Treatment of Borderline Personality Disorder With Psychoanalytically Oriented Partial Hospitalization: An 18-Month Follow-Up
Abstract
OBJECTIVE: The aim of this study was to determine whether the substantial gains made by patients with borderline personality disorder following completion of a psychoanalytically oriented partial hospitalization program, in comparison to patients treated with standard psychiatric care, were maintained over an 18-month follow-up period. METHOD: Forty-four patients who participated in the original study were assessed every 3 months after completion of the treatment phase. Outcome measures included frequency of suicide attempts and acts of self-harm, number and duration of inpatient admissions, service utilization, and self-reported measures of depression, anxiety, general symptom distress, interpersonal functioning, and social adjustment. RESULTS: Patients who completed the partial hospitalization program not only maintained their substantial gains but also showed a statistically significant continued improvement on most measures in contrast to the patients treated with standard psychiatric care, who showed only limited change during the same period. CONCLUSIONS: The superiority of psychoanalytically oriented partial hospitalization over standard psychiatric treatment found in a previous randomized, controlled trial was maintained over an 18-month follow-up period. Continued improvement in social and interpersonal functioning suggests that longer-term changes were stimulated.
Previously, we reported a favorable treatment outcome for patients with borderline personality disorder who completed a psychoanalytically oriented partial hospitalization program (1). Forty-four patients either were assigned to the partial hospitalization program or received standard psychiatric care (control group) in a randomized, controlled design. Treatment, which included individual and group psychoanalytic psychotherapy, was for a maximum of 18 months. Patients who completed the partial hospitalization program showed a favorable response on symptomatic and clinical measures when compared with the treatment-as-usual control group. But the chronically cyclic nature of borderline personality disorder means that long-term follow-up is essential. This article describes an 18-month follow-up of subjects who participated in the original study and includes three subjects who had terminated treatment prematurely.
There are limited follow-up data for psychotherapeutic treatments of patients with borderline personality disorder. Most studies either follow up patients retrospectively or follow a cohort of patients prospectively but without a controlled comparison group (2). Over a period of 1 year, Stevenson and Meares (3) successfully treated patients with borderline personality disorder with psychoanalytic psychotherapy. At a 5-year follow-up evaluation, the gains were maintained (4). But the study was uncontrolled, which limits the conclusions that can be drawn. In a controlled study, Linehan et al. (5) evaluated patients successfully treated with dialectical behavior therapy after 1 year and found few between-group differences, although some measures continued to favor dialectical behavior therapy. The present follow-up study has a number of advantages. The original study was an effectiveness trial of ordinary clinical referrals with a control group, had few exclusion criteria, and had a low dropout rate. Follow-up data from centrally organized medical records were available concerning self-harm, suicide attempts, and inpatient episodes on all patients. Loss of information from incomplete self-report data was small.
Individual and group psychoanalytic psychotherapy in the partial hospitalization program specifically targeted the development of mental capacities expected to enhance an individual’s resilience to psychosocial stress over the long term (6). In the context of follow-up for borderline personality disorder treatment, this enhancement is likely to be indicated not only by continuing symptomatic relief, reduction in suicide attempts and acts of self harm, and maintenance of gains in interpersonal functioning and social adjustment but also by further improvement. There is accumulating evidence that psychodynamic treatments are associated with continued improvement during the follow-up period (7). Thus, the present study had two main objectives: 1) to determine if the gains seen following the partial hospitalization program relative to those seen with treatment as usual were maintained and 2) to establish whether additional improvement occurred.
Method
Of 44 patients in the original study, three patients had left the partial hospitalization program prematurely (after 1 month, 2 months, and 4 months), and an additional three patients crossed over to the partial hospitalization program from the control group within 1 month of treatment assignment. The previous report analyzed data from the 38 patients (19 in each group) who remained in the group to which they had been assigned up to the end of the 18-month treatment period. This follow-up study reports on all patients assigned to the partial hospitalization program regardless of treatment duration (i.e., dropouts were included) and therefore represents a more conservative approach. Written informed consent was obtained after the procedure had been fully explained. An attempt was made at 18 months following admission to follow all 44 patients for an additional 18 months. No patient in the partial hospitalization program was lost to follow-up, but some refused to complete all assessments at all time points. Three patients in the control group refused continued participation. Complete medical records were, however, available for these patients. While assessments were not blind, all the outcome variables were based on objective clinical records confirmed by independent evaluation or were self-report measures.
