Prospective Study of Posttraumatic Stress, Anxiety, and Depressive Reactions After Earthquake and Political Violence
Abstract
OBJECTIVE: The authors sought to assess the severity and longitudinal course of posttraumatic stress, anxiety, and depressive reactions among two groups of adults differentially exposed to severe and mild earthquake trauma and a third group exposed to severe violence. They also examined interrelationships among these reactions and predictors of outcome and compared posttraumatic stress disorder (PTSD) symptom category profile and course between those exposed to earthquake and those exposed to violence.METHOD: Seventy-eight non-treatment-seeking subjects were assessed with self-report instruments approximately 1.5 and 4.5 years after the 1988 Spitak earthquake in Armenia and the 1988 pogroms against Armenians in Azerbaijan.RESULTS: The two groups that had been exposed to severe trauma (earthquake or violence) had high initial and follow-up PTSD scores that did not remit over the 3-year interval. Overall, depressive symptoms subsided. Posttraumatic stress, anxiety, and depressive reactions were highly intercorrelated within and across both time intervals. No significant differences in PTSD severity, profile, or course were seen between subjects exposed to severe earthquake trauma versus those exposed to severe violence.CONCLUSIONS: After exposure to severe trauma, either an earthquake or violence, adults are at high risk of developing severe and chronic posttraumatic stress reactions that are associated with chronic anxiety and depressive reactions. Clinical evaluation and therapeutic intervention should include specific attention to these reactions. Early mental health intervention is recommended to prevent their chronicity.
On December 7, 1988, an earthquake with a magnitude of 6.9 on the Richter scale struck northern Armenia (population 3.5 million). The enormous destruction, injury, and loss of life sustained by cities in the earthquake zone has been described elsewhere (1). Gumri, the second largest city in Armenia, 20 miles from the epicenter, was approximately 50% destroyed and 90% severely damaged. At least 7% of the city’s total population of 280,000 people were killed during the earthquake. Yerevan, the capital of Armenia, 47 miles from the epicenter, sustained mild damage and no significant loss of life. Beginning in February 1988, pogroms were perpetrated against Armenians in Azerbaijan. In Sumgait, the most terrorized city, there was widespread persecution, murder, destruction of property, and looting. The majority of the survivors fled to Armenia, many of whom were relocated to Pyureghavan, a city near Yerevan. We have previously reported on high rates of severe posttraumatic stress reactions among adults exposed to the earthquake (2) and of adults exposed to the pogroms (3).
There have been only a few longitudinal studies that have specifically investigated posttraumatic stress disorder (PTSD) among adults after natural disasters. They indicate that PTSD can have a persistent course over many years. For example, MacFarlane (4), in a prospective study among firefighters after the 1983 Australian bushfires, reported rates of PTSD (calculated from the General Health Questionnaire) of 32%, 27%, and 30% at 4, 11, and 29 months after exposure, respectively. Green et al. (5) retrospectively evaluated the status of survivors after the 1972 Buffalo Creek flood. A 14-year follow-up indicated that the rate of PTSD dropped from 44% in 1974 to 28% in 1986. Shore et al. (6) reported an exposure-related onset of PTSD, generalized anxiety disorder, and depression after the 1980 Mount St. Helen’s volcanic eruption. Symptoms of depression and anxiety abated by 3 years, whereas symptoms of PTSD tended to persist longer. Duggan and Gunn (7) reported on a group of adults exposed to different types of disasters. At initial assessment within a year of the event, 39% met criteria for PTSD, with 23% meeting such criteria after 26 months.
Studies of the course of posttraumatic stress reactions among prisoners of war (POWs) have been mainly retrospective. They indicate that PTSD is prevalent and persistent over many years (8–13). For example, Engdahl et al. (9) reported that 45–50 years after the trauma, 84% of POWs held by the Japanese met lifetime criteria for PTSD, with 59% meeting current criteria. Sutker et al. (12) reported current rates of PTSD of 70% among World War II Pacific theater POWs 50 years after imprisonment. Differences in PTSD rates across these studies reflect differences in the severity of the traumatic experiences of the POWs.
