Randomized, Controlled Trial of the Effectiveness of Short-Term Dynamic Psychotherapy and Cognitive Therapy for Cluster C Personality Disorders
Abstract
OBJECTIVE: This study compared the effectiveness of short-term dynamic psychotherapy and cognitive therapy for outpatients with cluster C personality disorders. METHOD: Patients (N=50) who met the criteria for one or more cluster C personality disorders and not for any other personality disorders were randomly assigned to receive 40 weekly sessions of short-term dynamic psychotherapy or cognitive therapy. The most common axis I disorders in the patient group were anxiety and depression diagnoses. Therapists were experienced, full-time clinicians and were receiving manual-guided supervision. Outcome variables included symptom distress, interpersonal problems, and core personality pathology. Measures were administered repeatedly during and after treatment, and change was assessed longitudinally by means of growth modeling procedures. RESULTS: The overall patient group showed, on average, statistically significant improvements on all measures during treatment and also during a 2-year follow-up period. Significant changes in symptom distress after treatment were found for the group of patients who received short-term dynamic psychotherapy but not for the cognitive therapy patients. Despite these differences in intragroup changes, no statistically significant differences between the short-term dynamic psychotherapy group and cognitive therapy group were found on any measure for any time period. Two years after treatment, 54% of the short-term dynamic psychotherapy patients and 42% of the cognitive therapy patients had recovered symptomatically, whereas approximately 40% of the patients in both groups had recovered in terms of interpersonal problems and personality functioning. CONCLUSIONS: Both short-term dynamic psychotherapy and cognitive therapy have a place in the treatment of patients with cluster C personality disorders. However, factors other than treatment modality may discriminate better between successful and poor outcomes. Such factors should be explored in future studies.
The cluster C disorders are the most prevalent personality disorders in the general population (1) (one of 10 individuals) and in outpatient clinic populations (2) (more than one of two patients). Moreover, the presence of any cluster C personality disorder is invariably associated with poorer outcomes in the treatment of axis I disorders (3–5).
In light of these findings, it is puzzling to find such a paucity of controlled trials examining the effectiveness of individual psychotherapy in this population. Among the handful of studies that have been conducted, only one (6) can be categorized as a randomized, controlled trial specifically designed to study the course of these disorders during and after treatment. In that study, 81 patients with predominantly cluster C disorders (70%) showed significant and equivalent improvement on measures of distress and social functioning after 40 sessions of two forms of dynamic psychotherapy. Furthermore, treated patients did significantly better than wait-list comparison subjects, and gains were maintained at 1.5-year follow-up. In two additional randomized, controlled trials, data for subgroups of patients with predominantly cluster C disorders were analyzed separately within larger trials designed to study major depression (3, 4). The studies found that patients with personality disorders responded equally well to interpersonal psychotherapy and cognitive behavior therapy (3) and equally well to psychodynamic-interpersonal therapy and cognitive behavior therapy (4). Finally, in one uncontrolled study, 38 patients with obsessive-compulsive and avoidant personality disorders treated with time-limited supportive-expressive therapy demonstrated significant average changes on diagnostic measures and on measures of distress, interpersonal problems, and personality functioning (7).
The present study extends the study by Winston et al. (6) by examining the effects of 40-session, short-term dynamic psychotherapy specifically designed for personality problems (8) and comparing those effects not with another form of dynamic therapy but with an alternative approach, that is, cognitive therapy. To our knowledge, this study provides the first empirical evidence of the effects of a form of cognitive therapy specifically intended for patients with personality dysfunction (9). This study also takes notice of the suggestion of Perry et al. (10) that the effects of specific therapies for specific personality disorders should be examined.
