Bipolar II Postpartum Depression: Detection, Diagnosis, and Treatment
Abstract
Research on postpartum mood disorders has focused primarily on major depressive disorder, bipolar I disorder, and puerperal psychosis and has largely ignored or neglected bipolar II disorder. Hypomanic symptoms are common after delivery but frequently unrecognized. DSM-IV does not consider early postpartum hypomania as a significant diagnostic feature. Although postpartum hypomania may not cause marked impairment in social or occupational functioning, it is often associated with subsequent, often disabling depression. Preliminary evidence suggests that bipolar II depression arising in the postpartum period is often misdiagnosed as unipolar major depressive disorder. The consequences of the misdiagnosis can be particularly serious because of delayed initiation of appropriate treatment and the inappropriate prescription of antidepressants. Moreover, no pharmacological or psychotherapeutic studies of bipolar postpartum depression are available to guide clinical decision making. Also lacking are screening instruments designed specifically for use before or after delivery in women with suspected bipolar depression. It is recommended that the treatment of postpartum bipolar depression follow the same guidelines as the treatment of nonpuerperal bipolar II depression, using medications that are compatible with lactation.
Bipolarity and the Postpartum Period
Bipolar spectrum disorder generally includes bipolar I disorder, bipolar II disorder, and bipolar disorder not otherwise specified (1) . Bipolar I disorder is characterized by recurrent episodes of mania and depression, while bipolar II disorder is defined as recurrent episodes of depression and hypomania. The illness course in bipolar disorder not otherwise specified is also punctuated with manic and depressive symptoms, but the disorder does not reach the DSM-IV threshold criteria for bipolar I or II disorder. There is accumulating evidence that the majority of bipolarity exists beyond the realm of bipolar I disorder. The U.S. National Comorbidity Survey Replication Study reported lifetime prevalence estimates of 1.0% for bipolar I disorder, 1.1% for bipolar II disorder, and 2.4% for bipolar disorder not otherwise specified (2) .
Despite the combined high prevalence of bipolar II disorder and bipolar disorder not otherwise specified, research on postpartum mood disorders has focused primarily on major depressive disorder, mania, and puerperal psychosis. While the nosological status of postpartum psychosis remains a topic of debate, it is usually a manifestation of bipolar disorder triggered by childbirth. The study of postpartum bipolarity beyond bipolar I disorder has been largely ignored; consequently, there are scant data on the prevalence of depressive presentations in bipolar II disorder and bipolar disorder not otherwise specified. Freeman et al. (3) reported that 67% of 30 women with bipolar I and II disorder had a postpartum mood episode within 1 month of delivery; in the eight women who had experienced episodes following their first delivery, the recurrence rate following a subsequent delivery was 100%. Identified postpartum episodes were almost exclusively of the depressive type. Another study (4) found that approximately 20% of women with bipolar disorder retrospectively reported having postpartum mood episodes, mainly of the depressive type. Compared to women with major depressive disorder, those with bipolar disorder are more likely to have episodes of postpartum depression; however, no prospective studies have been conducted to ascertain the comparative prevalence of postpartum depression in women with major depression and those with bipolar disorder.
Misdiagnosis of bipolar depression as major depressive disorder during the postpartum period appears to be common. For example, Sharma et al. (5) reported that 54% of 56 outpatients seen consecutively with the referral diagnosis of postpartum depression were rediagnosed as having a lifetime diagnosis of bipolar disorder. In terms of frequency of occurrence, the primary diagnoses in this sample were major depressive disorder (46%), bipolar disorder not otherwise specified (29%), bipolar II disorder (23%), and bipolar I disorder (2%). Thirty percent of patients had a positive screen for bipolar spectrum disorder on the Mood Disorders Questionnaire, and 86% of those who screened positive met DSM-IV criteria for a diagnosis of bipolar disorder; however, only a small number (10%) of these patients reported receiving a past diagnosis of bipolar disorder.
