Association of Panic Disorder With a History of Traumatic Suffocation
Abstract
OBJECTIVE: An important recent hypothesis suggests that panic disorder results from a false suffocation alarm. However, the association of panic disorder with a history of traumatic suffocation experiences (e.g., near-drowning and near-choking) has not been well studied. This study examined whether a history of traumatic suffocation might be more common in patients with panic disorder who have predominantly respiratory symptoms. METHOD: Patients with panic disorder (N=176) and psychiatric comparison subjects (N=60) were questioned about a history of traumatic suffocation experiences. The panic disorder patients were classified as having predominantly respiratory, cardiovascular, occulovestibular, or gastrointestinal symptoms in order to determine a possible association between traumatic suffocation and symptom subtype. RESULTS: The frequency of traumatic suffocation was significantly higher among the panic disorder patients (19.3%) than among the comparison subjects (6.7%). Within the panic disorder group, patients with a history of traumatic suffocation were significantly more likely to exhibit predominantly respiratory symptoms and nocturnal panic attacks, while patients without such a history were significantly more likely to have predominantly cardiovascular symptoms, occulovestibular symptoms, and agoraphobia. CONCLUSIONS: There may be a specific association between panic disorder and a history of traumatic suffocation, and such a history in turn appears associated with predominantly respiratory symptoms and nocturnal panic attacks. Although additional studies are needed to confirm these data, a history of traumatic suffocation might be hypothesized to play a role in the etiology of panic disorder in some patients and may provide a useful window on understanding the psychobiology of this disorder. (Am J Psychiatry 1997; 154:1566–1570)
Early work by Klein (1) on the possible differential responsivity of panic attacks and general anxiety to psychopharmacological agents provided an impetus for researchers to focus on panic disorder as a separate nosological entity. Such work has made considerable progress in recent years. The phenomenology of the disorder is now well characterized (2), the neuroanatomy and neurochemistry of panic are steadily becoming clearer (3, 4), and effective pharmacological and cognitive behavior interventions have been found (5, 6).
More recently, Klein (7) has provided an important theoretical framework for understanding much of the existing data about panic disorder. He argues that the physiological mechanisms for detecting potential suffocation are increasing Pco2 and brain lactate, and he and his colleagues review the triggering of panic attacks by CO2 inhalation (8) and lactate administration (9). Klein goes on to conclude that panic attacks occur when a suffocation monitor erroneously signals a lack of oxygen and maladaptively triggers an evolved suffocation alarm system.
This false suffocation alarm theory seems to account for the prominent symptoms of dyspnea during a panic attack (indicating a specific acute hyperventilation response to suffocation) (10) and for the chronic hyperventilation that predicts lactate-induced panic (indicating an ongoing attempt to lower Pco2) (11). The hypothesis also provides an explanation for the lack of panic in patients with absent suffocation alarms (Ondine's curse) and during pregnancy and delivery (where Pco2 is lowered) (12). Conversely, the hypothesis provides an explanation for panic attacks during relaxation and sleep, for premenstrual exacerbation of panic disorder, and for the high frequency of panic in patients with respiratory insufficiency (all of which are states characterized by increased Pco2) (13). The hypothesis also buttresses Klein's earlier differentiation between episodic spontaneous panic and chronic fear-like anxiety (in which there is hypothalamic-pituitary-adrenal [HPA] activation) (1, 14).
Nevertheless, the etiology of the putative false suffocation alarm in panic disorder remains incompletely understood. While family data suggest that genetic factors may be important (15), environmental factors might also be expected to play a role. Klein (7) noted that early separation anxiety and recent loss may be antecedents of panic disorder and speculated about whether separation anxiety may lower the suffocation alarm threshold. Nevertheless, while there is evidence for increased panic disorder after spousal bereavement (16) and parental loss (17), most patients with panic disorder do not have these antecedents.
If panic disorder is characterized by a false suffocation alarm, then an environmental factor that might be expected to play a role in this condition is an actual history of traumatic suffocation, as in near-drowning or near-choking. It has been suggested that behavioral sensitization, or an increase in response magnitude after exposure to a particular stimulus, may play an important role in the psychobiology of certain anxiety disorders (18). However, to our knowledge, the association between panic disorder and a history of traumatic suffocation has not been systematically studied.
