wide Range Achievement Test—Revised reading score [21]) was 109.0 (SD=14.6) in the normal group, while the mean premorbid intellectual level in the schizophrenic group was 99.1 (SD=12.1) as measured by the same test. This difference was significant (t=3.40, df=44, p<0.05).
Rating Instrument for Thought Disorder
A semistructured interview was conducted with each schizophrenic patient to rate thought disorder clinically. It consisted of a general conversation about the patient’s symptoms and three probes. In the first, the patient was asked to tell a story. In the second, the patient was asked to describe several reproductions of representational paintings. In the third, the patient was asked, “Why do you think that some people believe in God?” The resulting speech samples were rated by one of the investigators (M.S.A.) using the Scale for the Assessment of Thought, Language, and Communication (22). All items were rated for each patient.
We chose this rating instrument because of its emphasis on the linguistic components of thought disorder and because of its widespread clinical and research use. We did not use the scale to assess the normal subjects, since pilot work indicated that global scores were uniformly low (N=10, mean score=0.27, range=0–0.75), thus restricting its range.
We used four scores derived from the Scale for the Assessment of Thought, Language, and Communication. The first was a global scale score based on the interviewer’s clinical impression of the severity of the patient’s thought disorder. The second score was the sum of all scale item scores (summary scale score). It should be noted that the global scores and the summary scores were highly correlated (r>0.90, N=23, p<0.01). The third score was composed of items from the scale that loaded on what was labeled a production factor in a large-scale factor analytic study conducted by Harvey et al. (23) (hereafter called the negative factor score ). The fourth score was composed of items from the scale that loaded on what was labeled a disconnection factor in the same factor analytic study (hereafter called the positive factor score). This latter factor, which includes derailment, loss of goal, poverty of content, circumstantiality, tangentiality, and incoherence, probably represents the core of clinical notions about thought disorder.
The normal comparison subjects received all of the cognitive tests listed below. The patients were interviewed to derive ratings on the Scale for the Assessment of Thought, Language, and Communication, and within 3 days of the interview, they were also administered all of the tests listed below.
Cognitive Tests
Working memory
The Wisconsin Card Sorting Test (24) has been extensively described. It is thought to involve set shifting, abstraction, hypothesis testing, and responsiveness to feedback and thus requires working memory. The number of categories attained was the dependent measure.
In the Letter-Number Span (25), the subject must order relatively short sequences of randomly presented letters and numbers. Information must thus be maintained over a short delay and transformed. Because the test demands both storage and processing, it too is considered a working memory test. The number of correct trials was the dependent measure.
Attention
The attention subtest of the Dementia Rating Scale (26) is derived from a series of tests requiring short-term verbal memory, sustained concentration, and the deployment of cognitive resources in visual search tasks. The total raw score was the dependent measure.
Semantic processing and comprehension/knowledge
In the Peabody Picture Vocabulary Test (27), the subject is required to indicate which one of four pictures best describes a word spoken by an examiner. It is thus a test of the comprehension of single words that refer to things or actions. The age-adjusted standard score was the dependent measure.
In the Speed and Capacity of Language-Processing Test (28), the subject is asked to read simple declarative sentences (e.g., “Nuns are manufactured”) and indicate whether each is true or false. The test requires knowledge of the workings of the real world. The number of errors was the dependent measure.
Semantic processing and word production
Verbal fluency tests of word production require strategic retrieval and access to phonologic/orthographic or semantic lexical information. In the phonologic fluency test, the subject is requested to name as many words as possible that begin with the letters f, a, and s in consecutive 1-minute time periods. The dependent measure was the number of words retrieved, exclusive of perseverations, repetitions of a word root, or words that began with a letter other than the one specified. In the semantic fluency test, the subject is requested to name as many animals, fruits, and vegetables as possible in consecutive 1-minute time periods, exclusive of perseverations or out-of-category words. The difference between scores on the two types of fluency was used as the dependent measure in an effort to control for retrieval and attentional factors common to both tasks. In a previous study (29) we showed that semantic fluency was differentially impaired in comparison with phonologic fluency in patients with schizophrenia.
The Boston Naming Test (30) is a test of visual confrontation naming in which the subject must retrieve (name) the word that refers to a line drawing of an object.