Subject characteristics, the trial methodology, and details about the treatment program and the quality of randomization were presented in our original report (1). The two groups did not significantly differ on any demographic or clinical characteristic or on any of the outcome variables with the exception of a slightly higher state anxiety score and a lower social adjustment score for patients assigned to the partial hospitalization program. Outcome measures were assessed with the same instruments as during the treatment phase of the study. The SCL-90-R (8) was administered three times during the follow-up period (at the 24-, 30-, and 36-month evaluations) to assess self-reported general psychiatric symptoms. The Beck Depression Inventory (9) and Spielberger State and Trait Inventory (10) were administered five times during the follow-up period (at the 21-, 24-, 27-, 30-, and 36-month evaluations) to monitor depression and anxiety, respectively. Social and interpersonal functioning were measured with the Social Adjustment Scale (11) and the Inventory of Interpersonal Problems—circumflex version (12), respectively, at the end of the treatment phase (month 18) and the end of the follow-up period (month 36). Only 5% of the data for the patients in the partial hospitalization program (including dropouts) and less than 25% of the control group data were lost because of incomplete measures.
A semistructured interview (Suicide and Self-Harm Inventory) was used to obtain details of both suicidal and self-damaging acts at the 24-, 30-, and 36-month evaluations. Details of the method of collection of this information can be found in our original study (1). For all patients, searches of the hospital inpatient database were made at the 24-, 30-, and 36-month evaluations to obtain the number of hospital admissions and the lengths of stay over the preceding 6 months. These were cross-checked with the medical notes. All patients were admitted to the local unit because of the contracted nature of the service.
It was not possible to prevent patients from having further treatment. Participation in other treatment programs was monitored throughout the study for all patients, including medication data ascertained from prescription charts and dispensing records. A follow-up program was offered to the patients assigned to the partial hospitalization program, which was attended by all except the three who prematurely terminated treatment. The program consisted of group analytic therapy twice a week (180 hours over 18 months) and review in a psychiatric outpatient clinic if requested every 3 months (conducted by A.B.). Group attendance was 75% during the follow-up period, which indicates the stability of this cohort of treated patients. Community center attendance and general psychiatric partial hospitalization programs were available through self-referral. The control group continued to receive general psychiatric treatment, which could involve inpatient admission when required, a general psychiatric partial hospitalization program, outpatient consultation, community center attendance, or medication. None received any formal psychotherapy, although this was not precluded during the follow-up period.
All analyses were carried out using SPSS for Windows (Version 8, Chicago). We applied the multivariate analog of the analysis of covariance (ANCOVA) model to all interval data, including all self-report variables, with pretreatment scores as covariates and the time points of follow-up assessments as repeated measures variables (time). We predicted a significant main effect of treatment group (group), which is a test for continued treatment effectiveness. If there were trends toward relapse in the patients who completed the partial hospitalization program or remission in the control group patients during the follow-up period, we would expect significant interactions between the group and time factors. We used pair-wise comparisons with Bonferroni corrections to test if mean differences were significant at each of the follow-up assessment points. When the assumptions of the general-linear model were not met, nonparametric (Mann-Whitney U) tests were performed to test the difference between groups at each follow-up assessment, and a test of differences (Friedman’s test) was performed separately for each group to assess if there was evidence for significant tendency for relapse or remission. In the case of binary variables, Fisher’s exact test was used to compare groups, and these are reported as bare probabilities. All statistical analyses were repeated after including the subjects who had crossed over to the partial hospitalization program (i.e., N=25 versus 19) as well as after excluding dropouts (i.e., N=19 versus 19). These analyses led to an almost identical pattern of findings.
Results
Acts of Self-Harm and Suicide Attempts
At the end of the treatment phase, significantly more borderline personality disorder patients who completed the partial hospitalization program (N=13) than control group patients (N=3) had refrained from self-mutilation in the preceding 6 months (p<0.005, Fisher’s exact test). In addition, significantly more partial hospitalization patients than control group patients reported not engaging in self-mutilation after 24 months (90.9% [N=20 of 22] versus 36.8% [N=7 of 19], respectively; p<0.001, Fisher’s exact test), 30 months (81.8 % [N=18] versus 31.6% [N=6]; p<0.001, Fisher’s exact test) and 36 months (77.3% [N=17] versus 31.6% [N=6]; p<0.004, Fisher’s exact test). More self-mutilating acts were committed during the 18-month follow-up period by patients in the control group (mean=10.9, SD=11.8) than by patients who completed the partial hospitalization program (mean=0.6, SD=1.6), a difference that was highly significant (Mann-Whitney U=84, p<0.001).
