Variables That Affect the Clinical Use and Abuse of Methylphenidate in the Treatment of ADHD
Abstract
OBJECTIVE: Methylphenidate, the most common treatment for attention deficit hyperactivity disorder (ADHD), increases extracellular dopamine in the brain, which is associated with its reinforcing as well as its therapeutic effects. The authors evaluated variables that distinguish these two properties. METHOD: The brain imaging and clinical literatures were analyzed to identify variables that contribute to the abuse liability as well as to the clinical efficacy of methylphenidate. RESULTS: Four variables were identified. 1) Dose—there is a threshold for methylphenidate-induced dopamine increases to be perceived as reinforcing and to produce therapeutic effects. 2) Pharmacokinetics—the reinforcing effects of methylphenidate are associated with rapid changes in serum concentrations and presumably fast dopamine increases (as achieved with intravenous injection or insufflation), whereas the therapeutic effects are associated with slowly ascending serum concentrations and presumably smoothly rising dopamine levels (as achieved with oral administration). 3) Individual differences—sensitivity to methylphenidate varies across individuals and sets a threshold for blood and brain levels required for reinforcing effects (drug liking) and for therapeutic effects (symptom reduction). 4) Context—the effects of methylphenidate are modulated by different settings in abuse (rituals of self-administration and powerful conditioning) and in clinical use (external demands of low activity and focused attention). CONCLUSIONS: Reinforcing effects occur when methylphenidate elicits large and fast dopamine increases that mimic those of phasic dopamine cell firing, whereas therapeutic effects occur when methylphenidate elicits slow, steady-state dopamine increases that mimic those of tonic firing. Thus, the characteristics of clinical use (low doses administered orally and titrated for therapeutic effects) constrain methylphenidate’s abuse.
Attention deficit hyperactivity disorder (ADHD) is the most commonly diagnosed and treated behavioral disorder of childhood (1). The prevalence of ADHD is estimated to be 3%–6% of the general population in the United States and is about the same in many countries around the world when the same diagnostic criteria are used (2). Methylphenidate and amphetamine are the most frequently used treatments for ADHD (3). Over the past decade, the prescriptions for these stimulant medications have increased from less than 2 million in 1991 to over 10 million in 2001, and now it is estimated that approximately 6% of school-age children are identified and treated with these drugs (about 3 million/year in the United States).
Methylphenidate and amphetamine increase extracellular dopamine in the brain, as do cocaine and methamphetamine, the most commonly abused stimulant drugs. Methylphenidate (like cocaine) increases dopamine by blocking dopamine transporters (4), and amphetamine (like methamphetamine) increases dopamine by releasing dopamine from the terminal (5). Both increase dopamine in the nucleus accumbens, which is thought to underlie the reinforcing effects of drugs of abuse (6). This has raised legitimate concerns about the abuse liability of methylphenidate and amphetamine, although their abuse in the context of clinical use is quite limited (7) despite the magnitude of their clinical use. However, methylphenidate and amphetamine are self-administered by animals (8, 9) and sometimes used recreationally by humans (10, 11), so prevention of diversion and abuse is essential and is the rationale for methylphenidate and amphetamine being tightly controlled as Schedule II drugs.
The therapeutic effects of methylphenidate and amphetamine have also been related to their ability to increase extracellular dopamine (12, 13). Specifically, stimulant-induced dopamine increases in the striatum are believed to decrease background firing rates and increase signal-to-noise ratio of striatal cells (14), which we postulate as a mechanism for improving attention by enhancement of task-related neuronal cell firing. Since dopamine also modulates incentive salience and motivation (15), we postulate that stimulant-induced dopamine increases in the nucleus accumbens would enhance the saliency of a task by increasing the interest that it elicits and thus improving attention and performance.
Here we analyze the brain imaging and clinical literature to identify variables that influence response to methylphenidate in abuse and in clinical use. We focus on methylphenidate’s effects on dopamine, since this is the most relevant for its reinforcing effects, but we note that noradrenergic effects are also likely to be relevant for its therapeutic effects. Our analysis should also pertain to amphetamine, although the brain imaging literature is insufficient to address similarities and differences with methylphenidate.
Variable 1: Dose
Methylphenidate Doses in Clinical Use and in Abuse
The dose-response relationship of oral methylphenidate in the clinical setting has been well established (16). Up to a point, higher doses produce larger clinical responses (reductions in ADHD symptoms) but also result in increased side effects (anorexia, insomnia, stereotypic behavior, etc.). The optimal dose varies considerably across individuals (16), which will be subsequently discussed. In clinical use, the modal dose of immediate-release methylphenidate is 10 mg administered two or three times a day. For a 10-mg oral dose in a typical 30-kg child, the maximum serum concentration occurs about 1.5 to 2 hours afterward and leads to concentrations of approximately 10 ng/ml in plasma after administration, dropping by 50% about 2 hours later (17). The therapeutic effects parallel the serum concentration of immediate-release methylphenidate, with a maximum reduction in ADHD symptoms about 1.5 to 2 hours after dosing followed by a decline that is sufficient to require another dose about 4 hours after the first to reestablish full efficacy.
Abuse by oral administration of methylphenidate is rare. When abused, methylphenidate is usually administered intranasally or injected intravenously (7). The dose in abuse is not well documented, but most reports of diversion and nonclinical use suggest that 20-mg tablets of methylphenidate are ground up and sniffed. One hypothesis of the limited abuse of methylphenidate is that at clinical doses, it is a “weak stimulant” and does not produce dopamine increases sufficient to elicit reinforcing effects as those induced by the most commonly abused stimulants (cocaine and methamphetamine). This hypothesis has been addressed by studies in which positron emission tomography (PET) was used to investigate the effects of intravenous and oral methylphenidate on dopamine transporter and dopamine levels, which were conducted as part of a research program on cocaine.
Effects of Methylphenidate Compared With Cocaine
The relationships between doses of methylphenidate and of cocaine and the levels of dopamine transporter blockade were assessed in a PET study that used [11C]cocaine and [11C]methylphenidate, which themselves are radioligands whose dopamine transporter binding is decreased by pharmacological doses of methylphenidate or cocaine in proportion to the occupancy of dopamine transporter by the unlabeled drug. The relationships between dopamine transporter blockade and the reinforcing effects of cocaine and methylphenidate were assessed by using self-reports of drug effects such as “high,” “craving,” and “drug liking,” which are measures that have been shown to produce reliable and consistent findings across studies and predict administration of drugs in humans (18).