Postpartum Hypomania
Hypomanic symptoms are common after delivery, with various studies reporting rates in the range of 9%–20% (6 – 8) . While no comparative studies have been conducted on the prevalence of hypomania during the puerperium compared with the nonpuerperal periods, the rates of hypomania reported in various studies are higher than the lifetime prevalence of bipolar disorder. It has been suggested that postpartum hypomania does not simply reflect happiness at having a baby but is a manifestation of bipolar disorder (9) . Associated symptoms include increased goal-directed activity, overtalkativeness, racing of thoughts, decreased sleep requirement, distractibility, and irritability. In contrast, the “baby blues” denotes a brief period of mild emotional disturbance characterized by dysphoria, tearfulness, mood lability, insomnia, irritability, and anxiety. Symptoms of the baby blues occur in up to 80% of women in the few days after delivery and usually remit by the 10th day. Even though elation has been reported in some studies as a symptom of the baby blues, the symptoms of postpartum hypomania can be distinguished because of their onset on postpartum day 1 rather than day 3 or 4, as in the baby blues (9) . The peak prevalence of hypomanic symptoms is immediately after delivery, although the risk remains elevated for several weeks. Postpartum hypomania itself does not cause marked impairment in social or occupational functioning, but its clinical significance lies in its association with bipolar depression later in the postpartum period (10) .
Consequences of Missed Postpartum Bipolarity
Hypomania after delivery may be misconstrued as the normal joy related to the experience of motherhood. Because DSM-IV does not acknowledge hypomania as a postpartum-onset specifier, there is neither sufficient awareness of nor screening for this presentation. Consequently, clinicians may not inquire about episodes of mood elevation, and women may fail to report hypomanic symptoms and focus on symptoms of depression. There are no screening instruments designed specifically for use before or after delivery in women with bipolar disorder. Commonly used screening instruments, such as the Edinburgh Postnatal Depression Scale, have not been validated in women with bipolar disorder. Thus, women with bipolar II disorder and bipolar disorder not otherwise specified may be misdiagnosed as having major depressive disorder in the postpartum period. Brockington et al. (11) noted that unipolar postpartum depression can be distinguished from postpartum bipolar depression; he found that an early onset of depression (within 2 weeks of delivery) and a characteristic clinical profile—less anger, less self-rated emotion, and more animation—represent a clinical entity related to bipolar disorder.
The misdiagnosis of bipolar disorder as major depressive disorder frequently results in a delay in the initiation of appropriate treatment. The consequences of misdiagnosis can be particularly serious as treatment with antidepressants may precipitate mania, a mixed state, or rapid cycling and thereby increase the risk for psychiatric hospitalization. The injudicious use of antidepressants in patients with a bipolar diathesis has also been linked to polypharmacy and treatment refractoriness (12) .
Treatment and Prevention
Pharmacological Management
As in trials of antidepressants in nonpuerperal major depression, patients with bipolar disorder are routinely excluded from clinical trials in postpartum depression. Despite the lack of efficacy and safety data, antidepressants are regularly used as first-line pharmacotherapy in the management of bipolar postpartum depression. Sharma (13) reported three cases of early-onset postpartum depression in which bipolarity manifested after antidepressant treatment. There was no past history of psychiatric disturbance, but in each case, family history was positive for bipolar disorder. Treatment with antidepressants resulted in a highly unstable illness course, and discontinuation of antidepressants and initiation of mood stabilizers and atypical antipsychotics resulted in sustained improvement.
Two retrospective studies (N=101 and N=27) (14 , 15) and a prospective study (N=26) (16) evaluated the impact of prophylactic treatment with mood stabilizers on postpartum mood episodes in women with bipolar I or II disorder. The results of these studies supported the use of lithium and carbamazepine but not divalproex in the reduction of postpartum recurrences. A prospective cohort study of 25 women with bipolar I or II disorder (17) found that olanzapine alone or in combination with an antidepressant or mood stabilizer was associated with a lower risk of postpartum mood episodes than treatment with antidepressants, mood stabilizers, or no medication (18% versus 57%) for a minimum of 4 weeks after delivery. No studies have been conducted on atypical antipsychotics in the management of postpartum depression in women with bipolar disorder; however, evidence exists for quetiapine as a first-line choice in the acute treatment of bipolar II disorder (18) .