Our hospital is situated near a range of frequently used swimming points (including the ocean, rivers, and dams), so that it is not unlikely that patients may have experienced events such as near-drowning. We therefore questioned patients with panic disorder and psychiatric comparison subjects about past experiences of traumatic suffocation. We hypothesized that the patients with panic disorder would have a history of traumatic suffocation more frequently than the comparison subjects, and that the panic disorder patients with a history of traumatic suffocation would be more likely to have predominantly respiratory symptoms than the patients without such a history.
METHOD
Subjects were drawn consecutively from an anxiety disorders clinic and a general outpatient clinic of a tertiary psychiatric hospital. All subjects were evaluated for the study by a single research psychiatrist, who then obtained informed written consent and undertook the research assessment. One hundred seventy-six patients with panic disorder (75 female and 101 male) and 60 psychiatric comparison subjects (21 female and 39 male) were included in the study.
Patients with panic disorder were included if they met the DSM-IV criteria for panic disorder with or without agoraphobia (19). Patients who met DSM-IV criteria for comorbid mood and anxiety diagnoses, including major depression and posttraumatic stress disorder (PTSD), were not excluded. Panic attacks were classified on the basis of clinical history as having predominantly respiratory symptoms (i.e., shortness of breath, smothering sensations, a choking feeling), predominantly cardiovascular symptoms (palpitations, pounding heart, accelerated heart rate), predominantly occulovestibular symptoms (dizziness, light-headedness, feeling faint), or predominantly gastrointestinal symptoms (nausea, abdominal distress) (20, 21). The patients with panic disorder were also questioned about a childhood history of substantial separation anxiety, nocturnal panic attacks, and panic disorder in first-degree relatives. Finally, the panic disorder patients were assessed with the Hamilton Depression Rating Scale (22).
Psychiatric patients were included in the comparison group if they met the DSM-IV criteria (19) for major depression or social phobia; they were excluded from the comparison group if their comorbid panic symptoms met the DSM-IV criteria for panic disorder. The comparison subjects were also assessed with the Hamilton Depression Rating Scale.
After completion of the clinical assessment, both the patients with panic disorder and the psychiatric comparison subjects were questioned about a history of traumatic suffocation experiences. They were asked specifically about accidental forms of suffocation (near-drowning in water, near-asphyxiation after fire) and deliberate forms of suffocation (strangulation, choking). When such an event had taken place, the subject was asked to describe the circumstances in detail.
Where possible, collateral information regarding childhood separation anxiety, family history of panic disorder, and circumstances of traumatic suffocation was obtained from family members.
RESULTS
There were no significant differences in age or sex ratio between the patients with panic disorder and the psychiatric comparison group. The mean age at onset of psychiatric disorder was, however, significantly earlier among the panic patients than among the comparison subjects (table 1).
In the group with panic disorder, 19.3% (N=34) of the 176 patients gave a history of a traumatic suffocation experience. In contrast, 6.7% (N=4) of the 60 psychiatric comparison subjects gave such a history. This difference was statistically significant (χ2=4.4, df=1, p=0.04).
In the group with panic disorder, the mean age at the time of the traumatic suffocation was 13 years (SD=5.4). The forms of traumatic suffocation experience were near-drowning (N=25), torture by suffocation (N=8), and choking during a rape (N=1). Near-drowning experiences had taken place in the sea (N=9), in swimming pools (N=6), near dams (N=6), or in rivers (N=4). None of the subjects had experienced near-suffocation as a component of nonforced sexual activity or in the aftermath of a fire.