These studies revealed a threshold for drug-induced dopamine transporter blockade to be perceived as reinforcing (19, 20). For intravenous administration of cocaine or methylphenidate, greater than 50% dopamine transporter blockade was required to induce a “high” (19, 20). It is surprising that the potency of methylphenidate for blocking dopamine transporter was found to be greater than for cocaine; the ED50 dose (amount required to block 50% of dopamine transporter) for methylphenidate (0.075 mg/kg) was about half that for cocaine (0.13 mg/kg) (21). At the respective ED50 doses, reinforcing effects (self-reports of “high”) of intravenous methylphenidate were equivalent to those of intravenous cocaine. The intravenous peak plasma concentration occurs almost immediately after dosing and then drops about 50% in 2 to 3 hours (about the same as the postpeak drop after oral administration).
Of course, it is possible that oral methylphenidate at the doses used clinically would not achieve the threshold of dopamine transporter blockade considered necessary for reinforcement. The PET study to address this question revealed that oral methylphenidate at doses used therapeutically induced greater than 50% dopamine transporter blockade with an estimated ED50 dose of 0.25 mg/kg (22). A strong correlation (r=0.80, df=11, p<0.002) was seen between levels of dopamine transporter blockade and serum concentration of methylphenidate measured 2 hours after administration. On the basis of this relationship, the 50% dopamine transporter blockade “threshold” would be reached in adults at a serum concentration of about 10 ng/ml (which is expected about 2 hours after a 20-mg oral dose of immediate-release methylphenidate). In this PET study, even when higher oral doses of methylphenidate were administered that induced greater levels of dopamine transporter blockade, they were rarely perceived as reinforcing. Methylphenidate’s dopamine transporter occupancy and its relation to clinical variables as presented by Volkow et al. (22) are shown in Figure 1.
The typical intranasal doses of methylphenidate in abuse have not been well described in the literature. However, for cocaine typical doses of abuse are 0.3–0.6 mg/kg for intravenous administration and 50–100 mg for intranasal administration (23). The higher potency of methylphenidate than cocaine (21) suggests that intravenous doses of 0.1–0.3 mg/kg or intranasal doses of 25–50 mg would be used in methylphenidate abuse.
Summary
On the basis of its potency for dopamine transporter blockade, oral methylphenidate (at clinical doses used for ADHD) should not be considered a weak CNS stimulant compared with intravenous methylphenidate or even cocaine (at doses typically seen with abuse). The peak level of dopamine transporter blockade for a clinically relevant oral dose of methylphenidate, although delayed by about 2 hours, was about the same (i.e., >50%) as that seen with intravenous methylphenidate doses that produce reinforcing effects. However, these oral doses did not reliably produce the subjective experience of being “high.” This indicates that the >50% threshold for dopamine transporter blockade is necessary but not sufficient to produce reinforcing effects, so consideration of additional factors is required to understand why methylphenidate is reinforcing under some circumstances and not in others.
Variable 2: Pharmacokinetics
Route of Administration
Routes of administration affect the pharmacokinetic properties, which in turn affect the reinforcing effects of stimulant drugs. Two primary pharmacokinetic properties are relevant for relating serum concentration of methylphenidate to its therapeutic use and abuse: 1) the time to reach maximum concentration (Tmax), which is related to the absorption and distribution of the drug, and 2) the time required for the concentration to drop by 50% from the peak level (T1/2), which is related to the metabolism and excretion of the drug. Tmax (rise time) differs dramatically for intravenous and oral dosing, but T1/2 (fall time) is about the same for these two routes (17).
The time course of behavioral effects has been documented in studies addressing abuse as well as clinical use of methylphenidate. In abuse, the primary behavioral effects investigated are self-reported drug effects (i.e., the time course for the perception of being “high” as well as for craving and drug liking); in clinical use, the primary behavioral effects are the reductions of symptoms of ADHD (i.e., the time course of the decrease in hyperactivity, inattention, and impulsivity). This section discusses how the pharmacokinetic properties of stimulant drugs affect their behavioral effects.
Temporal Course of Clinical Effects
In children with ADHD, only one pharmacokinetic study comparing intravenous and oral administration of methylphenidate has been reported (17). Despite dramatic differences in Tmax (almost instantaneous for intravenous administration but about 1.5 to 2 hours for oral administration because of the delays in reaching the bloodstream imposed by absorption from the stomach and intestine), this study documented about the same T1/2 (about 2 hours) for intravenous and oral administration.
After an oral dose, the maximum behavioral effect occurs when the serum concentration reaches its maximum (near Tmax) and then declines so that when the serum concentration has dropped about 50% about 2–3 hours later (about T1/2 for methylphenidate), another dose is required to reestablish clinical efficacy. To achieve the 8–12-hour duration of efficacy desired for the clinical treatment of ADHD, dosing two or three times a day is required. For children weighing about 30 kg, a 10-mg t.i.d. regimen of immediate-release methylphenidate (about 0.3 mg/kg per administration) is expected to produce a series of peaks and troughs in plasma concentrations between 4 ng/ml (at the first trough) and 12 ng/ml (at the third peak) (Figure 2).
For children in school, dosing two or three times a day requires an administration of a controlled Schedule II drug at school. This public administration (often with children lining up at the school office at noon) is inconvenient, costly, and stigmatizing, which created a need for effective sustained-release formulations of methylphenidate that could be administered once a day. However, the first-generation sustained-release formulation, developed and approved for use over 20 years ago, was never well accepted in clinical practice, probably because the wax-matrix delivery system produced a nonoptimal pharmacokinetic profile with a much longer Tmax (about 4 hours) and only a slightly longer T1/2.
Recently, new information about the pharmacokinetic/behavioral relationship emerged from laboratory school studies that used “sipping study” methods to vary the amount of methylphenidate delivered in small doses in capsules administered every 30 minutes across the day (24, 25). These studies revealed 1) that a constant serum concentration (a “flat” pharmacokinetic profile) did not maintain full efficacy, suggesting acute tolerance to clinical doses of methylphenidate emerged each day and 2) that a rising serum concentration (an “ascending” pharmacokinetic profile) could counteract acute tolerance and maintain full efficacy for up to 12 hours.