Medications and Breastfeeding
Treatment during lactation requires minimizing infant exposure and adverse effects while maintaining optimum maternal mental health. In women with bipolar disorder, the benefits of breastfeeding should also be carefully balanced against the deleterious effect of sleep deprivation in triggering mood episodes. Consideration should be given to using the breast pump to allow others to assist with feeding, formula feeding, or supplementation of breast milk with formula in order to maximize consecutive hours of sleep.
In general, carbamazepine and valproate are considered compatible with breastfeeding. Lamotrigine should be used cautiously because of concerns about skin rash and higher-than-expected drug levels in the infant after exposure through breastfeeding, even though only 60% of the drug is transferred to the breast milk (19) . The use of lithium during lactation has typically been discouraged because of concerns that it may be secreted at high levels in milk and that infants may not clear it efficiently (20) . However, in light of the recent data showing no significant adverse clinical or behavioral effects in the infants, breastfeeding while taking lithium should be considered in carefully selected women. According to Viguera et al. (21) , suitable clinical characteristics include stable maternal mood, lithium monotherapy or a simple medication regimen, adherence to infant monitoring recommendations, a healthy infant, and a collaborative pediatrician.
There is preliminary evidence supporting the use of quetiapine during breastfeeding (22) , even though data on the safety of the atypical antipsychotics in lactating women are limited. In order to minimize the number of medications to which the infant is exposed during lactation, it is advisable to continue with the medication that was effective during pregnancy. For patients who are not receiving medication, a previously effective medication should be considered rather than trying a new one for which there may be more data on lactation. The infant’s pediatrician should be made aware of any medications that the mother is taking while breastfeeding.
Nonpharmacological Management
Psychoeducation and emotional support for the partner and other family members are important, and family members should be kept informed of the patient’s condition, treatment plan, and expected outcome. Help with nocturnal infant care should be recommended to minimize the patient’s sleep disruption. Once the patient’s condition is stable, issues such as parenting skills and maternal-infant bonding should be addressed. There have been no studies of psychotherapy for postpartum depression in bipolar II disorder and bipolar disorder not otherwise specified; however, social rhythm therapy that stresses maintaining a regular schedule of daily activities and stability in personal relationships should be considered to help attain and reinforce mood stability (23) .
Summary and Recommendations
Postpartum treatment of women with bipolar II disorder and bipolar disorder not otherwise specified is challenging because of the lack of diagnostic instruments designed for postpartum mood presentations and a paucity of psychopharmacological data to guide clinical decision making. Given the prevalence of bipolarity and the potentially serious consequences of its misdiagnosis, pregnant women should be universally screened for bipolar disorder by inquiring about personal and family history of bipolar disorder. This will permit early identification, formal risk assessment, and management planning, including close follow-up during the period of risk. It can provide an opportunity to address avoidable risk factors, such as general stress and sleep disruption, in late pregnancy and the early postpartum period. Women with postpartum depression in particular should be routinely screened for mania and hypomania. Until a validated assessment tool is established, the Mood Disorder Questionnaire may be useful for screening for bipolar disorder in pregnant and postpartum women (1) . The Highs scale (9) is not a diagnostic instrument, but it can be valuable in eliciting the symptoms of hypomania. The presence of clinical features, such as atypical features (DSM-IV criteria), racing of thoughts, and psychotic symptoms, during a depressive episode should serve as a clue to the bipolar nature of depression. Screening should include questions about a family history of bipolar disorder. Early initiation of appropriate management can improve the patient’s quality of life, which can significantly affect her family and her child’s early development.