Method
Patients
During the 5-year recruitment period, a total of 127 patients referred by two large psychiatric outpatient clinics, family doctors, and psychiatrists and psychologists in private practice were screened by an intake evaluator who was an experienced clinician and researcher. Patients were included if they were between ages 18 and 65 years and if they met the criteria for one or more DSM-III-R cluster C personality disorders or self-defeating personality disorder (which was included among the proposed diagnostic categories needing further study that were described in Appendix A of DSM-III-R). All diagnostic evaluations were audio- or videotaped and were performed by the intake evaluator with the Structured Clinical Interview for DSM-III-R (SCID-II) (11). A second diagnostician, an experienced clinical psychologist, reviewed a random sample of 20 SCID-II interviews. The combined agreement on the presence of one or more cluster C diagnoses and on the absence of any other axis II disorder was 0.77 (Cohen’s kappa). The patients who met the inclusion criteria and who did not meet the criteria for any cluster A or cluster B personality disorder returned within a week for a second diagnostic interview with the intake evaluator, who used the SCID-I interview to obtain DSM-III-R axis I diagnoses (12). Additional exclusion criteria were current or past psychotic disorder, current substance dependence or abuse, current eating disorder, organic brain disorder and other serious physical illness, active suicidal behavior, refusal to have the therapy sessions videotaped, and refusal to discontinue other active treatment. A total of 51 patients were included. After completing a number of self-report questionnaires and undergoing a psychodynamically oriented evaluation interview by a second evaluator, patients were presented with a full description of the study’s procedures, gave their written consent to participate, and were subsequently randomly assigned to receive 40 weekly sessions of either dynamic or cognitive therapy. Except for one patient who, in agreement with the therapist, terminated after childbirth midtherapy, all patients completed treatment in accord with the preplanned schedule of 40 sessions.
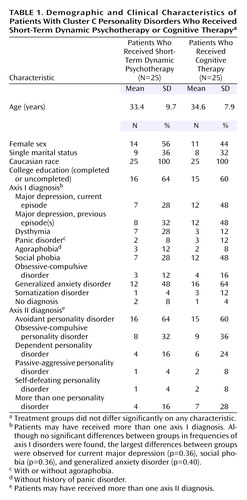
The demographic and clinical characteristics of the patients are shown in Table 1.
Treatments and Therapists
In both treatments, sessions were 50 minutes long, videotaped, and held once weekly. All therapists treated at least one patient as a training exercise before treating the patients who were enrolled in the study.
Short-term dynamic psychotherapy
McCullough Vaillant’s short-term dynamic psychotherapy model (8) follows the fundamental structure of psychodynamic psychotherapy as outlined by Malan’s triangle of conflict (i.e., defenses and anxieties block the expression of feelings) and triangle of person (i.e., work with conflicts in relation to the therapist and current and past persons). Specifically, the therapist 1) gently clarifies rather than confronts defenses, 2) empathizes with and exposes the underlying, conflicted affect, and 3) helps to regulate rather than to provoke anxiety. Three main treatment objectives represent the hypothesized change mechanisms: defense restructuring (recognizing and relinquishing defenses), affect restructuring (desensitization of affects through exposure to conflicted feeling), and self/other restructuring (alteration of maladaptive conceptions of self/others). The overall goal of this model of short-term dynamic psychotherapy is for previously avoided affects such as sadness/grief, anger, or tenderness to be experienced and expressed adaptively by the patient.
The short-term dynamic psychotherapy therapist team consisted of three psychiatrists and five clinical psychologists. All but one were in full-time clinical practice. Their general clinical experience ranged in length from 2 to 14.5 years (mean=9.2, SD=3.6), their experience with short-term dynamic psychotherapy in general ranged from 1.2 to 10.5 years (mean=6.0, SD=2.8), and their experience with this model of short-term dynamic psychotherapy for personality disorders ranged from 1.2 to 7.2 years (mean=4.7, SD=1.9). The therapist training program for short-term dynamic psychotherapy encompassed weekly 2-hour video-based peer supervision meetings and 2-day supervision seminars with Dr. McCullough Vaillant twice annually. Treatment integrity and adherence to the treatment manual (8), including the achievement of the treatment objectives, were carefully monitored during these supervision activities, which included the active use of rating scales by Dr. McCullough Vaillant. Each therapist treated an average of three patients (range=2–4).