Since 2000, several once-a-day formulations of methylphenidate and amphetamine have been developed and approved for the treatment of ADHD. These formulations are based on two processes of drug delivery: 1) an initial bolus delivery of immediate-release methylphenidate (by an overcoat or uncoated beads) designed to rapidly achieve the threshold for clinical efficacy and to produce the maximum effect within 2 hours after administration and 2) a controlled delivery of methylphenidate (by an osmotic pump process or by coated beads) designed to produce an ascending pharmacokinetic profile that would keep serum concentration above a rising threshold in order to maintain full efficacy in the face of acute tolerance (24). Studies with methylphenidate and amphetamine indicate that serum concentrations must increase about 50% from the initial morning peak to maintain full efficacy in the afternoon (Figure 2). On the basis of this design, the second generation of once-a-day formulations of methylphenidate and amphetamine have been rapidly accepted in clinical practice and now are prescribed in most (over 75%) cases for the treatment of ADHD in the United States.
Temporal Course of Reinforcing Effect
The speed of drug delivery to the brain affects the reinforcing effects of drugs (26, 27). Routes of administration that produce relatively fast brain uptake—injecting, smoking, or sniffing—are more reinforcing than oral administration, which produces relatively slow brain uptake (28).
Until recently, pharmacokinetic studies were limited to measurements in body fluids such as blood or urine. However, by using drugs labeled with carbon-11 (a positron emitter with a 20-minute half-life), which does not affect their pharmacological properties, PET imaging can be applied to directly investigate pharmacokinetic properties of [11C]cocaine and [11C]methylphenidate in the human brain and body (4). In the human brain, these drugs accumulate mostly in the striatum where they bind to dopamine transporter (4). Following intravenous dosing, uptake in the brain is very fast for both [11C]cocaine (4–6 minutes) and [11C]methylphenidate (6–10 minutes) (Figure 3), and for both drugs, the onset of the perceived “high” parallels the fast uptake of the drugs in the striatum, with the peak for the “high” reported at about the same time as the peak striatal concentration.
In contrast to these very similar and short values of Tmax, the half-life (T1/2) for cocaine and methylphenidate differed dramatically: for [11C]methylphenidate, T1/2 was much longer (90 minutes) than that seen with [11C]cocaine (20 minutes). Despite this four- to fivefold difference, the duration of the “high” was about the same for cocaine and methylphenidate (Figure 3). For cocaine, the decline of the “high” paralleled the clearance of [11C]cocaine in the striatum and returned to baseline when most of the [11C]cocaine had left the brain. For methylphenidate, however, the “high” returned to baseline even while the striatal levels of [11C]methylphenidate remained high (80% of peak). These pharmacokinetic and behavioral properties of methylphenidate derived from PET studies suggest that acute tolerance occurs to the reinforcing effects of intravenous methylphenidate, which is consistent with studies of cocaine that show that the “high” from cocaine also dissipates rapidly even when high plasma levels are maintained by repeated intravenous administration (29) or by infusion (30).
Thus, the “behavioral/reinforcing half life” of intravenous methylphenidate is much shorter than its pharmacokinetic half life (Figure 3). This dissociation suggests that the initial fast dopamine transporter blockade (and rapid increases in synaptic dopamine) is associated with the “high” and not the continuous blockade of the dopamine transporter (or consistently high levels of synaptic dopamine). Indeed, in PET studies that evaluated the relationship between methylphenidate-induced dopamine increases and their reinforcing effects, when equivalent levels of dopamine increases were established for intravenous and oral methylphenidate, intravenous methylphenidate induced a “high” but oral methylphenidate did not (13, 31). PET measures of dopamine increases were done using [11C]raclopride, a D2 receptor radioligand that competes with endogenous dopamine for D2 receptors so that its binding to the receptors is decreased when dopamine increases (32). These studies showed that with the intravenous administration of methylphenidate (dopamine measures collected 5 minutes after its administration when peak behavioral effects were observed), but not with the oral administration (dopamine measures collected at 60 minutes when peak behavioral effects were observed), the intensity of the “high” was significantly correlated with the dopamine changes (Figure 4). The behavioral differences between oral and intravenous administrations parallel the differences in the rate at which they reach peak brain concentrations (less than 10 minutes for intravenous methylphenidate and about 1.5 hours for oral methylphenidate), which are assumed to reflect the rate at which they increase dopamine (Figure 4). This would suggest that the relevant variable for reinforcement is the magnitude of the dopamine changes per time unit.
It should also be noted that even though Tmax is about the same for any dose of methylphenidate, the time at which serum concentration would cross any threshold value is related to dose, with higher doses exceeding thresholds faster than lower doses. Thus, for very large oral doses, the time required to achieve a critical level for serum concentration and dopamine transporter blockade (e.g., 50%–80%) may be similar to that for low intravenous doses, which could account for why large oral doses produce reinforcing effects in some subjects (10).
Half-Life and Clearance of the Drug From Brain
Although much less investigated, the T1/2 and clearance of stimulant drugs from the brain is also likely to affect its reinforcing effects. If a drug blocks greater than 50% of dopamine transporter with a single administration but then has slow clearance, then dopamine transporter saturation will occur with repeated frequent administration. In the case of methylphenidate, its slow clearance may also limit self-administration because of the persistence of side effects, whose duration parallels the temporal course of methylphenidate in the brain (33). We predict that drugs that block dopamine transporter but have very fast clearance, such as cocaine, are much more likely to promote frequent self-administration than drugs with relatively slow clearance such as methylphenidate (4). We also predict that fluctuating versus steady-state drug concentrations in brain will affect the drug’s reinforcing effects. This prediction is based on animal studies that show that the rate at which animals self-administer stimulant drugs is associated with the downward slope of dopamine that follows the drug-induced increases in the nucleus accumbens (34, 35). In this respect, drugs with longer half-lives or delivery systems that maintain plasma levels close to or higher than thresholds of efficacy for long time periods are less likely to be abused than drugs such as cocaine that have a very fast T1/2.
Summary
The reinforcing effects of methylphenidate are dependent on its ability to increase extracellular dopamine rapidly as when it is administered intravenously (phasic changes) but are limited by its relatively long half-life in brain. In contrast, the therapeutic effects of methylphenidate are associated with slower increases in dopamine that are maintained over time (tonic changes).