Research on the course of PTSD among Vietnam veterans has found comparatively lower rates of current PTSD as compared with World War II POWs while also indicating that PTSD persists. Rates of PTSD have been found to vary with the nature and intensity of combat-related experiences (14–18). For example, Kulka et al. (18) reported a lifetime PTSD prevalence in male Vietnam veterans of 30% and a current incidence of 15% two decades after the war, indicating that approximately one-half of these cases have remained chronic.
Studies of the course of PTSD in the general population also indicate that PTSD symptoms tend to persist for years (15, 19–21). Kessler et al. (21) reported that one-third of individuals who developed PTSD after trauma did not experience remission of the disorder after 10 years. Davidson et al. (20) reported that PTSD became chronic in 46% of all patients who developed the disorder. Rape and assault, especially with injury, are associated with high rates and chronicity of PTSD (22–27). For example, Kilpatrick et al. (22) reported that 16.5% of women who had been raped continued to meet PTSD diagnostic criteria an average of 17 years afterward, with 10.5% of aggravated assault victims still having PTSD 10 years later. Studies among populations exposed to political violence and torture indicate that such experiences are associated with chronic PTSD (28–33). Carlson and Rosser-Hogan (31) reported that, among 50 randomly selected Cambodian refugees who had not been seeking treatment, 86% met DSM-III-R criteria for current PTSD about a decade after their traumatic experiences.
A majority of studies that have evaluated comorbid conditions with PTSD have found significant rates of comorbid depression and anxiety (6, 8–11, 15, 16, 18, 20, 21, 24, 27, 30, 31, 34, 35). For example, Kulka et al. (18) reported that among 15% of male Vietnam veterans with current PTSD, there was a total current comorbidity rate of approximately 50% for several other psychiatric disorders, including anxiety, depression, and substance abuse.
The highest reported rates of chronic PTSD have been among individuals exposed to extreme violence. It has been suggested that posttraumatic stress reactions to violence may differ from that to natural disaster (36, 37). Frederick (36) suggested that different psychological symptoms are associated with each type of trauma. Our previous study among adults exposed to the Spitak earthquake or the pogroms in Azerbaijan revealed high rates of severe posttraumatic stress reactions among these highly exposed individuals, irrespective of the type of trauma, with no difference in symptom profile between these groups (3). The present report is a 3-year follow-up (i.e., approximately 4.5 years after the trauma) of a subgroup of individuals included in the initial study. This report describes the severity, symptom profile, and course of PTSD, depression, and anxiety among these subjects.
Method
Subjects
A total of 78 ethnically Armenian subjects, who had not been seeking treatment, from three groups that had been previously studied approximately 1.5 years after their respective trauma were reevaluated 3 years later. The first group consisted of adults from Yerevan exposed to mild earthquake trauma, with no prior exposure to violence. For weeks after the earthquake, these individuals were exposed to graphic depictions of the earthquake destruction and subsequent plight of the victims. The second group consisted of adults from Gumri exposed to severe earthquake trauma, with no prior exposure to violence. Individuals from Gumri were exposed to extreme direct threats to their lives during the earthquake and heard screams from those who had been injured, burned, or trapped under collapsed buildings. Many had seen mutilated corpses exposed on the sidewalks or hanging from buildings for days following the earthquake. The third group consisted of adults from Sumgait exposed to mild earthquake trauma but severe violence in Azerbaijan. They experienced direct threats to their life for days and witnessed mutilation, torture, stabbing, and burning or murder of a family member or friend.
Subjects in the three groups included housewives, students, and a cross-section of working-class individuals, such as teachers, other employees of primary and secondary schools, factory workers, engineers, and hospital employees. Although the initial group of subjects did not constitute a representative sample of each population, attempts were made within each city to gather as diverse a group of individuals as possible. The initial sampling procedures have been described in detail elsewhere (2, 3). A subgroup that consisted of approximately one-half of the original subjects in Yerevan and Gumri (exposed to mild and severe earthquake trauma, respectively) was reinterviewed 4.5 years after the trauma. Every other subject from the original sample was selected. Whenever a subject was not located, the next individual on the list was selected. Two individuals from the original list in Gumri and three in Yerevan were not located. All subjects from the original Sumgait group (exposed to severe violence) were targeted for follow-up. Out of the original 25 subjects, five were not located, and one did not wish to be interviewed. All subjects included in this report had the study explained to them and gave written informed consent for their participation.