Cognitive therapy
Equipped with the cognitive model of personality disorders (9), the therapist specifically 1) deals during initial sessions with any coexisting axis I problems, 2) teaches the patient to identify and evaluate key negative automatic thoughts, 3) structures the sessions carefully and builds a collaborative and trusting relationship with the patient, 4) employs guided imagery to unravel the meaning of new and earlier experiences, 5) in collaboration with the patient prepares homework assignments tailored to the patient’s specific issues, and 6) applies specific cognitive, behavioral, and emotion-focused schema restructuring techniques to dispute core beliefs and to develop new and more adaptive beliefs and behaviors. Two main treatment objectives represent the hypothesized change mechanisms: first, to help the patient develop new and more adaptive core beliefs, and second, to help the patient develop more adaptive problem-solving interpersonal behaviors.
The cognitive therapy therapist team consisted of six clinical psychologists. All but one were full-time clinicians. Their general clinical experience ranged in length from 6 to 21 years (mean=11.2, SD=4.3), their experience with cognitive therapy in general ranged from 1.2 to 9.8 years (mean=5.9, SD=2.4), and their experience with cognitive therapy for personality disorders ranged from 1.2 to 7.5 years (mean=4.1, SD=1.8). The training program for the therapists who provided cognitive therapy encompassed weekly 2-hour video-based peer supervision meetings and, twice annually, supervision seminars with visiting cognitive therapy experts (e.g., J. Beck, A. Freeman, J. Young). Treatment integrity and adherence to the manual (9) were closely monitored during the weekly supervision activities. Each therapist treated an average of four patients (range=1–5).
Treatment Integrity and Differentiability
Systematic checks on the integrity and differentiability of the two treatments were performed by two independent raters (with 2 and 4 years of clinical experience, respectively) using the Inventory of Therapeutic Strategies (13). The Inventory of Therapeutic Strategies rates therapists’ interventions in terms of categories of intention (exploratory, supportive, or work enhancing), content, and object focus (e.g., therapist, others, self). Raters reviewed an entire early session (typically the sixth) and subsequently rated the frequency of Inventory of Therapeutic Strategies categories plus agenda setting and homework assignment. In analyses of data for categories that were rated reliably (r>0.65; range=0.65–0.83, mean=0.73), two-tailed t tests showed that short-term dynamic psychotherapy and cognitive therapy differed in their emphasis on supportive strategies (t=2.2, df=48, p<0.02; cognitive therapy had the stronger emphasis), work with defenses (t=4.0, df=48, p<0.001; short-term dynamic psychotherapy had the stronger emphasis), transference work (i.e., therapist as focus) (t=3.33, df=48, p=0.002; short-term dynamic psychotherapy had the stronger emphasis), agenda setting (t=9.9, df=48, p<0.0001; cognitive therapy had the stronger emphasis), and homework assignment (t=5.6, df=48, p<0.0001; cognitive therapy had the stronger emphasis). As for work enhancing strategies, the emphases were equally strong in the two treatments (t=0.03, df=48, p=0.50).
Outcome Measures
A measure of symptom distress was provided by the Global Severity Index of the SCL-90-R (14).
The total mean score of the full version (127 items) of the Inventory of Interpersonal Problems (15) was used to assess patients’ problems with assertiveness, intimacy, sociability, submissiveness, control, and responsibility for others.
The Millon Clinical Multiaxial Inventory (16), a 175-item questionnaire, was used to assess personality pathology as reflected by the cluster C personality disorder scales of avoidant, dependent-submissive, compulsive-conforming, and passive-aggressive, which have proved diagnostically efficient and congruent with DSM-III personality disorder diagnoses. Two Millon Clinical Multiaxial Inventory indices were computed: the total mean raw score on the four cluster C scales and the proportion of patients with a base rate score above 74, which represents the cutoff for “a prominent clinical syndrome” (16).