Variable 3: Individual Differences
Clinical and imaging studies have documented large individual differences in response to stimulant drugs with respect to their therapeutic as well as their reinforcing effects, which are not fully accounted for by simple factors such as age, weight, and drug metabolism. Some of these differences may be related to phenotypic differences (i.e., normal volunteers versus drug abusers versus cases with ADHD) but others appear to be due to unknown factors.
Individual Differences in Clinical Use
The optimal methylphenidate doses for the treatment of children with ADHD range from 5 mg to 20 mg per administration (a fourfold difference). Some small children require high doses and some large children require small doses, so adjustment for weight does not account for this range (36). Neither do differences in absorption and metabolism (36), since children who respond to low doses (5 mg per administration) have low serum concentrations of methylphenidate (4–5 ng/ml at Tmax) and those who respond to high doses (20 mg per administration) have high serum concentrations (12–15 ng/ml).
Individual Differences in Methylphenidate’s Effects on Dopamine
Imaging studies have documented large variability between subjects in the magnitude of the dopamine changes induced by methylphenidate (37). The hypothesis that this difference might be accounted for by differences in dopamine transporter blockade was not supported, since in some cases when methylphenidate produced >50% dopamine transporter blockade there was little or no increase in extracellular dopamine. On the basis of this finding, we postulated that the differences in the amount of methylphenidate-induced dopamine increases may reflect differences in dopamine cell activity (38), since with dopamine transporter blockade, dopamine accumulates in the extracellular space in proportion to the rate of release. This implies that methylphenidate would induce smaller dopamine changes in subjects with low dopamine cell activity than in those with high dopamine cell activity. This is consistent with the findings that HVA levels in CSF (a marker of dopamine turnover in CNS) predicts response to methylphenidate in children with ADHD: the higher the levels, the better the responses (39). It also suggests a plausible mechanism that may underlie nonresponse to methylphenidate, which occurs in 15%–30% of children with ADHD (36), or the requirement for very high doses to produce clinical effects, which is required in about 20% of those who are considered responsive to stimulants.
In the clinical use of methylphenidate, we have also suggested that individual differences in the sensitivity to the side effects of oral methylphenidate constrain the doses that can be used clinically (40). Some individuals are sensitive to methylphenidate and suffer side effects at low doses, which in addition to anorexia and insomnia often include a short period of dysphoria and stereotypic behaviors when the serum concentrations are at peak levels.
Individual Differences in the Reinforcing Effects of Methylphenidate
The reinforcing effects of stimulant drugs have been shown to vary widely across subjects (41–43). Imaging studies have consistently documented low levels of striatal dopamine D2 receptors in stimulant abusers (44), suggesting that differences in dopamine D2 receptors could underlie some of the differences in the sensitivity to the reinforcing effects of methylphenidate. To investigate this hypothesis, we measured the baseline levels of dopamine D2 receptors in the striatum of healthy non-drug-abusing subjects and in parallel assessed their sensitivity to the reinforcing effects of intravenous methylphenidate (45). Subjects with low dopamine D2 receptor levels tended to describe methylphenidate as pleasant, whereas the subjects with high dopamine D2 receptor levels tended to describe it as unpleasant. In addition, dopamine D2 receptor levels correlated negatively with methylphenidate-induced pleasant effects (subject self-ratings of happiness and mood) and positively with its unpleasant effects (subject self-ratings of annoyance and distrust). Another study documented that the levels of dopamine D2 receptors predicted how much subjects liked the effects of intravenous methylphenidate (46). These findings suggest that vulnerability to stimulant abuse may be related in part to the expression of dopamine D2 receptors: subjects with low levels of dopamine D2 receptors may be at higher risk of abusing stimulant drugs than those with high levels of dopamine D2 receptors, in whom drugs like methylphenidate may produce unpleasant effects that limit its abuse.
Summary
Pharmacokinetic/behavioral studies document large individual differences in sensitivity to oral doses of methylphenidate that appear to depend mostly on central rather than peripheral factors. PET studies in humans provide evidence that the variability in methylphenidate-induced increases in dopamine are likely to reflect differences in dopamine cell activity (dopamine release) between subjects. This suggests a mechanism for the wide range of clinical doses. It also corroborates the findings from animal studies showing that responses to stimulants are determined in part by the state of the dopamine system (47, 48). Imaging studies have also shown that the availability of dopamine D2 receptors in the brain may modulate the reinforcing responses to methylphenidate in humans.
Variable 4: Context of Administration
If the effects of methylphenidate are a result of dopamine signal amplification and dependent in part on dopamine cell activity, which itself is responsive to environmental stimulation (49), then one could predict that these effects should be sensitive to the context of administration and to expectations, which differ dramatically in abuse and clinical use.
Context Effects in Clinical Use
In clinical practice, the context of the school setting moderates the impact of stimulant medications on children with ADHD. The initial studies of context effects were with amphetamine, but recently situational effects have also been corroborated for methylphenidate. One study showed that children with ADHD treated with methylphenidate showed larger reductions in placebo-adjusted activity level in the classroom than in the playground setting (50).
In clinical studies of methylphenidate, the traditional “placebo effects” do not occur. Instead, after placebo administration, a clear pattern of deterioration across the day emerges, in contrast to the pattern of improvement with methylphenidate (50). Also, when methylphenidate is given therapeutically and produces large improvements in the classroom, children with ADHD do not attribute this “success” to the drug (51). This indicates that expectancy does not play a prominent role in methylphenidate’s therapeutic effects.
Context Effects in Abuse
It is recognized that context as well as expectation affects the responses to drugs of abuse (52). For example, the subjective responses of drug abusers to the drug are more pleasurable when subjects expect to receive the drug than when they do not (53). This effect is believed to be due in part to conditioned associative learning, which enables previously “neutral” stimuli to elicit appetitive responses (54). Chronic drug use, which markedly stimulates dopamine neurotransmission, results in attribution of excessive salience to drug taking and to drug-associated stimuli (54).
The context dependency of stimulant-induced dopamine increases has been demonstrated in laboratory animals for cocaine. For example, cocaine-induced increases in dopamine in the nucleus accumbens are larger when animals are given cocaine in an environment where they had previously received cocaine than when they receive it in a novel environment (55) or when animals self-administer cocaine than when cocaine administration is involuntary (56). Microdialysis studies in rodents have shown that the magnitude of methylphenidate-induced dopamine increases in the prefrontal cortex is dependent on the conditions of its administration: when rats are restrained for 15 minutes at the time of administration, methylphenidate-induced increases in dopamine are significantly greater than when they are not (57).