A similar pattern emerged for suicide attempts. At the end of treatment, significantly fewer patients who completed the partial hospitalization program (N=4) than control group patients (N=12) had attempted suicide in the preceding 6 months (p<0.004, Fisher’s exact test). In addition, significantly fewer partial hospitalization patients than control group patients had made a serious suicidal gesture after 24 months (9.1% [N=2] versus 36.8% [N=7], respectively; p<0.04, Fisher’s exact test) and 36 months (18.2% [N=4] versus 63.2% [N=12]; p<0.004, Fisher’s exact test). Fewer suicide attempts were made during the 18-month follow-up period by patients who completed the partial hospitalization program (N=4) than by patients in the control group (N=28), a difference that was again highly significant (Mann-Whitney U=97, p<0.001).
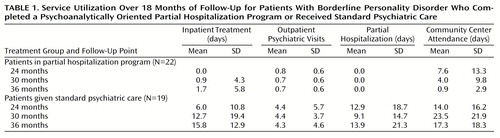
Service Utilization
Service utilization data are summarized in Table 1. No patient who completed the partial hospitalization program had been admitted by 6 months after discharge, whereas seven patients who had received standard psychiatric care had been admitted at least once by the 24-month evaluation (p<0.002, Fisher’s exact test). By 1 year after the end of the treatment phase, one partial hospitalization patient had been admitted for 20 days, while seven more control group patients received inpatient treatment (p<0.02, Fisher’s exact test). An additional partial hospitalization patient was admitted twice in the final 6 months of follow-up for 25 and 12 days, while 14 control group patients were admitted during the final 6 months (p<0.001, Fisher’s exact test). Mann-Whitney tests revealed that differences in the average number of inpatient treatment days between the two groups were significant at all follow-up points (24 months: U=143, p<0.005; 30 months: U=138, p<0.007; 36 months: U=72, p<0.001). We examined the variation over the 18 months of follow-up in the number of days in the hospital for patients in the control group (there was little variation over time for those who completed the partial hospitalization program). The repeated measures analysis of variance indicated significant differences between time points of assessment (Wilks’s lambda=0.64, F=4.2, df=2, 16, p<0.03). Exploring the polynomial components of this effect confirmed a significant quadratic effect (F=5.6, df=1, 17, p<0.03) and no significant linear effect (F<1.0, df=1, 17, n.s.).
Mann-Whitney tests revealed that patients who completed the partial hospitalization program had significantly fewer outpatient psychiatric consultations than did the control group patients at all follow-up points (24 months: U=59, p<0.001; 30 months: U=86, p<0.001; 36 months: U=73, p<0.001). Ten patients (52.6%) in the control group received some partial hospitalization treatment during the first 6 months of follow-up (range=3–60 days) as did 36.8% (N=7) during the rest of the follow-up period (range=8–60 days). No patient who completed the partial hospitalization program returned to partial hospitalization care either in the specialist setting or in the general psychiatric setting, which resulted in highly significant between-group differences at all follow-up points (24 months: U=99, p<0.001; 30 months: U=132, p<0.002; 36 months: U=132, p<0.002). Community center visits were measured in number of recorded attendances, which were significantly lower for the partial hospitalization group after the second follow-up point (30 months: U=91.5, p<0.001; 36 months: U=87, p<0.001). While there was a significant decline in the use of community center services in the partial hospitalization group over the follow-up period (Friedman’s χ2=8.4, df=2, p<0.02), a similar decline was not observed in the control group (Friedman’s χ2=3.7, df=2, n.s.).