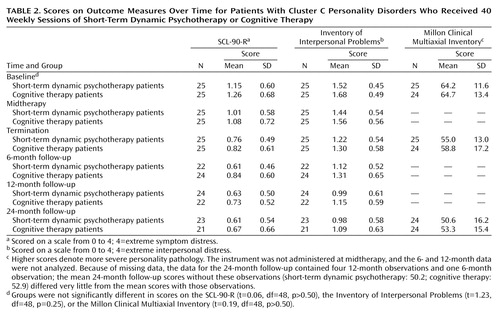
These measures were administered repeatedly during treatment and follow-up. See Table 2 for details regarding the timing of data collection.
Statistical Analysis
Given our data collection design and our desire to include all available time-series data in our analyses, data from the SCL-90-R and Inventory of Interpersonal Problems were analyzed by using hierarchical linear models in order to utilize more fully the information inherent in the data (17). The hierarchical linear models that we used consisted of a within-patient and a between-patient model. The former (level 1) captured change over time for each patient plus termination status on the measures. The between-patient model (level 2) estimated the effect of treatment type on rates of change and status. At level 1, a two-piece linear model enabled us to capture rates of change during treatment and follow-up plus termination status for each patient. A two-piece model was chosen to allow for the analysis of the nonlinear change pattern exhibited by the plots of the patients’ time-series. In addition, we wanted to assess change and the effect of the two treatments in each of the two key phases. The analyses were conducted by using the HLM 5 computer program (18).
The Millon Clinical Multiaxial Inventory scores were analyzed by using paired t tests to assess change over time and by using independent t tests to compare the treatment effects at termination and 2-year follow-up. Since a hierarchical linear model normally requires at least three observations per patient, hierarchical linear model analysis was not considered an option for the Millon Clinical Multiaxial Inventory data. The Millon Clinical Multiaxial Inventory was not administered midtherapy because we reasoned that personality pathology would be less sensitive to change over the brief interval of 20 sessions.
On the basis of a two-tailed t test, an alpha of 0.05, and 25 patients in each group, power to detect a medium-sized effect (d=0.50) was 0.41 (19) for the comparison of short-term dynamic psychotherapy and cognitive therapy. Power to detect a large effect (d=0.80) was 0.79.
Results
Descriptive and Preliminary Analyses
Means and standard deviations for the outcome measures are shown in Table 2 along with baseline equivalence results.
Therapist effects
Based on several one-way analyses of variance, the therapists were found to be equally effective (p values from 0.26 to 0.61, mean=0.40)
Attrition, additional therapy, and medication
One of the 51 patients discontinued treatment; her baseline data were not included in the analyses. One short-term dynamic psychotherapy patient and one cognitive therapy patient did not attend any of the follow-up assessments.
Two patients in each condition received additional psychotherapy (8–20 sessions) between their 6- and 24-month follow-ups. In addition, one short-term dynamic psychotherapy patient used antidepressants during part of follow-up. Since, in separate analyses, the effect of additional treatment was found to be small (as measured by the SCL-90-R) or negligible (as measured by the Inventory of Interpersonal Problems), their follow-up data were included in the analyses.
Three short-term dynamic psychotherapy patients and two cognitive therapy patients used hypnotics, and two short-term dynamic psychotherapy patients and one cognitive therapy patient used antidepressants during part of the treatment phase. The effect of medication on rates of change was found to be very small.
Effectiveness
Psychiatric symptoms and interpersonal problems
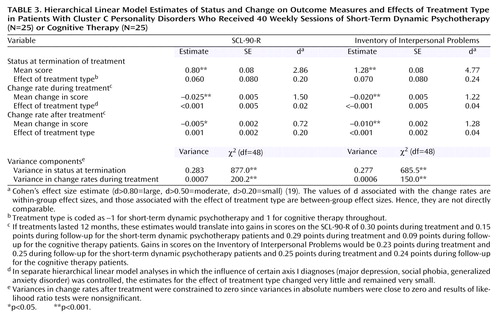
In fitting a two-piece hierarchical linear model to the data, the estimates of change during treatment indicated (Table 3) that for the overall patient group, SCL-90-R and Inventory of Interpersonal Problems scores, on average, were decreasing by 0.025 (p<0.0001) and 0.020 (p<0.0001) points per month, respectively. Furthermore, patients continued to improve after treatment, as indicated by decreases in scores on the SCL-90-R (0.005 points per month, p=0.03) and on the Inventory of Interpersonal Problems (0.010 points per month, p<0.0001).