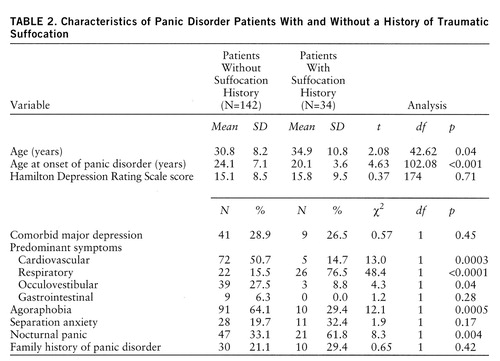
There was no significant difference in sex ratio between the 34 panic disorder patients with a history of traumatic suffocation (19 female and 15 male) and the 142 without such a history (56 female and 86 male) (χ2=2.4, df=1, p=0.12). The panic disorder patients with a history of traumatic suffocation were significantly older than the patients without such a history (table 2). Notably, however, the mean age at onset of panic disorder was significantly earlier among those with a history of traumatic suffocation. There was no significant difference between the two groups in Hamilton depression ratings or in the incidence of comorbid major depression.
In the panic disorder patients with a history of traumatic suffocation, the most common predominant symptoms were respiratory (table 2). However, in the panic disorder patients without such a history, the most common predominant symptoms were cardiovascular. In the comparison of the frequency of these predominant symptom subtypes in the two groups, the differences reached statistical significance for both of the subtypes.
The patients with a history of traumatic suffocation were significantly more likely to give a history of nocturnal panic attacks (table 2). In contrast, the patients without such a history were significantly more likely to demonstrate agoraphobia. However, there was no significant difference in the incidence of childhood separation anxiety or in the frequency of familial panic disorder.
Illustrative Case Vignettes
Case 1. A 54-year-old man presented with panic disorder that had begun at age 24. His panic attacks were characterized by predominantly respiratory symptoms. On questioning about traumatic suffocation experiences, the patient recalled having been swept out to sea at age 8. He described this as a very scary experience—he had been washed out by a strong current, had been unable to breathe, and had lost consciousness. By chance he was saved by a bather, who performed mouth-to-mouth resuscitation. The patient also noted that during his panic attacks, he sometimes relived this near-drowning experience.
Case 2. A 31-year-old man presented with panic disorder. Typically, his panic attacks were characterized by predominantly respiratory symptoms, and there were also frequent nocturnal panic attacks. On questioning about traumatic suffocation experiences, the patient recalled having been tortured as a political prisoner at age 18. A wet bag had been placed over his head repeatedly, leading to choking feelings, hyperventilation, and panic. At about age 20 the patient began to experience spontaneous panic attacks. The characteristic reexperiencing, avoidant, and numbing symptoms of PTSD were less prominent.
Case 3. A 29-year-old man presented with panic disorder of 12 years' duration. His panic attacks were characterized by predominantly respiratory symptoms, and he also suffered from nocturnal panic attacks. On questioning about a history of traumatic suffocation, the patient recalled a near-drowning experience at age 13. While swimming in a river, he had stepped off a sandy shelf into deep water. He went down for what seemed an interminable length of time and could not find the surface again. Fortunately, he was seen by his father, who rescued him.
DISCUSSION
The main findings of this study were that 1) there was a significantly higher incidence of traumatic suffocation experiences, both accidental (near-drowning) and deliberate (torture by suffocation), in the patients with panic disorder than in the psychiatric comparison subjects, and 2) within the group of panic disorder patients, those with a history of traumatic suffocation were significantly more likely to exhibit predominantly respiratory symptoms and nocturnal panic attacks, while those without such a history were significantly more likely to exhibit predominantly cardiovascular symptoms and agoraphobia.
The contribution of environmental factors to panic disorder has been noted by other authors. Klein (7) cited descriptions of “gas hysteria” during World War I, when entire army units broke ranks and ran without provocation. Cocoon-like protective masks caused either panic or marked anxiety and hyperventilation in a substantial percentage of soldiers. Similarly, several studies have described “mass hysteria” precipitated by peculiar odors and the sight of distressed hyperventilating persons (7). Finally, early separation anxiety, loss, and grief have been associated with an increased incidence of panic disorder (16, 17, 23). Thus, environmental triggering of panic disorder may reflect an increase in the salience of cues relevant to suffocation (e.g., gas hysteria) or may reflect specific physiological changes to the suffocation alarm (e.g., early loss).