Because insufficient research has been conducted on the treatment of postpartum bipolar II disorder, definitive recommendations cannot be made. Until there is more research and stronger evidence, the treatment of bipolar postpartum depression should follow the same guidelines as the treatment of nonpuerperal bipolar II depression (18) , provided the selected medications are compatible with lactation. For acute management, treatment options include quetiapine, lamotrigine, lithium, valproate, quetiapine plus lamotrigine, and lithium plus lamotrigine. For prophylactic treatment, lithium, lamotrigine, or an atypical antipsychotic, such as olanzapine and quetiapine, should be considered. Antidepressant monotherapy should be avoided for prophylactic and acute treatment. For women with bipolar disorder who are already receiving an antidepressant, the need for its continued use in the maintenance treatment of depression should be evaluated because antidepressants may perpetuate instability of the illness course.
For women who appear to have significant bipolar illness in the postpartum setting, consideration should be given to the continued use of stabilizing medication after the first postpartum year. If medication is discontinued, it is advisable to continue psychiatric monitoring beyond the first postpartum year in order to ensure ongoing maternal emotional stability. Women should be carefully monitored for mood stability during subsequent pregnancies and postpartum periods. Consideration should be given to whether to use prophylactic management with previously effective medications or careful monitoring and prompt initiation of medications that have been effective in the past.
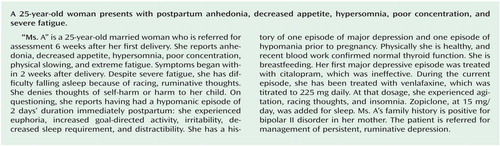
In the case vignette, the patient was thought to have bipolar II disorder, depressed phase, with postpartum onset. Clues to the bipolar nature of the depression included a history of postpartum hypomania, atypical symptoms of depression (hypersomnia and psychomotor retardation), family history of bipolar disorder, and a loss of antidepressant response. Collateral history obtained from her husband confirmed the diagnosis of bipolar II disorder. The venlafaxine dose was gradually tapered off and she was started on lamotrigine. During withdrawal from venlafaxine the patient’s insomnia worsened, leading her treatment team to substitute 25 mg of quetiapine for the zopiclone she had been taking at bedtime. She was unable to tolerate a higher dose of quetiapine because of excessive sedation and postural hypotension. The treatment team decided to try lamotrigine, at 150 mg daily, because of its ease of use (no laboratory monitoring) and safety during lactation compared to lithium. The patient reported a significant and sustained improvement in her condition after the addition of lamotrigine.
1. Hirschfeld RMA, Williams JBW, Spitzer RL, Calabrese JR, Flynn L, Keck PE Jr, Lewis L, McElroy SL, Post RM, Rapport DJ, Russell JM, Sachs GS, Zajecka J: Development and validation of a screening instrument for bipolar spectrum disorder: the Mood Disorder Questionnaire. Am J Psychiatry 2000; 157:1873–1875Google Scholar
2. Merikangas KR, Akiskal HS, Angst J, Greenberg PE, Hirschfeld RM, Petukhova M, Kessler RC: Lifetime and 12-month prevalence of bipolar spectrum disorder in the National Comorbidity Survey Replication. Arch Gen Psychiatry 2007; 64:543–552Google Scholar
3. Freeman MP, Smith KW, Freeman SA, McElroy SL, Kmetz GE, Wright R, Keck PE Jr: The impact of reproductive events on the course of bipolar disorder in women. J Clin Psychiatry 2002; 63:284–287Google Scholar
4. Payne JL, Roy PS, Murphy-Eberenz K, Weismann MM, Swartz KL, McInnis MG, Nwulia E, Mondimore FM, MacKinnon DF, Miller EB, Nurnberger JI, Levinson DF, DePaulo JR Jr, Potash JB: Reproductive cycle-associated mood symptoms in women with major depression and bipolar disorder. J Affect Disord 2007; 99:221–229Google Scholar