Table 3 also shows that the estimates of the effects of treatment type on termination status (p=0.40 and p=0.47) and on rates of change were close to zero (p=0.52–0.92) and were not statistically significant and that the corresponding effect sizes (d) were small. Thus, the improvement trajectories for short-term dynamic psychotherapy and cognitive therapy patients were, on average, highly similar as measured by both the SCL-90-R and the Inventory of Interpersonal Problems.
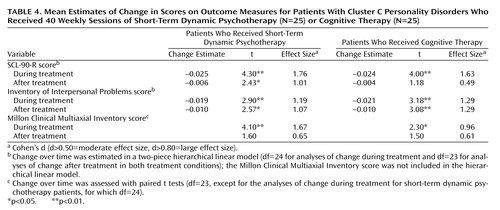
Finally, we examined the rates of change for each treatment group separately. As Table 4 shows, within-group effect sizes were generally large for symptom distress and interpersonal problems both during and after treatment. It is noteworthy, however, that the estimate of symptom change during follow-up for short-term dynamic psychotherapy patients was statistically significant, while the estimate for cognitive therapy patients was not significant. Even though the mean rate of symptom change during follow-up for short-term dynamic psychotherapy patients was almost twice as large as that of cognitive therapy patients, the difference between those rates was statistically nonsignificant (p>0.40) (Table 3). This nonsignificant finding is related to the fact that the intervals within which the true change rates lie were fairly wide (for short-term dynamic psychotherapy patients: from –0.012 to –0.001; for cognitive therapy patients: from –0.010 to 0.003) and overlapped a great deal.
Personality pathology
Cluster C personality pathology as assessed by the raw scores on the Millon Clinical Multiaxial Inventory changed significantly and favorably for the overall patient group during treatment (t=4.40, df=48, p<0.0001, d=1.25) and during follow-up (t=3.96, df=47, p<0.001, d=1.15). Effects for each treatment analyzed separately are shown in Table 4. There were no significant differences between groups at termination (t=0.90, df=48, p=0.40, d=0.26) or at follow-up (t=0.59, df=46, p>0.50, d=0.18). Change in personality pathology was also assessed by using the Millon Clinical Multiaxial Inventory’s base rate score; scores above 74 signify a prominent cluster C syndrome (16). A prominent cluster C syndrome was found in 88% of the short-term dynamic psychotherapy patients at baseline, 72% at termination, and 50% at 2-year follow-up. For cognitive therapy patients the percentages were nearly identical: 87.5% at baseline, 72% at termination, and 50% at 2-year follow-up. The drop from baseline to follow-up indicates a 43% reduction.
Clinically Significant Change
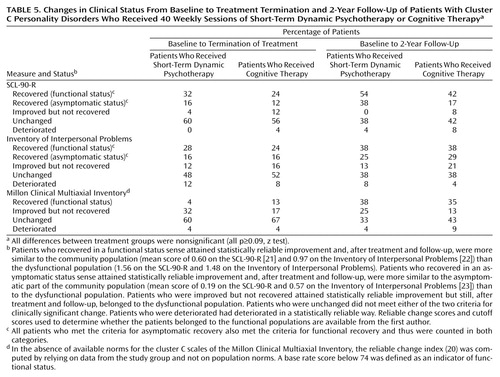
Essentially, clinically significant change has to do with the return to normal functioning (20). As defined in this study, clinically significant change occurs when 1) a patient moves from a dysfunctional population to a functional or normal population during treatment and 2) the magnitude of a patient’s change is statistically reliable. If a patient’s change meets both of these criteria, he or she is classified as recovered (20), i.e., as having returned to normal functioning.