RESULTS
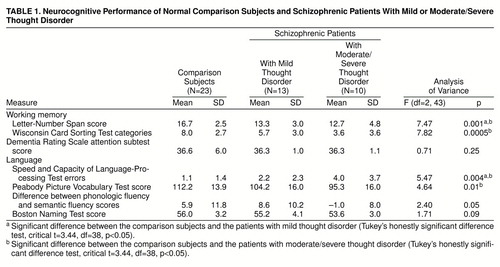
We first wished to determine whether semantic processing impairments were associated with thought disorder. We compared the scores of the normal subjects, the schizophrenic patients who had global ratings of less than 2 (i.e., no greater than mild thought disorder; N=13) on the Scale for the Assessment of Thought, Language, and Communication, and the patients who had global ratings of 2 or more (i.e., moderate to severe thought disorder; N=10) on the cognitive variables in a series of ANOVAs, followed by Tukey’s honestly significant difference post hoc t tests when the overall one-way ANOVA was significant at p<0.05 (table 1). In the contrast between the normal comparison subjects and the group with low levels of thought disorder, effect sizes were large (i.e., >0.80) for the Letter-Number Span (d=1.24) and the Wisconsin Card Sorting Test (d=0.81). In the contrast between the normal comparison subjects and the group with high levels of thought disorder, effect sizes were large for the above-noted variables (Letter-Number Span, d=1.10; Wisconsin Card Sorting Test, d=1.40) as well as the Speed and Capacity of Language-Processing Test (d=1.14) and the Peabody Picture Vocabulary Test (d=1.13). In the contrast between the groups with low and high levels of thought disorder, only the difference between phonologic fluency and semantic fluency yielded a large effect size (d=1.02). Examination of plots of individuals’ scores on this measure indicated that 60% of the patients with more severe thought disorder generated more words to phonologic cues than to semantic cues, while 31% of the normal subjects and the patients with mild thought disorder did so.
We next performed a series of multiple regression analyses of scores of the patients with schizophrenia. To ensure an appropriate variable-to-subject ratio (1:6), we chose the one variable from each of the cognitive domains (working memory, attention, comprehension/knowledge, word production) that had the highest correlation with the summary score on the Scale for the Assessment of Thought, Language, and Communication. On the basis of these criteria, the following variables were selected: scores on the difference between semantic fluency and phonologic fluency, the Peabody Picture Vocabulary Test, the Wisconsin Card Sorting Test, and the attention subtest of the Dementia Rating Scale. In the first analysis, these variables were regressed onto the positive factor score on the Scale for the Assessment of Thought, Language, and Communication with the use of SAS MAXR procedures (31). MAXR is a forward selection stepwise technique that attempts to maximize the amount of predicted variance (R2) in one-, two-, three-, four-, and n-variable solutions for any given set of n variables. For each step, MAXR determines whether removing a variable and replacing it with another increases R2. After comparing all possible combinations, it chooses the one that yields the largest R2.
At the program"s initiation we entered the four above-noted variables. We found a two-variable solution based on scree analysis (that is, three- and four-variable solutions added only trivially to the R2, i.e., about 2%.) Two variables made significant contributions: the difference between semantic fluency and phonologic fluency and the Peabody Picture Vocabulary Test score. Together they accounted for 43% of the variance in positive factor ratings on the Scale for the Assessment of Thought, Language, and Communication (table 2). Neither the working memory nor the attention measures accounted for a significant proportion of the variance. Moreover, a putative measure of intellectual function, the Wide Range Achievement Test reading score, although highly correlated with the Peabody Picture Vocabulary Test score, did not reach the significant entry criterion in a separate multiple regression analysis, nor did it correlate significantly with the difference between semantic fluency and phonologic fluency (r=0.08, N=23, p>0.10). Thus, only semantic measures appeared to be related to the positive aspect of clinically rated thought disorder in this analysis. When the same set of four variables was regressed onto the negative factor scores on the Scale for the Assessment of Thought, Language, and Communication, no combination of variables accounted for more than 10% of the variance.
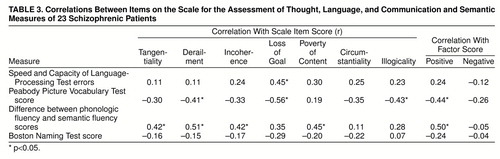
We also conducted simple first-order correlational analyses between all semantic measures and the items that loaded on the positive factor, as well as the illogicality item from the Scale for the Assessment of Thought, Language, and Communication (not included in the original Harvey et al. study). The results are shown in table 3. The difference between semantic fluency and phonologic fluency correlated highly with derailment and tangentiality, and the Peabody Picture Vocabulary Test scores correlated highly with illogicality.