There is also evidence that methylphenidate-induced changes in dopamine in the human brain are affected by context. In PET studies of humans, increases in extracellular dopamine in the striatum after 20 mg of oral methylphenidate were greater when subjects were exposed to a salient stimulus (visual display of food in food-deprived individuals) than when it was given with a neutral stimulus (recall of family genealogy) (58).
Summary
We postulate that dopamine cell activity depends on context and conditioning, which can amplify or dampen dopamine increases at any level of dopamine transporter blockade. This could provide an explanation for some qualitative differences in the effects of methylphenidate in abuse and in clinical use. In both settings, we postulate that context will have a large effect on response to methylphenidate but that the context of clinical use and abuse differ qualitatively. Moreover, conditioning may operate in abuse and not in clinical use, where clear and large effects of methylphenidate are not attributed to the drug. Thus, within the context of the classroom, methylphenidate appears to make schoolwork more salient but does not elicit drug craving or drug-seeking behavior to recreate this effect, but when it is procured illegally and taken with the expectation of getting “high,” powerful conditioning factors appear to operate that do elicit drug craving and drug seeking.
Discussion
The literature indicates that the level and variation in dopamine is set by two processes: tonic dopamine cell firing (which maintains baseline steady-state extrasynaptic dopamine levels and sets the overall responsiveness of the dopamine system) and phasic dopamine cell firing (which leads to fast dopamine changes that highlight the saliency of stimuli) (59). Our analysis of the literature suggests that methylphenidate-induced dopamine changes per time unit is the primary factor that distinguishes the reinforcing effects from the therapeutic effects. On this basis, we speculate that methylphenidate’s ability to induce fast increases in dopamine that mimic those produced by phasic dopamine cell firing is associated with abuse, whereas methylphenidate’s ability to induce slow, steady-state increases in dopamine that mimic those produced by tonic dopamine cell firing is associated with clinical use. Although it had been hypothesized that the therapeutic effects of methylphenidate are due to its ability to increase tonic dopamine levels, which then stimulate dopamine autoreceptors attenuating phasic dopamine increases (60), we postulate that methylphenidate’s long-lasting dopamine transporter blockade (main mechanism for removal of extracellular dopamine) results in an overall amplification of dopamine signals. Indeed, imaging studies document an amplification of stimulation-induced dopamine increases by oral methylphenidate (58).
We postulate that individual differences exist in release (dopamine cell firing) and receptor sensitivity, which modulate the impact of methylphenidate (an indirect agonist that depends on release), and that these factors affect the vulnerability to or interfere with abuse. Also context and expectation modulate methylphenidate’s effects differently in abuse (where strong conditioned responses enhance its reinforcing effects and trigger its use) than in clinical use (where rigorous timed dosing in the context of daily routines constrains its abuse).
We hypothesize that under certain circumstances methylphenidate overactivates the dopamine system, making the experience of the drug itself “very salient” (by intravenous or very large oral doses that produce fast and large increases in dopamine). Moreover, by exceeding the usual threshold for salience, this can operate to decrease the salience of non-drug-related stimuli. In contrast, methylphenidate at therapeutic doses will operate to amplify the saliency value of stimuli to which the subject may be exposed during everyday routines and which by themselves may have been insufficient to elicit dopamine responses that signal saliency and drive interest and attention.
Received Jan. 22, 2003; revision received March 19, 2003; accepted March 31, 2003. From the Brookhaven National Laboratory; the Department of Psychiatry, State University of New York, Stony Brook; and the Child Development Center, University of California, Irvine. Address reprint requests to Dr. Volkow, National Institute on Drug Abuse, 6001 Executive Blvd., Room 5274–MSC 9581, Bethesda, MD 20892; [email protected] (e-mail). Supported in part by grants from the Department of Energy, Office of Biological and Environmental Research (DE-ACO2-98CH10886); and the National Institute on Drug Abuse (DA-7092-01 and DA-00280).
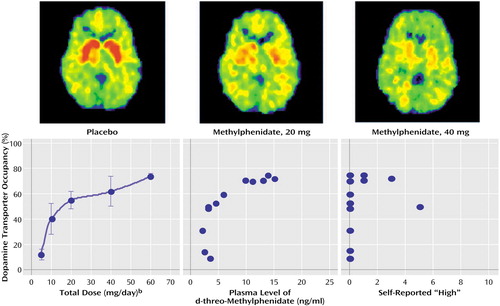
Figure 1. Dopamine Transporter Occupancy Following Administration of Placebo or Therapeutic Doses of Oral Methylphenidate and Relation to Clinical Variablesa
aAdapted from Volkow et al. (22): the images in the top row show reductions in striatal binding of the [11C]cocaine ligand with methylphenidate relative to placebo. The lower panel shows the relationship between dopamine transporter blockade induced by oral methylphenidate and clinical variables. Note that while oral methylphenidate induced greater than 50% dopamine transporter blockade, it did not induce a “high.”
bError bars represent standard deviations.
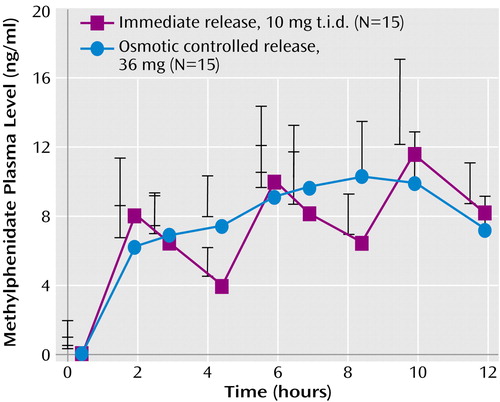
Figure 2. Drug Plasma Concentrations Across the Day in Children With ADHD, by Methylphenidate Release Formulationa
aData are from study by Swanson et al. (24). Mean values are presented with standard deviations depicted as error bars. Immediate-release methylphenidate, given three times a day at about 0.3 mg/Kg to a typical 10-year-old child, elicits peaks and troughs in plasma concentrations between 4 ng/ml (at the first trough) and 12 ng/ml (at the third peak), whereas the sustained osmotic-controlled release elicits a smooth-rising plasma concentration of methylphenidate.