On the basis of these criteria, patients are routinely categorized as 1) recovered (meeting both criteria), 2) as improved but not recovered, 3) as deteriorated, in the case of negative change (meeting the second criterion only), or 4) as unchanged (meeting neither criterion) (20). In this study, patient termination and 24-month follow-up scores were compared to scores for two functional or normal populations—a general community sample (21, 22) and a community sample of subjects who had been screened and found to be asymptomatic (23).
The percentages of patients in each of the four categories described in the previous paragraph are shown in Table 5. It appears that the percentages of patients who were unchanged or deteriorated at termination ranged from 60% to 71% (mean=62.5%) at termination of treatment and from 37% to 51% (mean=44.6%) at 2-year follow-up. Difference between the two means was significant (p<0.0001, z test). Among patients who recovered symptomatically (as measured by the SCL-90-R), it appears that at 2-year follow-up one of two short-term dynamic psychotherapy patients and two of five cognitive therapy patients were part of the general community population, while about two of five short-term dynamic psychotherapy patients and one of six cognitive therapy patients had joined the asymptomatic community population. As measured by the Inventory of Interpersonal Problems and the Millon Clinical Multiaxial Inventory, differences between groups in recovery rates were very small. As expected, relatively more patients returned to functional status (the general community population) than to asymptomatic status, and relatively more patients had recovered by 2-year follow-up than by treatment termination. As measured by the Millon Clinical Multiaxial Inventory, this latter difference was statistically significant for the short-term dynamic psychotherapy patients (p=0.002, z test; d=1.01) and approached significance for the cognitive therapy patients (p=0.053, z test; d=0.58).
Discussion
The large within-group effect sizes on all measures for short-term dynamic psychotherapy patients during treatment are in line with the findings of Winston et al. (6). In fact, for the SCL-90-R, the measure that the two studies had in common, the effect size for short-term dynamic psychotherapy patients in the current study was three times higher than the effect size for the short-term dynamic psychotherapy patients in the study by Winston et al. (d=1.76, compared to d=0.59) and two times higher than the effect size for patients who received an alternative form of brief dynamic psychotherapy in the study by Winston et al. (d=1.76, compared to d=0.95).
Unlike the patients in many other psychotherapy outcome studies, the patients in this study on average continued to improve significantly after treatment. With respect to interpersonal problems, for instance, effect sizes for both treatments were large (short-term dynamic psychotherapy: d=1.07; cognitive therapy: d=1.29), and about 40% of the patients had recovered by 2 years after treatment. Similar recovery rates were found for core personality pathology. This finding of continued improvement supports one of the original justifications for short-term approaches articulated by short-term therapy pioneers such as Sifneos (24). They argued that in successful short-term therapy, patients would, through an internalized therapeutic dialogue and other mechanisms, be able to achieve gains on their own after termination (24).
When the mean effects of the two treatments were contrasted, no statistically significant differences emerged for any of the measures during any of the time periods. As noted earlier, statistical power to detect medium-sized differences (see footnote a, Table 3, and reference 19) was insufficient, and, as a consequence, the risk of accepting a false no-difference result (i.e., a type II error) was increased. In such a situation there is reason to question whether the mean values observed on the measures in the two groups were truly equivalent. To cast more light on that suspicion, we conducted post hoc equivalency tests (25) using the mean initial status and change rates (Table 3 and Table 4) for the outcome measures. The results showed that for the Millon Clinical Multiaxial Inventory, but not for the SCL-90-R and Inventory of Interpersonal Problems, the difference between groups was small enough to declare the change rates equivalent (i.e., within an interval of ±20% around a zero difference). Thus, it can be concluded with some confidence that the small differences between groups with respect to change in core personality pathology during and after treatment are of trivial clinical importance. However, these test results do not allow us to make equally confident conclusions about the clinical unimportance of the differential treatment effects for symptom distress and interpersonal problems. In fact, the finding of the fairly large differences between groups in rates of clinically significant change as measured by the SCL-90-R (Table 5) lends credence to the conclusion that the differences in symptom distress between groups may be clinically important and nontrivial.