DISCUSSION
Our results suggest that clinically rated thought disorder in schizophrenia is associated with and may result from semantic processing abnormalities. We found consistent deficits on various tests of semantic processing, including fluency measures and measures of comprehension and knowledge. The fluency measure discriminated between the groups with high and low levels of thought disorder. Moreover, scores on two of these tests—difference between semantic fluency and phonologic fluency and the Peabody Picture Vocabulary Test—accounted for more than 40% of the variance in clinically rated thought disorder on the Scale for the Assessment of Thought, Language, and Communication.
This particular combination of measures suggests that several subcomponents may underlie clinically rated thought disorder. First, the large verbal fluency difference scores in the schizophrenic group with moderate or severe thought disorder suggest that these patients may have difficulty accessing semantic items. This may be due to disorganization of the semantic system, since in a previous study in which multidimensional scaling was used (32), we observed that the semantic systems of patients with schizophrenia are not organized along the stereotyped dimensions that normal individuals use to organize production.
The distinction between the different types of fluency may be worthy of comment. In studies that used positron emission tomography with 15O for regional cerebral blood flow mapping, regional cortical differences between the two fluency tasks were observed (33 and unpublished manuscript by M. Gourovitch et al.). While phonologic fluency produced more activation in Broca’s area and Wernicke’s area—thought to be important in verbal working memory’s articulatory rehearsal loop (34)—semantic fluency produced relatively greater activation in temporal lobe regions, which are thought to be important in semantic processing. Thus, the distinction between the fluency tasks may be neurophysiologically plausible.
The second variable that was predictive of thought disorder, Peabody Picture Vocabulary Test scores reflecting deficient information about the meaning of words, suggests that lack of semantic or conceptual knowledge may also contribute to thought disorder. It is noteworthy that the Peabody Picture Vocabulary Test scores were highly correlated with the presence of illogicalities in speech. These findings are generally consistent with the proposal advanced by Cutting and Murphy (17). Moreover, because picture vocabulary comprehension may be relatively insensitive to the cognitive decline associated with schizophrenia (35), some mild but preexisting limitations in language processing may predispose patients to thought disorder when they become ill. However, the Peabody Picture Vocabulary Test score was a less salient contributor to thought disorder than verbal fluency.
Performance on semantic tests predicted positive but not negative thought disorder. The distinction between the two is crucial; our results suggest that they may be produced by fundamentally different mechanisms. The core features that relate to semantic processing measures in schizophrenia are those remarked upon by Bleuler (1) and involve loosening of associations: how one word follows another on the basis of meaning, and how strings of words must maintain internal logical cohesion, consistency, and relevance to environmental context.
Our work has implications for measuring thought disorder. While there have been numerous studies of the validity of various rating scales and language and working memory deficits in schizophrenia, few investigators have sought to determine the nature of cognitive mechanisms that might underlie thought disorder. Ultimately, a measure such as the difference between types of fluency, which is objective and easily obtained and has a high first-order relationship with thought disorder (r=0.52), may complement current systems of ratings. Our use of a score for the difference between two types of fluency may have effectively controlled for retrieval factors, attentional and motivational factors, and general cognitive efficiency common to both tasks. However, much work remains to be done in order to assess the validity and reliability of this measure. Moreover, because thought disorder fluctuates over time, our findings should be considered state related.
Our work may also have theoretical implications for understanding symptom structure in schizophrenia. The phenomenon that has been most strongly associated with thought disorder is bizarre behavior, marked by failures in appropriate adherence to social or cultural behavior patterns (13). Such behavior, often assumed to reflect frontal lobe failures in inhibition, may actually result from fundamental misapprehension of the semantics of actions, such that patients misjudge the meaning or context of the social situation in which they find themselves or do not consider the significance of certain acts or displays. Thus, by placing thought disorder within the semantic system, it may be more easily appreciated that thought disorder might be linked to disorganized behavior on the basis of fundamental misuse of semantics, whether involving words, social behavior, or private actions.
In conjunction with our past work, these results indicate that the language disorder present in schizophrenia may occupy a unique place in the cognitive science approaches to language. Schizophrenia appears to be characterized by disorganization of the semantic system without large decrements in amount of information (36, 37). Thus, patients exhibit relatively intact naming, expressive vocabulary, and lexical size, but on measures of the relations among lexical items (i.e., semantics), patients display marked abnormalities on putative measures of semantic space(32, 38, and unpublished manuscript by K. Tallent et al.). This stands in contrast to disorders in which there is frank corruption of semantic information, for example, Alzheimer’s disease or disorders of lexical access (39,40). Thus, recent accounts of language processing have emphasized three dissociable levels: semantic, lexical, and phonologic. Given the profile noted above (relatively intact visual confrontation naming and phonologic fluency but reduced semantic fluency, mild word comprehension deficits, and abnormalities in semantic space), evidence points to a rather selective deficit in the semantic system in schizophrenic thought disorder. Furthermore, this deficit may depend on disturbed automatic spreading semantic activation along semantic dimensions. In the second part of this study (19), using a semantic priming task, we found a strikingly high degree of association in schizophrenic patients among lack of priming for closely related words (in normal subjects, these very words result in facilitation), verbal fluency difference scores, and thought disorder. This latter result suggests a mechanism by which automatic spreading semantic activation may be aberrant in schizophrenic patients with thought disorder, such that they are unable to gain access to appropriate and relevant lexical exemplars.