While evidence of an association between panic disorder and traumatic suffocation may suggest a causal relationship, the data here cannot be said to demonstrate causality. It is possible, for example, that patients with panic disorder have enhanced recall of past dyspneic episodes. Nevertheless, it is also possible that an episode of actual suffocation acts physiologically to sensitize a putative suffocation alarm, which is then more easily triggered at a later point. Certainly, such an explanation seems useful in explaining the association between a history of traumatic suffocation and predominantly respiratory symptoms (which would effectively decrease Pco2). Similarly, this explanation appears useful in explaining the association between a history of traumatic suffocation and nocturnal panic attacks (during sleep there is an increase in Pco2).
The data from this study are consistent with a view of panic disorder as a heterogeneous entity, with patients differing across a number of phenomenological and psychobiological variables. It is well-known that in panic disorder there is variability in a number of features, including clinical phenomenology, comorbid axis I and II disorders, and response to treatment. Nevertheless, the idea that panic disorder can be subtyped according to symptom profile is perhaps less widely accepted, and this aspect of our method and findings may therefore be questioned. It is notable, however, that a number of early descriptions of what can now be recognized as panic attacks focused on cardiac symptoms—then denoted as “soldier's heart,” “irritable heart,” and so on (20, 24)—while other descriptions of panic disorder have emphasized respiratory symptoms as a central feature (7, 10, 25). In addition, a number of empirical studies have suggested that patients do experience certain symptoms more than others, thus allowing subtyping (20, 21, 26–31). In the most comprehensive of these studies, Briggs et al. (21) found that patients in the Cross-National Panic Study could be divided on the basis of a number of statistical analyses into two groups characterized by the presence or absence of prominent respiratory symptoms. Our method is supported by this work, and our findings are consistent with it. Further work is necessary, however, to determine the reliability and validity of the clinical subtyping used here.
Briggs and colleagues (21) found that patients with panic disorder in whom prominent respiratory symptoms were present and those in whom they were absent differed in both panic phenomenology and response to treatment. Patients with prominent respiratory symptoms had more spontaneous panic attacks and responded better to imipramine, whereas patients without prominent respiratory symptoms had more situational panic attacks and responded somewhat better to alprazolam. Briggs et al. noted that the existence of a group of patients with prominent respiratory symptoms and spontaneous panic seemed to support the suffocation alarm hypothesis. Similarly, our finding that patients with a history of near-drowning were more likely to have respiratory symptoms and less likely to have agoraphobia seems consistent with these earlier data.
Our data do not adequately address the question of whether patients with panic disorder who do not provide a history of traumatic suffocation are unable to recall these experiences, have experienced other environmental triggers of panic disorder, or have had greater genetic loading for panic disorder. Nevertheless, panic disorder patients with and without a history of traumatic suffocation did not differ in the frequency of childhood separation anxiety or familial panic disorder, providing a preliminary suggestion that the two groups may have similar genetic predispositions to the development of panic disorder.
The frequency with which panic disorder is associated with traumatic suffocation and the particular kinds of suffocation experience reported here may well be peculiar to the specific setting of the study. Our hospital is situated near a range of frequently used swimming places, so that near-drowning experiences are perhaps unusually common. In addition, torture of political prisoners by suffocation appears to have been a method commonly used by security police of the apartheid regime in our area. These particular forms of traumatic suffocation are likely to be far more infrequent in other regions. The extent to which panic disorder is associated with traumatic suffocation and the nature of suffocation experiences in other regions are questions for future research.
The association we found between deliberate traumatic suffocation and subsequent panic disorder raises the question of whether there is also an association between comorbid panic in patients with PTSD and suffocation at the time of the precipitating stressor. Certainly, PTSD is characterized by hyperarousal symptoms, and panic symptoms in this disorder may simply reflect noradrenergic hyperactivity. Nevertheless, it is not unlikely that patients who develop PTSD after war, rape, or domestic violence have experienced deliberate traumatic suffocation within these contexts. Determining whether this is indeed the case seems to be another interesting question for further research.