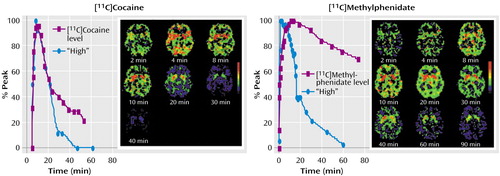
Figure 3. Striatal Uptake and Self-Reports of Being “High” in Cocaine-Abusing Subjects After Intravenous Administration of Cocaine or Methylphenidatea
aAdapted from Volkow et al. (4): subjects were given pharmacological doses of cocaine (0.6 mg/kg) or methylphenidate (0.5 mg/kg). The graphs show the time activity curves for the concentration of the ligands [11C]cocaine and [11C]methylphenidate in the striatum alongside the temporal course for subject self-reports of being “high.”
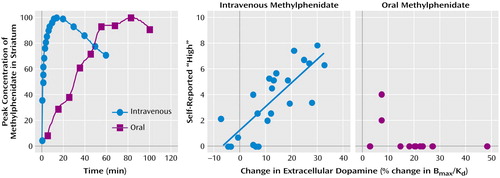
Figure 4. Striatal Uptake and the Relationship Between Changes in Extracellular Dopamine and Self-Reports of Being “High” After Intravenous or Oral Administration of Methylphenidatea
aData in the first panel, adapted from Solanto (12), are from a baboon, since mouth exposure to radiation from oral doses of labeled methylphenidate is too high for human studies. The second and third panels are adapted from Volkow et al. (13, 31, 32, 44): subject self-reports were obtained 5 minutes after intravenous administration and 60 minutes after oral administration. Note that while oral and intravenous methylphenidate induced equivalent changes in dopamine, oral methylphenidate did not induce a “high,” whereas for intravenous methylphenidate the magnitude of the dopamine increases was associated with the intensity of the “high.” This is likely to reflect differences in the rate at which dopamine changes occur, which was much faster with intravenous administration (peak achieved after 6-10 minutes) than with oral administration (peak achieved after 60–90 minutes) of methylphenidate.
1. National Institutes of Health: Consensus development conference statement: diagnosis and treatment of attention-deficit/hyperactivity disorder (ADHD). J Am Acad Child Adolesc Psychiatry 2000; 39:182–193Crossref, Medline, Google Scholar
2. Swanson JM, Sergeant JA, Taylor E, Sonuga-Barke EJS, Jensen PS, Cantwell DP: Attention deficit disorder and hyperkinetic disorder. Lancet 1998; 351:429–433Crossref, Medline, Google Scholar
3. Greenhill LL, Pliszka S, Dulcan MK, Bernet W, Arnold V, Beitchman J, Benson RS, Bukstein O, Kinlan J, McClellan J, Rue D, Shaw JA, Stock S (American Academy of Child and Adolescent Psychiatry): Practice parameter for the use of stimulant medications in the treatment of children, adolescents, and adults. J Am Acad Child Adolesc Psychiatry 2002; 41(Feb suppl):26S-49SGoogle Scholar
4. Volkow ND, Ding Y, Fowler JS, Wang GJ, Logan J, Gatley JS, Dewey SL, Ashby C, Lieberman J, Hitzemann R, Wolf AP: Is methylphenidate like cocaine? studies on their pharmacokinetics and distribution in human brain. Arch Gen Psychiatry 1995; 52:456–463Crossref, Medline, Google Scholar
5. Jones SR, Gainetdinov RR, Wightman RM, Caron MG: Mechanisms of amphetamine action revealed in mice lacking the dopamine transporter. J Neurosci 1998; 18:1979–1986Crossref, Medline, Google Scholar
6. Di Chiara GD, Imperato A: Drugs abused by humans preferentially increase synaptic dopamine concentrations in the mesolimbic system of freely moving rats. Proc Natl Acad Sci USA 1988; 85:5274–5278Crossref, Medline, Google Scholar
7. Parran TV, Jasinski DR: Intravenous methylphenidate abuse: prototype for prescription drug abuse. Arch Intern Med 1991; 151:781–783Crossref, Medline, Google Scholar
8. Johanson CE, Shuster CR: A choice procedure for drug reinforcers: cocaine and methylphenidate in the rhesus monkey. J Pharmacol Exp Ther 1975; 193:676–688Medline, Google Scholar
9. Bergman J, Madras B, Johnson SE, Spealman RD: Effects of cocaine and related drugs in nonhuman primates, III: self-administration by squirrel monkeys. J Pharmacol Exp Ther 1989; 251:150–155Medline, Google Scholar
10. Kollins SH, MacDonald EK, Rush CR: Assessing the abuse potential of methylphenidate in nonhuman and human subjects: a review. Pharmacol Biochem Behav 2001; 68:611–627Crossref, Medline, Google Scholar
11. Foley R, Mrvos R, Krenzelok EP: A profile of methylphenidate exposures. J Toxicol Clin Toxicol 2000; 38:625–630Crossref, Medline, Google Scholar
12. Solanto MV: Neuropsychopharmacological mechanisms of stimulant drug action in attention-deficit hyperactivity disorder: a review and integration. Behav Brain Res 1998; 94:127–152Crossref, Medline, Google Scholar
13. Volkow ND, Wang G, Fowler JS, Logan J, Gerasimov M, Maynard L, Ding Y, Gatley SJ, Gifford A, Franceschi D: Therapeutic doses of oral methylphenidate significantly increase extracellular dopamine in the human brain. J Neurosci 2001; 21:RC121:1–5Google Scholar
14. Kiyatkin EA, Rebec GV: Dopaminergic modulation of glutamate-induced excitations of neurons in the neostriatum and nucleus accumbens of awake, unrestrained rats. J Neurophysiol 1996; 75:142–153Crossref, Medline, Google Scholar
15. Berridge KC, Robinson TE: What is the role of dopamine in reward: hedonic impact, reward learning, or incentive salience? Brain Res Rev 1997; 28:309–369Crossref, Google Scholar
16. Greenhill LL, Swanson JM, Vitiello B, Davies M, Clevenger W, Wu M, Arnold LE, Abikoff HB, Bukstein OG, Conners CK, Elliott GR, Hechtman L, Hinshaw SP, Hoza B, Jensen PS, Kraemer HC, March JS, Newcorn JH, Severe JB, Wells K, Wigal T: Impairment and deportment responses to different methylphenidate doses in children with ADHD: the MTA titration trial. J Am Acad Child Adolesc Psychiatry 2001; 40:180–187Crossref, Medline, Google Scholar