Received Nov. 19, 1997; revision received May 22, 1998; accepted June 8, 1998. From the Clinical Brain Disorders Branch and the Experimental Therapeutics Branch, NIMH. Address reprint requests to Dr. Goldberg, Clinical Brain Disorders Branch, NIMH, Bldg. 10, Rm. 4S235, MSC 1379, Bethesda, MD 20892-1379.
 |
 |
 |
1. Bleuler E: Dementia Praecox or the Group of Schizophrenias (1911). New York, International Universities Press, 1950Google Scholar
2. Hoffman RS, Stopek S, Andreasen NC: A comparative study of manic versus schizophrenic speech disorganization. Arch Gen Psychiatry 1986; 43:831–838Crossref, Medline, Google Scholar
3. Manschreck TC, Maher B, Celada MT, Schneyer M, Fernandez R: Object chaining and thought disorder in schizophrenic speech. Psychol Med 1991; 21:443–446Crossref, Medline, Google Scholar
4. McGrath J: Ordering thoughts on thought disorder. Br J Psychiatry 1991; 158:307–316Crossref, Medline, Google Scholar
5. Berman KF, Zec RF, Weinberger DR: Physiologic dysfuntion of dorsolateral prefrontal cortex in schizophrenia, II: role of neuroleptic treatment, attention, and mental effort. Arch Gen Psychiatry 1986; 43:126–135Crossref, Medline, Google Scholar
6. Cleghorn JM, Kaplan RD, Szechtman B: Neuroleptic drug effects on cognitive function in schizophrenia. Schizophr Res 1990; 3:211–219Crossref, Medline, Google Scholar
7. Goldberg TE, Weinberger DR: Thought disorder, working memory, and attention: interrelationships and the effects of neuroleptic medications. Int Clin Psychopharmacol 1995; 10(suppl):99–104Google Scholar
8. Hurt SW, Holzman PS, Davis JM: Thought disorder: the measurement of its change. Arch Gen Psychiatry 1983; 40:1281–1285Crossref, Medline, Google Scholar
9. Spohn HE, Coyne L, Mittleman F: Effect of neuroleptic treatments on attention, information processing, and thought disorder. Psychopharmacology (Berl) 1985; 21:582–587Google Scholar
10. Liddle PF: Schizophrenic syndromes, cognitive performance, and neurologic dysfunction. Psychol Med 1987; 17:49–57Crossref, Medline, Google Scholar
11. Nuechterlein KH, Edell WS, Norris M: Attentional vulnerability indicators, thought disorder, and negative symptoms. Schizophr Bull 1986; 12:408–426Crossref, Medline, Google Scholar
12. Servan-Schreiber D, Cohen JD, Steingard S: Schizophrenic deficits in the processing of context: a test of a theoretical model. Arch Gen Psychiatry 1996; 53:1105–1112Crossref, Medline, Google Scholar
13. Liddle PF, Barnes TRE: Syndromes of chronic schizophrenia. Br J Psychiatry 1990; 157:558–561Crossref, Medline, Google Scholar
14. Gerson SN, Benson DF, Frazier SH: Diagnosis: schizophrenia versus posterior aphasia. Am J Psychiatry 1977; 134:966–969Link, Google Scholar
15. Grove WM, Andreasen NC: Language and thinking in psychosis: is there an input abnormality? Arch Gen Psychiatry 1985; 42:26–32Google Scholar
16. Chaika E: A linguist looks at “schizophrenic” language. Brain Lang 1974; 1:257–276Crossref, Google Scholar
17. Cutting J, Murphy D: Schizophrenic thought disorder: a psychological and organic interpretation. Br J Psychiatry 1988; 152:310–319Crossref, Medline, Google Scholar
18. Clare L, McKenna PJ, Mortimer AM, Baddeley AD: Memory in schizophrenia: what is impaired and what is preserved? Neuropsychologia 1993; 31:1225–1241Google Scholar
19. Aloia MS, Gourovitch ML, Missar D, Pickar D, Weinberger DR, Goldberg TE: Cognitive substrates of thought disorder, II: specifying a candidate cognitive mechanism. Am J Psychiatry 1998; 155:1677–1684Link, Google Scholar