5. Sharma V, Khan M, Corpse C, Sharma P: Missed bipolarity and psychiatric comorbidity in women with postpartum depression. Bipolar Disord 2008; 10:742–747Google Scholar
6. Webster J, Pritchard MA, Creedy D, East C: A simplified predictive index for the detection of women at risk for postnatal depression. Birth 2003; 30:101–108Google Scholar
7. Farías ME, Wenk E, Cordero M: Adaptación de la Escala Highs Para la Detección de Sintomatología Hipomaníaca en el Puerperio. Trastornos del Animo 2007; 3:27–36Google Scholar
8. Heron J, Craddock N, Jones I: Postnatal euphoria: are “the highs” an indicator of bipolarity? Bipolar Disord 2005; 7:103–110Google Scholar
9. Glover V, Liddle P, Taylor A, Adams D, Sandler M: Mild hypomania (the highs) can be a feature of the first postpartum week: association with later depression. Br J Psychiatry 1994; 164:517–521Google Scholar
10. Lane A, Keville R, Morris M, Kinsella A, Turner M, Barry S: Postnatal depression and elation among mothers and their partners: prevalence and predictors. Br J Psychiatry 1997; 171:550–555Google Scholar
11. Brockington I, Margison F, Schofield E, Knight R: The clinical picture of the depressed form of puerperal psychosis. J Affect Disord 1998; 15:29–37Google Scholar
12. Sharma V, Khan M, Smith A: A closer look at treatment resistant depression: is it due to a bipolar diathesis? J Affect Disord 2005; 84:251–257Google Scholar
13. Sharma V: A cautionary note on the use of antidepressants in postpartum depression. Bipolar Disord 2006; 8:411–414Google Scholar
14. Viguera AC, Nonacs R, Cohen LS, Tondo L, Murray A, Baldessarini RJ: Risk of recurrence of bipolar disorder in pregnant and nonpregnant women after discontinuing lithium maintenance. Am J Psychiatry 2000; 157:179–184Google Scholar
15. Cohen LS, Sichel DA, Robertson LM, Heckscher E, Rosenbaum JF: Postpartum prophylaxis for women with bipolar disorder. Am J Psychiatry 1995; 152:1641–1645Google Scholar
16. Wisner K, Hanusa B, Peindl K, Perel J: Prevention of postpartum episodes in women with bipolar disorder. Biol Psychiatry 2004; 56:592–596Google Scholar
17. Sharma V, Smith A, Mazmanian D: Olanzapine in the prevention of postpartum psychosis and mood episodes in bipolar disorder. Bipolar Disord 2006; 8:400–404Google Scholar
18. Yatham LN, Kennedy SH, Schaffer A, Parikh SV, Beaulieu S, O’Donovan C, MacQueen G, McIntyre RS, Sharma V, Ravindran A, Young LT, Young AH, Alda M, Milev R, Vieta E, Calabrese JR, Berk M, Ha K, Kapczinski F: Canadian Network for Mood and Anxiety Treatments (CANMAT) and International Society for Bipolar Disorders (ISBD) collaborative update of CANMAT guidelines for the management of patients with bipolar disorder: update 2009. Bipolar Disord 2009; 11:225–255Google Scholar
19. Liporace J, Kao A, D"Abreu A: Concerns regarding lamotrigine and breast feeding. Epilepsy Behav 2004; 5:102–105Google Scholar
20. Chaudron LH, Jefferson JW: Mood stabilizers during breastfeeding: a review. J Clin Psychiatry 2000; 61:79–90Google Scholar
21. Viguera AC, Newport DJ, Ritchie J, Stowe Z, Whitfield T, Mogielnicki J, Baldessarini RJ, Zurick A, Cohen LS: Lithium in breast milk and nursing infants: clinical implications. Am J Psychiatry 2007; 164:342–345Google Scholar
22. Gentile S: Infant safety with antipsychotic therapy in breast-feeding: a systematic review. J Clin Psychiatry 2008; 69:666–673Google Scholar
23. Frank E, Kupfer D, Thase M, Mallinger A, Swartz H, Fagiolini A, Grochocinski V, Houck P, Scott J, Thompson W, Monk T: Two-year outcomes for interpersonal and social rhythm therapy in individuals with bipolar I disorder. Arch Gen Psychiatry 2005; 62:996–1004Google Scholar