17. Chan YP, Swanson JM, Soldin SS, Thiessen JJ, Macleod SM, Logan W: Methylphenidate hydrochloride given with or before breakfast, II: effects on plasma concentration of methylphenidate and ritalinic acid. Pediatrics 1983; 72:56–59Medline, Google Scholar
18. Fischman MW, Foltin RW: Utility of subjective-effects measurements in assessing abuse liability of drugs in humans. Br J Addict 1991; 86:1563–1570Crossref, Medline, Google Scholar
19. Volkow ND, Wang GJ, Fischman MW, Foltin RW, Fowler JS, Abumrad NN, Vitkun S, Logan J, Gatley SJ, Pappas N, Hitzemann R, Shea CE: Relationship between subjective effects of cocaine and dopamine transporter occupancy. Nature 1997; 386:827–830Crossref, Medline, Google Scholar
20. Volkow ND, Wang G-J, Fowler JS, Gatley SJ, Logan J, Ding Y-S, Dewey SL, Hitzemann R, Gifford A, Pappas NR: Blockade of striatal dopamine transporters by intravenous methylphenidate is not sufficient to induce self reports of “high.” J Pharmacol Exp Ther 1999; 288:14–20Medline, Google Scholar
21. Volkow ND, Wang GJ, Fowler JS, Fischman M, Foltin R, Gatley SJ, Logan J, Wong C, Gifford A, Hitzemann R, Pappas N: Methylphenidate and cocaine have a similar in vivo potency to block dopamine transporters in the human brain. Life Sci 1999; 65:7–12Crossref, Google Scholar
22. Volkow ND, Wang G-J, Fowler JS, Gatley SJ, Logan J, Ding Y-S, Hitzemann R, Pappas N: Dopamine transporter occupancies in the human brain induced by therapeutic doses of oral methylphenidate. Am J Psychiatry 1998; 155:1325–1331Link, Google Scholar
23. Foltin RW, Fischman MW: Smoked and intravenous cocaine in humans: acute tolerance, cardiovascular and subjective effects. J Pharmacol Exp Ther 1991; 257:247–261Medline, Google Scholar
24. Swanson J, Gupta S, Lam A, Shoulson I, Lerner M, Modi N, Lindemulder E, Wigal S: Development of a new once-a-day formulation of methylphenidate for the treatment of attention-deficit/hyperactivity disorder: proof-of-concept and proof-of-product studies. Arch Gen Psychiatry 2003; 60:204–211Crossref, Medline, Google Scholar
25. Swanson J, Gupta S, Guinta D, Flynn D, Agler D, Lerner M, Williams L, Shoulson I, Wigal S: Acute tolerance to methylphenidate in the treatment of attention deficit hyperactivity disorder in children. Clin Pharmacol Ther 1999; 66:295–305Crossref, Medline, Google Scholar
26. Oldendorf WH: Some relationships between addiction and drug delivery to the brain, in Bioavailability of Drugs to the Brain and the Blood Brain Barrier: NIDA Research Monograph 120. Edited by Frankenheim J, Brown RM. Rockville, Md, National Institute on Drug Abuse, 1992, pp 13–25Google Scholar
27. Balster RL, Schuster CR: Fixed-interval schedule of cocaine reinforcement: effects of dose and infusion duration. J Exp Anal Behav 1973; 20:119–129Crossref, Medline, Google Scholar
28. Verebey K, Gold MS: From coca leaves to crack: the effects of dose and routes of administration in abuse liability. Psychiatr Annals 1988; 18:513–520Crossref, Google Scholar
29. Foltin RW, Fischman M: Smoked and intravenous cocaine in humans: acute tolerance, cardiovascular and subjective effects. J Pharmacol Exp Ther 1991; 257:247–261Medline, Google Scholar
30. Ambre JJ, Belknap SM, Nelson J, Ruo TI, Shin SG, Atkinson AJ: Acute tolerance to cocaine in humans. Clin Pharmacol Ther 1988; 44:1–8Crossref, Medline, Google Scholar
31. Volkow ND, Wang GJ, Fowler JS, Logan J, Gatley SJ, Wong C, Hitzemann R, Pappas NR: Reinforcing effects of psychostimulants in humans are associated with increases in brain dopamine and occupancy of D(2) receptors. J Pharmacol Exp Ther 1999; 291:409–415Medline, Google Scholar
32. Volkow ND, Wang G-J, Fowler JS, Logan J, Schlyer D, Hitzemann R, Lieberman J, Angrist B, Pappas N, MacGregor R, Burr G, Cooper T, Wolf AP: Imaging endogenous dopamine competition with [11C]raclopride in the human brain. Synapse 1994; 16:255–262Crossref, Medline, Google Scholar
33. Volkow ND, Wang GJ, Gatley SJ, Fowler JS, Ding YS, Logan J, Hitzemann R, Angrist B, Lieberman J: Temporal relationships between the pharmacokinetics of methylphenidate in the human brain and its behavioral and cardiovascular effects. Psychopharmacology (Berl) 1996; 123:26–33Crossref, Medline, Google Scholar
34. Wise RA, Newton P, Leeb K, Burnette B, Pocock D, Justice JB Jr: Fluctuations in nucleus accumbens dopamine concentration during intravenous cocaine self-administration in rats. Psychopharmacology (Berl) 1995; 120:10–20Crossref, Medline, Google Scholar
35. Ranaldi R, Pocock D, Zereik R, Wise RA: Dopamine fluctuations in the nucleus accumbens during maintenance, extinction, and reinstatement of intravenous D-amphetamine self-administration. J Neurosci 1999; 19:4102–4109Crossref, Medline, Google Scholar
36. Swanson JM, Cantwell D, Lerner M, McBurnett K, Hanna G: Effects of stimulant medication on learning in children with ADHD. J Learn Disabil 1991; 24:219–230Crossref, Medline, Google Scholar
37. Volkow ND, Wang GJ, Fowler JS, Logan J, Franceschi D, Maynard L, Ding YS, Gatley SJ, Gifford W, Swanson JM: Relationship between blockade of dopamine transporters by oral methylphenidate and the increases in extracellular dopamine: therapeutic implications. Synapse 2002; 43:181–187Crossref, Medline, Google Scholar