20. Spitzer RL, Williams JBW, Gibbon M: Structured Clinical Interview for DSM-III-R (SCID). New York, New York State Psychiatric Institute, Biometrics Research, 1987Google Scholar
21. Kremen W, Seidman L, Faraone SV, Pepple JR, Lyons MJ, Tsuang M: The “three Rs” and neuropsychological function in schizophrenia: an empirical test of the matching fallacy. Neuropsychology 1996; 10:22–31Crossref, Google Scholar
22. Andreasen NC: Scale for the Assessment of Thought, Language, and Communication (TLC). Schizophr Bull 1986; 12:473–482Crossref, Medline, Google Scholar
23. Harvey PD, Lenzenweger MF, Keefe RSE, Pogge DL, Serper MR, Mohs RC: Empirical assessment of the factorial structure of clinical symptoms in schizophrenic patients: formal thought disorder. Psychiatry Res 1992; 44:141–151Crossref, Medline, Google Scholar
24. Heaton RK, Chelune GJ, Talley JL, Kay GG, Curtiss G: Wisconsin Card Sorting Test Manual. Odessa, Fla, Psychological Assessment Resources, 1993Google Scholar
25. Gold JM, Carpenter C, Randolph C, Goldberg TE, Weinberger DR: Auditory working memory and the Wisconsin Card Sorting Test. Arch Gen Psychiatry 1997; 54:159–168Crossref, Medline, Google Scholar
26. Kessler HR, Roth DL, Kaplan RF, Goode KT: Confirmatory factor analysis of the Mattis Dementia Rating Scale. Clin Neuropsychologist 1994; 8:451–461Crossref, Google Scholar
27. Dunn LM, Dunn LM: Peabody Picture Vocabulary Test—Revised Manual. Circle Pines, Minn, American Guidance Service, 1981Google Scholar
28. Baddeley A, Emslie H, Smith IN: The Speed and Capacity of Language-Processing Test. Bury St Edmunds, UK, Thames Valley, 1992Google Scholar
29. Gourovitch ML, Goldberg TE, Weinberger DR: Verbal fluency deficits in patients with schizophrenia: semantic fluency is differentially impaired as compared to phonologic fluency. Neuropsychology 1996; 6:573–577Crossref, Google Scholar
30. Kaplan E, Goodglass H, Weintraub S: The Boston Naming Test. Philadelphia, Lea & Febiger, 1983Google Scholar
31. SAS User"s Guide: Statistics, version 6. Cary, NC, SAS Institute, 1990Google Scholar
32. Aloia MS, Gourovitch ML, Weinberger DR, Goldberg TE: An investigation of semantic space in patients with schizophrenia. J Int Neuropsychol Society 1996; 2:267–273Crossref, Medline, Google Scholar
33. Mummery CJ, Patterson K, Hodges JR, Wise RJS: Generating tiger as an animal name or a word beginning with t: differences in brain activation. Proc R Soc Lond B 1996; 263:989–995Crossref, Medline, Google Scholar
34. Paulesu E, Frith CD, Frackowiak RS: The neural correlates of the verbal component of working memory. Nature 1993; 362:342–345Crossref, Medline, Google Scholar
35. Blatt SJ: Recall and recognition vocabulary. Arch Gen Psychiatry 1959; 1:473–476Crossref, Google Scholar
36. Allen HA, Liddle PF, Frith CD: Negative features, retrieval processes and verbal fluency in schizophrenia. Br J Psychiatry 1993; 163:769–775Crossref, Medline, Google Scholar
37. Gold JM, Hermann BP, Randolph C, Wyler AR, Goldberg TE, Weinberger DR: Schizophrenia and temporal lobe epilepsy: a neuropsychological study. Arch Gen Psychiatry 1994; 51:265–272Crossref, Medline, Google Scholar
38. Paulsen JS, Romero R, Chan A, Davis AV, Heaton RK, Jeste DV: Impairment of the semantic network in schizophrenia. Psychiatry Res 1996, 63:109–121Google Scholar
39. Damasio H, Grabowski TJ, Tranel D, Hichwa RD, Damasio AR: A neural basis for lexical retrieval. Nature 1996; 380:499–505Crossref, Medline, Google Scholar
40. Caramazza A: How many levels of processing are there in lexical access? Cognitive Neuropsychol 1997; 14:177–208Google Scholar