Six borderline personality disorder patients who completed the partial hospitalization program (27.3%) and 14 control group patients (73.7%) were still taking medication at the end of the follow-up period (p<0.01, Fisher’s exact test). More important, while 63.2% (N=12) of the control subjects were receiving more than one class of drug (polypharmacy), only 9.1% (N=2) of the partial hospitalization patients were taking mood stabilizers and antidepressants at the end of follow-up (p<0.001, Fisher’s exact test). Cumulatively, 79.0% (N=15) of the control subjects and 36.4% (N=8) of the partial hospitalization patients had received medication during the follow-up period (p<0.007, Fisher’s exact test), with 68.4% (N=13) and 13.6% (N=3), respectively, taking more than one drug (p<0.001, Fisher’s exact test).
Self-Report Measures
A multivariate analog of the repeated measures analysis of covariance was applied to mean state and trait anxiety scores (Table 2). There was an overall significant decrease in state anxiety across both groups (Wilks’s lambda=0.70, F=2.5, df=5, 29, p<0.05). The similar pattern of decline was indicated by an insignificant interaction between group and time (Wilks’s lambda=0.73, F=2.1, df=5, 29, p<0.10). Patients who completed the partial hospitalization program scored substantially lower than control group subjects throughout the follow-up period after we controlled for baseline differences. The main effect of group was highly significant (F=34.9, df=1, 33, p<0.001). Pair-wise comparison revealed that the group differences were significant at all follow-up time points (p<0.001). For trait anxiety no significant overall decline was observed (Wilks’s lambda=0.79, F=1.6, df=5, 30, n.s.). The main effect of group only approached significance (F=3.5, df=1, 34, p<0.07), and pair-wise comparisons revealed significant differences at the 18-month (p<0.05) and 36-month (p<0.002) evaluations.
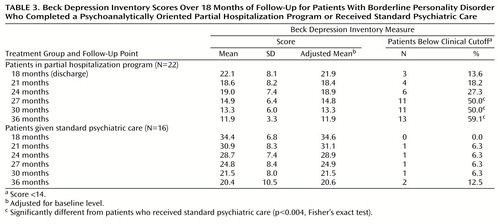
Mean scores on the Beck Depression Inventory are shown in Table 3. ANCOVA revealed no significant main effect of time (Wilks’s lambda=9.25, F<1.0, df=5, 31, n.s.). Patients who completed the partial hospitalization program reported themselves as significantly less depressed than did the control group subjects, and there was a powerful overall group difference (F=32.6, df=1, 35, p<0.001). The rate of decline in the two groups was comparable, and the group-by-time interaction was not significant (Wilks’s lambda=0.84, F=1.1, df=5, 31, n.s.). Pair-wise comparison revealed significant differences (p<0.001) in Beck Depression Inventory scores at all assessment points. At the end of the treatment phase, only three partial hospitalization patients and none of the control group subjects were below the clinical cutoff on the Beck Depression Inventory. The proportion of partial hospitalization patients who scored below 14 increased over the follow-up period, with significant between-group differences seen at the 27-, 30-, and 36-month evaluations (Table 3).
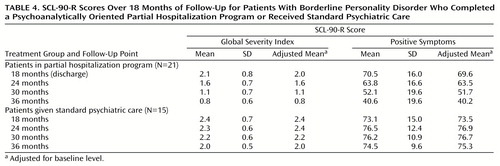
The mean scores on the global severity index scale of the SCL-90-R are summarized in Table 4. Overall, patients who completed the partial hospitalization program obtained significantly lower scores than did the control group patients (F=30.2, df=1, 33, p<0.001). There was a significant group-by-time interaction (Wilks’s lambda=0.59, F=7.3, df=3, 31, p<0.001). Polynomial decomposition of this interaction revealed a highly significant linear effect (F=19.4, df=1, 33, p<0.001), indicating that the increase in disparity between the two groups over the follow-up period was statistically significant. Pair-wise comparisons showed that global severity was not significantly different at the end of the treatment phase but was significantly lower for the partial hospitalization patients at the 24-month evaluation (p<0.001) and remained significantly lower throughout the follow-up period at the same level of significance.
Mean positive symptom scores are also summarized in Table 4. The main effect of group was highly significant (F=26.7, df=1, 33, p<0.001). The group-by-time interaction was also significant (Wilks’s lambda=0.54, F=8.9, df=3, 31, p<0.001). Polynomial decomposition showed a highly significant linear effect (F=27.6, df=1, 33, p<0.001). Pair-wise comparisons were not significant at the end of the treatment phase but were significant at the 24-month evaluation (p<0.01), and the difference increased over the follow-up period (p<0.001) as the number of reported symptoms declined in the partial hospitalization patients but remained constant in the control group.