The 29 subjects (seven men and 22 women) from Yerevan exposed to mild earthquake trauma had a mean age of 29 years (SD=10). The 30 subjects (four men and 26 women) from Gumri exposed to severe earthquake trauma had a mean age of 43 years (SD=7). The 19 subjects from Sumgait (seven men and 12 women) exposed to severe violence had a mean age of 44 years (SD=15). The data were screened for the effect of sex on initial score and change in posttraumatic stress, anxiety, and depressive reaction scores between 1.5 and 4.5 years after the trauma. There was no effect of sex on any of the symptom measures 1.5 years after the trauma, nor was there an effect of sex on change in scores over time (all p values >0.10). Furthermore, there was no interaction of sex with city. On the basis of these results, men and women within each group were combined for the analyses.
Instruments
PTSD symptoms were evaluated using the PTSD Reaction Index (38). Items are rated on a 0–4 frequency scale. Scores for intrusion, avoidance, and arousal were derived by grouping items related to these categories on the basis of DSM-III-R criteria and calculating the mean item score for each symptom category (2, 3). Previously reported findings from 1.5 years after the earthquake among adults from Gumri and Yerevan indicated that a score of 40 or above on the PTSD Reaction Index identified 88% of subjects who met DSM-III-R criteria for PTSD. Ninety-five percent of those who did not meet these criteria had scores that fell below 40. Of the subjects who scored above the cutoff point of 40, 97% met DSM-III-R criteria for PTSD (2). At both time points, subjects from Yerevan and Gumri rated their posttraumatic stress reactions to the earthquake, while subjects from Sumgait rated their reactions to the violence. All subjects were evaluated for traumatic experiences that may have occurred in the 3-year interval between the two assessment points (1.5 and 4.5 years after the trauma). Intervening trauma assessed included exposure of the respondent to war, community violence, rape, serious accidental injury, and witnessing violence, suicide, or serious injury. Three subjects reported experiencing intervening trauma, including witnessing a son being shot, being in a serious automobile accident, and falling from a balcony. The pattern of change in PTSD Reaction Index scores for these subjects did not differ from that of their group as a whole.
Modified Hamilton Depression and Anxiety Scales
The Hamilton Depression Rating Scale (39) and the Hamilton Anxiety Rating Scale (40, 41) were adapted for use in this study as self-report measures. The 21-item Hamilton depression scale was adapted for the Armenian population by deleting two items that were considered nondiscriminatory. Item 13, which assesses general somatic symptoms, was excluded because almost all adults in the region had somatic complaints (backaches, muscle aches, and fatigability due to poor nutrition and extreme physical hardship). Item 17, which assesses insight into their illness, was excluded because people in the region were not deemed psychologically minded. One question was added regarding the onset of argumentativeness and aggression after the trauma. No questions on the Hamilton anxiety scale were added or deleted.
An independent study group of 28 adults from Gumri was used to determine the correlation of the clinician-administered and self-report evaluations. Two-thirds of this group were clinic patients with a spectrum of symptoms of varying severity, while the other third consisted of volunteers who had lived in Gumri during and after the earthquake and had not sought treatment. Half of the group was assessed first by clinical interview, followed by completion of the self-report form. The other half first completed the self-report form, then were clinically interviewed. The modes of administration were highly correlated (r=0.89, df=26, p<0.001 for the depression measures; r=0.87, df=26, p<0.001 for the anxiety measures).