Although recovery rates generally tended to be greater when the 2-year follow-up period was also included in the analyses, this tendency was particularly strong, and in fact was statistically significant for the short-term dynamic psychotherapy patients, for outcomes measured with the Millon Clinical Multiaxial Inventory. This result may be seen as a delayed effect of the treatments. As such, this finding supports the notion of Howard et al. (26) that changes in life functioning, including personality functioning, are slower to occur than changes in subjective well-being and distress. This finding may also indicate that the Millon Clinical Multiaxial Inventory captured different domains of psychopathology than did the SCL-90-R and the Inventory of Interpersonal Problems.
Another limitation, in addition to the insufficient power to detect medium-sized effects, was the lack of observer-rated measures. As noted by Perry et al. (10), it is a strength to include both observer-rated and self-report measures. To mitigate the initial reactivity of many self-report measures, Perry et al. recommended long-term follow-up when using such measures. We incorporated that recommendation and observed continuing strong effects on the measures after treatment. It is worth noting that Perry et al. found that self-report measures produce smaller effects than observer-rated ones. This finding may indicate that self-report measures tend to yield more conservative estimates of treatment effects in these patient populations.
We did not include a no-treatment comparison group due to ethical issues involved in withholding treatment in this population and because of the abundant evidence (27) that psychotherapy in general is more effective than no therapy. Instead, for comparison groups, we used normative samples to assess the status of treated patients after treatment.
The findings of this study await replication in larger groups of patients and with different teams of therapists. In future studies it would be most important also to identify the characteristics of patients who do and do not have a response to treatment.
 |
 |
 |
 |
 |
Received June 4, 2002; revisions received Dec. 4, 2002, and April 23, 2003; accepted May 5, 2003. From the Department of Psychiatry, Norwegian University of Science and Technology, Trondheim, Norway. Address reprint requests to Dr. Svartberg, Department of Psychiatry, Mount Sinai Hospital, 600 University Ave., Toronto, Ont. M5G 1X5, Canada; [email protected] (e-mail). Supported by grants from the Norwegian Research Council. The authors thank Leigh McCullough for supervision of the dynamic therapists and comments on an earlier version of the manuscript; M. van Beelen, T. Haug, O. Hummelsund, P.J. Ingstad, B. Jansen, T. Johnsen, R. Leland, B. Engum, K. Røsdal, S. Sævareid, T. Tande, and P. Vogel for conducting the therapy; O. Røkkum and E. Røsshag for conducting the ratings; and K. Choi for help with data analysis.
1. Torgersen S, Kringlen E, Cramer V: The prevalence of personality disorders in a community sample. Arch Gen Psychiatry 2001; 58:590–596Crossref, Medline, Google Scholar
2. Alnæs R, Torgersen S: DSM-III symptom disorders (axis I) and personality disorders (axis II) in an outpatient population. Acta Psychiatr Scand 1988; 78:348–355Crossref, Medline, Google Scholar
3. Shea MT, Pilkonis PA, Beckham E, Collins JF, Elkin I, Sotsky SM, Docherty JP: Personality disorders and treatment outcome in the NIMH Treatment of Depression Collaborative Research Program. Am J Psychiatry 1990; 147:711–718Link, Google Scholar
4. Hardy GE, Barkham M, Shapiro DA, Stiles WB, Rees A, Reynolds S: Impact of cluster C personality disorders on outcomes of contrasting brief psychotherapies for depression. J Consult Clin Psychol 1995; 63:997–1004Crossref, Medline, Google Scholar
5. Reich JH, Vasile RG: Effects of personality disorders on the outcome of axis I conditions. J Nerv Ment Dis 1993; 181:475–484Crossref, Medline, Google Scholar