The mean scores for the Inventory of Interpersonal Problems and the Social Adjustment Scale at the end of the treatment phase and the end of the follow-up period are summarized in Table 5. The differences between the groups were marked at posttreatment and increased over the follow-up period. The repeated measures ANCOVA performed on the posttreatment and follow-up data with pretreatment measure as covariate revealed a substantial group main effect (F=92.3, df=1, 37, p<0.001). The between-subject and repeated measures factor interaction was also significant (Wilks’s lambda=0.87, F=5.4, df=1, 37, p<0.03), indicating that the observed lowering of interpersonal problems over the follow-up period was statistically significant relative to the lack of change in the control group over the same period. Similarly, social adjustment problems reported on the Social Adjustment Scale improved during follow-up. The difference was significant both at posttreatment and at the 36-month evaluation. The ANCOVA (pretest Social Adjustment Scale total scores as covariates) yielded a significant group main effect (F=25.2, df=1, 36, p<0.001) as well as a significant interaction between group and time factors (Wilks’s lambda=0.86, F=6.0, df=1, 36, p<0.02).
Discussion
Long-term follow-up of patients treated in an 18-month psychoanalytically oriented partial hospitalization program showed not only that the substantial symptomatic and clinical gains made during treatment were maintained but also that there was additional improvement. The continuing decline in symptom distress, the absence of major clinical problems, and the associated low admission rates and minimal acts of self-harm throughout the follow-up period suggest that the partial hospitalization patients developed the psychological capacities necessary to withstand the normal stresses and strains of everyday life. This is in keeping with the aims of psychoanalytically informed treatment.
Although acts of self-harm and a need for hospital admission continued in the control group, there was some evidence of symptomatic improvement. This can be seen as spontaneous remission, but in light of the amount of treatment they received it seems appropriate to see these as attenuated treatment effects. Information about the natural course of borderline personality disorder over time is limited (13). If it is correct that supportive measures with medication lead to symptomatic improvement, this further emphasizes the need for future studies to be carefully controlled. Follow-up data in this study may be influenced by distortion of sampling, e.g., that nonimprovers kept returning to the service. But only three patients in the control group were partially lost to follow-up, there was minimal attrition in self-report measures for the remaining patients, and accurate clinical information about self-harm and hospital admissions was available for all patients. This limits the likelihood of sampling problems.
The recovery from depression is of interest. Although Gunderson and Phillips (14) concluded that borderline personality disorder and depression exhibit “a surprisingly weak and non-specific relationship,” the difficulty in evaluating the relationship between the disorders remains. In this study the improvement in depression was in the context of stability in other areas, such as social adjustment and interpersonal functioning, which suggests that depression in borderline personality disorder is an indicator of affect dysregulation rather than part of an affective disorder.
There was continued use of medication in both groups. Medication patterns are influenced by a large number of factors unrelated to a patient’s mental state, such as physician prescribing patterns, patient’s attitudes about medication, and frequency of visits to the psychiatrist’s office. However, the substantial differences observed between the groups would be hard to explain in terms of such artifacts alone. In Great Britain, individual prescribing patterns in the hospital are governed by guidelines, which are monitored. Individual physician choice plays an attenuated part. It seems that patients who completed the partial hospitalization program gave fewer indications to their physicians that they would still benefit from psychoactive medication. This is in keeping with their overall reduction in service utilization. The observed reduction in symptoms is even more impressive in the light of reduced use of medication.
While we do not have detailed data on cost-effectiveness, the gains made during and after treatment are important from a health care service perspective. The control group used more of all types of services monitored in this study. Borderline patients dominate psychiatric referrals to emergency rooms, particularly following impulsive acts of self-harm. The maintenance of a reduction in episodes of self-harm and suicide attempts and low rates of hospital admission in the borderline personality disorder patients who completed a psychoanalytically oriented partial hospitalization program (compared with patients who received standard psychiatric care) reduced to a minimal level the need for costly emergency treatment and expensive inpatient care. This suggests considerable savings following treatment.