The data presented here also suggest several avenues for future neurobiological research on panic disorder. The neurobiology of panic disorder may depend on whether patients have panic attacks only or whether there is also development of fear anxiety (i.e., fear of having panic attacks). In patients with panic attacks only, HPA axis function may be normal, while in patients with fear anxiety, HPA axis function may be abnormal (7). Indeed, patients with predominantly respiratory symptoms demonstrate increased spontaneous panic attacks and response to imipramine, while patients without predominantly respiratory symptoms demonstrate increased situational panic attacks and response to alprazolam (21). Similarly, we would speculate that in persons with panic disorder associated with a history of traumatic suffocation, there is less likely to be evidence of fear anxiety and HPA abnormalities than in those with panic disorder without such a history. Similarly, imipramine and selective serotonin reuptake inhibitors—which may act by resetting the threshold of the false suffocation alarm in panic disorder (7)—would be effective in the treatment of persons with panic disorder associated with traumatic suffocation, and these patients would less frequently require benzodiazepines for the treatment of fear anxiety.
In conclusion, the data presented here suggest that there may be a specific association between panic disorder and a history of traumatic suffocation, and that such a history may in turn correlate positively with predominantly respiratory symptoms and nocturnal panic attacks and negatively with predominantly cardiovascular symptoms and agoraphobia. Although additional studies are needed to replicate these data and to determine their generalizability to other geographical regions, a history of traumatic suffocation might be hypothesized to play a role in the etiology of panic disorder in some patients, and this suggests several avenues for further phenomenological and psychobiological research on the disorder.
 |
 |
Received July 19, 1996; revision received March 24, 1997; accepted May 1, 1997. From the Department of Psychiatry, Faculty of Medicine, University of Stellenbosch. Address reprint requests to Dr. Bouwer, Department of Psychiatry, University of Stellenbosch, P.O. Box 19063, Tygerberg 7505, South Africa. Dr. Stein is supported by a grant from the Medical Research Council of South Africa and the Lundbeck Fellowship.
1. Klein DF: Delineation of two drug-responsive anxiety syndromes. Psychopharmacologia 1964; 5:397–408Crossref, Medline, Google Scholar
2. Fyer AJ, Mannuzza S, Endicott J: Differential diagnosis and assessment of anxiety: recent developments, in Psychopharmacology: The Third Generation of Progress. Edited by Meltzer HY. New York, Raven Press, 1987, pp 1177–1203Google Scholar
3. Gorman JM, Liebowitz MR, Fyer AJ, Stein J: A neuroanatomical hypothesis for panic disorder. Am J Psychiatry 1989; 146:148–161Link, Google Scholar
4. Coplan JD, Gorman JM, Klein DF: Serotonin related functions in panic-anxiety: a critical overview. Neuropsychopharmacology 1992; 6:189–200Medline, Google Scholar
5. Klein DF, Klein HM: The definition and psychopharmacology of spontaneous panic and phobia: a critical review, in Psychopharmacology of Anxiety. Edited by Tyrer PJ. New York, Oxford University Press, 1989, pp 135–162Google Scholar
6. Barlow DH: Anxiety and Its Disorders: The Nature and Treatment of Anxiety and Panic. New York, Guilford Press, 1988Google Scholar
7. Klein DF: False suffocation alarms, spontaneous panics, and related conditions: an integrative hypothesis. Arch Gen Psychiatry 1993; 50:306–317Crossref, Medline, Google Scholar
8. Papp LA, Klein DF, Gorman JM: Carbon dioxide hypersensitivity, hyperventilation, and panic disorder. Am J Psychiatry 1993; 150:1149–1157Google Scholar