Statistical Analyses
Changes in scores on the PTSD Reaction Index, the modified Hamilton anxiety scale, and the modified Hamilton depression scale were analyzed by means of repeated measures analyses of variance (ANOVAs), with group as a between-subject factor and time as a within-subject factor. Greenhouse-Geisser corrections were applied to within-subject comparisons. Changes in the percentage of subjects who met diagnostic criteria for PTSD over time were assessed by using McNemar’s test. Changes over time in scores on the intrusion, avoidance, and arousal subscales of the PTSD Reaction Index were evaluated by using repeated measures ANOVA with group as a between-subject factor and subscale as a within-subject factor. Relationships among the psychological variables were assessed by means of Pearson correlations.
Results
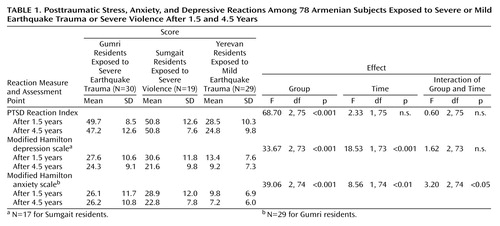
Table 1 shows the mean PTSD Reaction Index, the modified Hamilton depression scale, and the modified Hamilton anxiety scale scores for the three groups 1.5 and 4.5 years after their respective trauma, with repeated measures ANOVA tables for the three scales.
PTSD Reaction Index scores for the subjects from Gumri (exposed to severe earthquake trauma) and Sumgait (exposed to severe violence) did not differ from each other, while both were significantly higher than those of subjects from Yerevan (exposed to mild earthquake trauma) at both times (all p values <0.05, Scheff秮 PTSD Reaction Index scores did not change significantly over time, and there was no interaction of group and time.
Similarly, the modified Hamilton depression scale and the modified Hamilton anxiety scale scores of subjects from Gumri and Sumgait did not differ significantly from one another and were both significantly higher than the scores for subjects from Yerevan at both time intervals (all p values <0.05, Scheff秮 Overall, the depression scale scores improved significantly over time, with no significant difference in the pattern of improvement between groups. The Sumgait and Yerevan residents accounted for the overall improvement in the anxiety scale scores, as the anxiety scale scores of the Gumri residents remained the same.
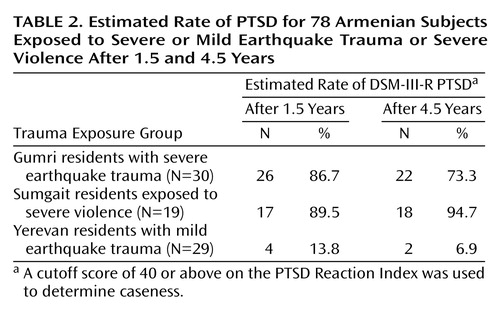
Table 2 shows the estimated percentage of subjects in each group who met DSM-III-R criteria for PTSD 1.5 and 4.5 years after their traumatic experience (i.e., scored 40 or above on the PTSD Reaction Index). A large percentage of subjects exposed to either severe earthquake trauma or severe violence was estimated to meet criteria for DSM-III-R PTSD at both time intervals.
Natural Disaster Versus Violence
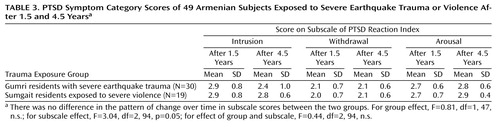
Comparisons were made between the subjects who experienced severe trauma as a result of either a natural disaster (Gumri earthquake victims) or violence (Sumgait pogrom victims) in regard to pattern of change in scores over time for intrusion, avoidance, and arousal PTSD symptom categories (Table 3). There was no difference in the pattern of change over time in subscale scores between the two groups.