This study has a number of limitations. The study group size was small, with additional loss of power from some attrition of subjects and consequent loss of self-report data at some time points. It is notable that no patient who completed the partial hospitalization program was lost to follow-up. We have no treatment integrity measure, making it difficult to identify the active ingredients of this treatment and make specific clinical recommendations. Treatment differences may be related to such factors as experience of staff with borderline patients and enthusiasm of the treatment team. Finally, we considered the possibility that the amount of staff time used by patients may be a factor, but patients in the control group received considerably more staff time during follow-up than the partial hospitalization patients as evidenced by service utilization statistics.
Further studies will be needed to establish if attendance at a partial hospitalization program is necessary for the effective delivery of psychotherapeutic help. The data from the control group demonstrated that mere attendance at a general psychiatric partial hospitalization program is insufficient to ensure enduring symptomatic change. But it remains possible that the psychotherapeutic intervention would have been equally effective had it been delivered in a modified form in an outpatient setting. This is the subject of an ongoing trial.
 |
 |
 |
 |
 |
Received Feb. 16, 2000; revisions received May 17 and July 12, 2000; accepted Aug. 10, 2000. From the Halliwick Day Unit, St. Ann’s Hospital, and the Psychoanalysis Unit, University College London, London. Address reprint requests to Dr. Bateman, Haringey Healthcare NHS Trust, Halliwick Day Unit, St. Ann’s Hospital, St. Ann’s Road, London N15 3TH, U.K.; [email protected] (e-mail).
1. Bateman A, Fonagy P: The effectiveness of partial hospitalization in the treatment of borderline personality disorder: a randomized controlled trial. Am J Psychiatry 1999; 156:1563–1569Google Scholar
2. Bateman AW, Fonagy P: Effectiveness of psychotherapeutic treatment of personality disorder. Br J Psychiatry 2000; 177:138–143Crossref, Medline, Google Scholar
3. Stevenson J, Meares R: An outcome study of psychotherapy for patients with borderline personality disorder. Am J Psychiatry 1992; 149:358–362Link, Google Scholar
4. Stevenson J, Meares R: Borderline patients at 5 year follow-up, in Proceedings of the 1995 Annual Congress of the Royal Australian and New Zealand College of Psychiatrists. Cairns, Australia, RANZP, 1995Google Scholar
5. Linehan MM, Heard HL, Armstrong HE: Naturalistic follow-up of a behavioral treatment for chronically parasuicidal borderline patients. Arch Gen Psychiatry 1993; 50:971–974Crossref, Medline, Google Scholar
6. Fonagy P, Target M: A contemporary psychoanalytical perspective: psychodynamic developmental therapy, in Psychosocial Treatments for Child and Adolescent Disorders: Empirically Based Strategies for Clinical Practice. Edited by Hibbs ED, Jensen PS. Washington, DC, American Psychological Association and National Institutes of Health, 1996, pp 619–638Google Scholar
7. Anderson EM, Lambert MJ: Short-term dynamically oriented psychotherapy: a review and meta-analysis. Clin Psychol Rev 1995; 15:503–514Crossref, Google Scholar
8. Derogatis LR: SCL-90-R: Administration, Scoring, and Procedures Manual, II. Towson, Md, Clinical Psychometric Research, 1983Google Scholar
9. Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J: An inventory for measuring depression. Arch Gen Psychiatry 1961; 4:561–571Crossref, Medline, Google Scholar
10. Spielberger CD, Gorsuch RL, Lushene RD: STAI Manual. Palo Alto, Calif, Consulting Psychologists Press, 1970Google Scholar
11. Cooper P, Osborn M, Gath D, Feggetter G: Evaluation of a modified self-report measure of social adjustment. Br J Psychiatry 1982; 141:68–75Crossref, Medline, Google Scholar
12. Horowitz LM, Rosenberg SE, Baer BA, Ureno G, Villasenor G: Inventory of interpersonal problems: psychometric properties and clinical applications. J Consult Clin Psychol 1988; 56:885–892Crossref, Medline, Google Scholar
13. Links P, Heslegrave R, Van Reekum R: Prospective follow-up study of borderline personality disorder: prognosis, prediction of outcome, and axis II comorbidity. Can J Psychiatry 1998; 43:265–270Crossref, Medline, Google Scholar
14. Gunderson JG, Phillips KA: A current view of the interface between borderline personality disorder and depression. Am J Psychiatry 1991; 148:967–975Link, Google Scholar