9. Liebowitz MR, Fyer AJ, Gorman JM, Levitt M, Dillon D, Levy G, Anderson S, Levitt M, Palij M, Davies SO, Klein DF: Lactate provocation of panic attacks, I: clinical and behavioral findings. Arch Gen Psychiatry 1984; 41:764–770Crossref, Medline, Google Scholar
10. Anderson DJ, Noyes R Jr, Crowe RR: A comparison of panic disorder and generalized anxiety disorder. Am J Psychiatry 1984; 141:572–575Link, Google Scholar
11. Papp LA, Martinez JM, Klein DF, Ross D, Liebowitz MR, Fyer AJ, Hollander E, Gorman JM: Arterial blood gas changes in panic disorder and lactate-induced panic. Psychiatry Res 1989; 28:171–180Crossref, Medline, Google Scholar
12. Pine DS, Weese-Mayer DE, Silvestri JM, Davies M, Whitaker AH, Klein DF: Anxiety and congenital central hypoventilation syndrome. Am J Psychiatry 1994; 151:864–870Link, Google Scholar
13. Yellowlees PM, Haynes S, Pitts N, Ruffin RE: Psychiatric morbidity in patients with life-threatening asthma: initial report of a controlled study. Med J Aust 1988; 149:246–249Crossref, Medline, Google Scholar
14. Klein DF: Anxiety reconceptualized, in Anxiety: New Research and Changing Concepts. Edited by Klein DF, Rabkin JG. New York, Raven Press, 1981, pp 235–262Google Scholar
15. Weissman MM: Family genetic studies of panic disorder. J Psychiatr Res 1993; 27(suppl 1):S69–S78Google Scholar
16. Jacobs S, Hansen F, Kasl S, Ostfeld A, Berkman L, Kim K: Anxiety disorders during acute bereavement: risk and risk factors. J Clin Psychiatry 1990; 51:269–274Medline, Google Scholar
17. Tweed JL, Schoenbach VJ, George LK, Blazer DG: The effects of childhood parental death and divorce on 6-month history of anxiety disorders. Br J Psychiatry 1989; 154:823–828Crossref, Medline, Google Scholar
18. Charney DS, Deutch AY, Krystal JH, Southwick SM, Davis M: Psychobiologic mechanisms of posttraumatic stress disorder. Arch Gen Psychiatry 1993; 50:294–305Crossref, Google Scholar
19. First MB, Spitzer RL, Gibbon M, Williams JB: Structured Clinical Interview for DSM-IV Axis I Disorders. New York, New York State Psychiatric Institute, Biometrics Research, 1994Google Scholar
20. Lelliott P, Bass C: Symptom specificity in patients with panic. Br J Psychiatry 1990; 157:593–597Crossref, Medline, Google Scholar
21. Briggs AC, Stretch DD, Brandon S: Subtyping of panic disorder by symptom profile. Br J Psychiatry 1993; 163:201–209Crossref, Medline, Google Scholar
22. Hamilton M: A rating scale for depression. J Neurol Neurosurg Psychiatry 1960; 23:56–62Crossref, Medline, Google Scholar
23. Gittelman-Klein R, Klein DF: The relationship between separation anxiety and panic and agoraphobic disorders. Psychopathology 1984; 17:56–65Crossref, Medline, Google Scholar
24. Skerritt PW: Anxiety and the heart—a historical review. Psychol Med 1983; 13:17–25Crossref, Medline, Google Scholar
25. Bass C, Kartsounis L, Lelliott P: Hyperventilation and its relationship to anxiety and panic. Integrative Psychiatry 1987; 5:274–291Google Scholar
26. Aronson TA, Logue CM: Phenomenology of panic attacks: a descriptive study of panic disorder patients' self-reports. J Clin Psychiatry 1988; 49:8–13Medline, Google Scholar
27. Verberg K, Griez E, Meijer J, Pols H: Respiratory disorders as a possible predisposing factor for panic disorder. J Affect Disord 1995; 33:129–134Crossref, Medline, Google Scholar
28. Katon W: Panic disorder and somatization. Am J Med 1984; 77:101–106Crossref, Medline, Google Scholar
29. Lydiard RB, Laraia MT, Howell EF, Ballenger JC: Can panic disorder present as irritable bowel syndrome? J Clin Psychiatry 1986; 47:470–473Google Scholar
30. Stein MB, Asmundson GJG, Ireland D, Walker JR: Panic disorder in patients attending a clinic for vestibular disorders. Am J Psychiatry 1994; 151:1697–1700Google Scholar
31. Clark DB, Hirsch BE, Smith MG, Furman JM, Jacob RG: Panic in otolaryngology patients presenting with dizziness or hearing loss. Am J Psychiatry 1994; 151:1223–1225Google Scholar