38. Pucak ML, Grace AA: Regulation of substantia nigra dopamine neurons. Crit Rev Neurobiol 1994; 9:67–89Medline, Google Scholar
39. Castellanos FX, Elia J, Kruesi MJ, Marsh WL, Gulotta CS, Potter WZ, Ritchie GF, Hamburger SD, Rapoport JL: Cerebrospinal fluid homovanillic acid predicts behavioral response to stimulants in 45 boys with attention deficit/hyperactivity disorder. Neuropsychopharmacology 1996; 14:125–137Crossref, Medline, Google Scholar
40. Swanson J, Volkow ND: Pharmacokinetic and pharmacodynamic properties of methylphenidate in humans, in Stimulant Drugs and ADHD. Edited by Solanto MV, Arnsten AFT, Castellanos FX. New York, Oxford University Press, 2001, pp 259–282Google Scholar
41. Chait LD: Factors influencing the reinforcing and subjective effects of d-amphetamine in humans. Behav Pharmacol 1993; 4:191–199Crossref, Medline, Google Scholar
42. Slattum PW, Venitz J, Barr WH: Comparison of methods for the assessment of central nervous system stimulant response after dextroamphetamine administration to healthy male volunteers. J Clin Pharmacol 1996; 36:1039–1050Crossref, Medline, Google Scholar
43. Wang G-J, Volkow ND, Hitzemann RJ, Wong C, Angrist B, Burr G, Pascani K, Pappas N, Lu A, Cooper T, Lieberman JA: Behavioral and cardiovascular effects of intravenous methylphenidate in normal subjects and cocaine abusers. Eur Addict Res 1997; 3:49–54Crossref, Google Scholar
44. Volkow ND, Fowler JS, Wang GJ: Role of dopamine in drug reinforcement and addiction in humans: results from imaging studies. Behav Pharmacol 2002; 13:355–366Crossref, Medline, Google Scholar
45. Volkow ND, Wang G-J, Fowler JS, Logan J, Gatley SJ, Gifford A, Hitzemann R, Ding Y-S, Pappas N: Prediction of reinforcing responses to psychostimulants in humans by brain dopamine D2 receptor levels. Am J Psychiatry 1999; 156:1440–1443Link, Google Scholar
46. Volkow ND, Wang G-J, Fowler JS, Thanos PP, Logan J, Gatley SJ, Gifford A, Ding Y-S, Wong C, Pappas N, Thanos PPK: Brain DA D2 receptors predict reinforcing effects of stimulants in humans: replication study. Synapse 2002; 46:79–82; correction, 2003; 47:295Google Scholar
47. Deminiere IM, Piazza PV, Le Moal M, Simon H: Experimental approach to individual vulnerability to psychostimulant addiction. Neurosci Biobehav Rev 1989; 13:141–147Crossref, Medline, Google Scholar
48. Hooks MS, Jones GH, Smith AD, Neill DB, Justice JB: Response to novelty predicts the locomotor and nucleus accumbens dopamine response to cocaine. Synapse 1991; 9:121–128Crossref, Medline, Google Scholar
49. Overton PG, Clark D: Burst firing in midbrain dopaminergic neurons. Brain Res Brain Res Rev 1997; 25:312–334Crossref, Medline, Google Scholar
50. Swanson JM, Gupta S, Williams L, Agler D, Lerner M, Wigal S: Efficacy of a new pattern of delivery of methylphenidate for the treatment of ADHD: effects on activity level in the classroom and on the playground. J Am Acad Child Adolesc Psychiatry 2002; 41:1306–1314Crossref, Medline, Google Scholar
51. Pelham WE, Hoza B, Kipp HL, Gnagy EM, Trane ST: Effects of methylphenidate and expectancy of ADHD children’s performance, self-evaluations, persistence, and attributions on a cognitive task. Exp Clin Psychopharmacol 1997; 5:3–13Crossref, Medline, Google Scholar
52. Mitchell SH, Laurent CL, de Wit H: Interaction of expectancy and the pharmacological effects of d-amphetamine: subjective effects and self-administration. Psychopharmacology (Berl) 1996; 125:371–378Crossref, Medline, Google Scholar
53. Kirk JM, Doty P, De Wit H: Effects of expectancies on subjective responses to oral delta9-tetrahydrocannabinol. Pharmacol Biochem Behav 1998; 59:287–293Crossref, Medline, Google Scholar
54. Robinson TE, Berridge KC: The neural basis of drug craving: an incentive-sensitization theory of addiction. Brain Res Brain Res Rev 1993; 18:247–291Crossref, Medline, Google Scholar
55. Duvauchelle CL, Ikegami A, Asami S, Robens J, Kressin K, Castaneda E: Effects of cocaine context on NAcc dopamine and behavioral activity after repeated intravenous cocaine administration. Brain Res 2000; 862:49–58Crossref, Medline, Google Scholar
56. Hemby SE, Co C, Koves TR, Smith JE, Dworkin SI: Differences in extracellular dopamine concentrations in the nucleus accumbens during response-dependent and response-independent cocaine administration in the rat. Psychopharmacology (Berl) 1997; 133:7–16Crossref, Medline, Google Scholar
57. Marsteller DA, Gerasimov MR, Schiffer WK, Geiger JM, Barnett CR, Borg JS, Scott S, Ceccarelli J, Volkow ND, Molina PE, Alexoff DL, Dewey SL: Acute handling stress modulates methylphenidate-induced catecholamine overflow in the medial prefrontal cortex. Neuropsychopharmacology 2002; 27:163–170Crossref, Medline, Google Scholar
58. Volkow ND, Wang G-J, Fowler JS, Logan J, Jayne B, Franceschi D, Wong C, Gatley SJ, Gifford A, Ding Y-S, Pappa N: “Non-hedonic” food motivation in humans involves dopamine in the dorsal striatum. Synapse 2002; 44:175–180Crossref, Medline, Google Scholar
59. Grace AA: The tonic/phasic model of dopamine system regulation and its implications for understanding alcohol and psychostimulant craving. Addiction 2000; 95:S119-S128Google Scholar
60. Seeman P, Madras BK: Anti-hyperactivity medication: methylphenidate and amphetamine. Mol Psychiatry 1998; 3:386–396Crossref, Medline, Google Scholar