6. Winston A, Laikin M, Pollack J, Samstag LW, McCullough L, Muran JC: Short-term psychotherapy of personality disorders. Am J Psychiatry 1994; 151:190–194Link, Google Scholar
7. Barber JP, Morse JQ, Krakauer ID, Chittams J, Crits-Christoph K: Change in obsessive-compulsive and avoidant personality disorders following time-limited supportive-expressive therapy. Psychotherapy 1997; 34:133–143Crossref, Google Scholar
8. McCullough Vaillant L: Changing Character. New York, Basic Books, 1997Google Scholar
9. Beck AT, Freeman A: Cognitive Therapy for Personality Disorders. New York, Guilford, 1990Google Scholar
10. Perry JC, Banon E, Ianni F: Effectiveness of psychotherapy for personality disorders. Am J Psychiatry 1999; 156:1312–1321Abstract, Google Scholar
11. Spitzer RL, Williams JBW, Gibbon M, First MB: Structured Clinical Interview for DSM-III-R Personality Disorders (SCID-II). Washington, DC, American Psychiatric Press, 1990Google Scholar
12. Spitzer RL, Williams JBW, Gibbon M, First MB: User’s Guide for the Structured Clinical Interview for DSM-III-R (SCID). Washington, DC, American Psychiatric Press, 1990Google Scholar
13. Gaston L, Thompson L, Gallagher D, Cournoyer L-G, Gagnon R: Alliance, technique, and their interactions in predicting outcome of behavioral, cognitive and brief dynamic therapy. Psychother Res 1998; 8:190–209Crossref, Google Scholar
14. Derogatis LR: SCL-90-R: Administration, Scoring, and Procedures Manual, II. Towson, Md, Clinical Psychometric Research, 1983Google Scholar
15. Horowitz LM, Rosenberg SE, Baer BA, Ureno G, Villasenor VS: Inventory of Interpersonal Problems: psychometric properties and clinical applications. J Consult Clin Psychol 1988; 56:885–892Crossref, Medline, Google Scholar
16. Millon T: Millon Clinical Multiaxial Inventory, 3rd ed. Minneapolis, National Computer Services, 1984Google Scholar
17. Raudenbush SW, Bryk AS: Hierarchical Linear Models: Applications and Data Analysis Methods, 2nd ed. Newbury Park, Calif, Sage Publications, 2001Google Scholar
18. Raudenbush SW, Bryk AS, Cheong YF, Congdon R: HLM 5: Hierarchical Linear and Nonlinear Modeling. Lincolnwood, Ill, Scientific Software International, 2000Google Scholar
19. Cohen J: Statistical Power Analysis for the Behavioral Sciences, 2nd ed. Hillsdale, NJ, Lawrence Erlbaum Associates, 1988Google Scholar
20. Jacobson NS, Roberts LJ, Berns SB, McGlinchey JB: Methods for defining and determining the clinical significance of treatment effects: description, application, and alternatives. J Consult Clin Psychol 1999; 67:300–307Crossref, Medline, Google Scholar
21. Holi MM, Sammallahti PR, Aalberg VA: A Finnish validation study of the SCL-90. Acta Psychiatr Scand 1998; 97:42–46Crossref, Medline, Google Scholar
22. Hansen NB, Lambert MJ: Brief report: assessing clinical significance using the Inventory of Interpersonal Problems. Assessment 1996; 3:133–136Crossref, Google Scholar
23. Tingey RC, Lambert MJ, Burlingame GM, Hansen NB: Clinically significant change: practical indicators for evaluating psychotherapy outcome. Psychother Res 1996; 6:144–153Crossref, Medline, Google Scholar
24. Sifneos PE: Short-Term Anxiety-Provoking Psychotherapy: A Treatment Manual. New York, Plenum, 1992Google Scholar
25. Rogers JL, Howard KI, Vessey JT: Using significance tests to evaluate equivalence between two experimental groups. Psychol Bull 1993; 113:553–565Crossref, Medline, Google Scholar
26. Howard KI, Lueger RJ, Maling M, Martinovich Z: A phase model of psychotherapy outcome: causal mediation of change. J Consult Clin Psychol 1993; 61:678–685Crossref, Medline, Google Scholar
27. Lambert MJ, Bergin AE: The effectiveness of psychotherapy, in Handbook of Psychotherapy and Behavior Change, 4th ed. Edited by Bergin AE, Garfield SL. New York, John Wiley & Sons, 1994, pp 141–150Google Scholar