Correlations and Prognostic Factors
Scores on the reaction measures were highly correlated with each other and across both assessment points (all p values <0.001, df=76). The PTSD Reaction Index score 1.5 years after the traumatic experience was highly correlated with the modified Hamilton depression scale (r=0.67) and the modified Hamilton anxiety scale (r=0.74) scores after 1.5 years. The depression and anxiety scale scores were also highly correlated 1.5 years after the trauma (r=0.79). The PTSD Reaction Index score after 4.5 years was highly correlated with the 1.5-year scores on the PTSD Reaction Index (r=0.70), the depression scale (r=0.64), and the anxiety scale (r=0.65). After 4.5 years, high correlations were found between scores on the PTSD Reaction Index and the depression scale (r=0.72), PTSD Reaction Index and the anxiety scale (r=0.79), and the depression and anxiety scales (r=0.81). The PTSD Reaction Index score after 4.5 years was highly correlated with the three PTSD Reaction Index subscale scores 1.5 years after the traumatic experience (intrusion: r=0.67; withdrawal: r=0.59; arousal: r=0.46). The best predictor of PTSD Reaction Index score at 4.5 years was PTSD Reaction Index score at 1.5 years. Finally, high correlations were found for the three PTSD Reaction Index subscale scores between 1.5 and 4.5 years after the trauma (intrusion: r=0.62; avoidance: r=0.62; arousal: r=0.42).
Discussion
The central finding of this prospective study was that individuals exposed to either extreme earthquake trauma or extreme violence did not show improvement of their severe PTSD symptoms between 1.5 and 4.5 years after their respective traumatic experiences. The PTSD symptoms of individuals exposed to mild earthquake trauma fell from the low-moderate to the upper-mild range.
The severity of PTSD symptoms among Gumri residents exposed to severe earthquake trauma and Sumgait residents exposed to severe violence are attributable to the extreme nature of their traumatic experiences. Nearly every adult in both groups experienced significant direct threats to their lives and witnessed horrifying sights for many days. The persistence of PTSD symptoms in these two groups is consistent with findings from other studies of extremely traumatized individuals, e.g., World War II POWs (12) and Cambodian refugees (31). The persistence of PTSD symptoms in these groups appeared to be related to pervasive trauma reminders that were embedded in circumstances after the trauma during this 3-year interval. These reminders continually reactivated symptoms (2). For those exposed to earthquake, ubiquitous undisposed debris and destroyed buildings, makeshift shoddy homes, and absence of family members (either due to death or employment elsewhere) served as ongoing reminders of earthquake-related trauma. For those exposed to violence, daily media news reports of the violence in Azerbaijan and the war in Karabagh served this same purpose.
The persistence of PTSD symptoms among adults in Gumri also appeared to be related to the unremitting severity of multiple stresses and adversities experienced after the earthquake. These included impoverished and crowded living conditions and lack of food, heat, electricity, and jobs. The demands associated with physical, emotional, and financial hardships appeared to interfere with efforts to contend with PTSD symptoms (2, 3). Conversely, continued PTSD symptoms seemed to give rise to secondary stresses and adversities, such as marital discord and disturbances in occupational and social functioning (42, 43), which compromised their ability to cope with PTSD symptoms.
The severity and persistence of depressive symptoms among earthquake victims in Gumri and pogrom-exposed subjects from Sumgait were most probably related to a number of factors. Losses of family members and friends, of irreplaceable treasured belongings and residence, and loss of community cohesion may have contributed to depression. Depressive symptoms were also related to chronic and pervasive stresses and adversities after the trauma. Finally, depressive symptoms may have arisen from traumatic experiences (14, 44) and persistent posttraumatic stress symptoms (45). As opposed to PTSD, depressive symptoms improved over time. Despite the improvement, the modified Hamilton depression scale scores of the Gumri and Sumgait residents remained relatively high. The improvement in depressive symptoms may have been due to subsidence of grief and rising hopes for social and economic recovery with the impending formation of an independent Armenian republic.
The severity and persistence of anxiety symptoms among those in Gumri exposed to severe earthquake trauma may be related to a number of factors. In the months after the earthquake, there were hundreds of aftershocks. Anticipatory anxiety associated with fears of recurrence during this acute period may have progressed into trait-like anxiety. Chronic PTSD symptoms (e.g., recurrent intrusive memories) and pervasive external trauma reminders may also have perpetuated anxiety. The overall improvement in anxiety symptoms was attributable to improvement in the Sumgait residents exposed to severe violence and the Yerevan residents exposed to mild earthquake trauma. The change in the Sumgait subjects may be attributable to the fact that during the follow-up interval, those in Sumgait lived in a somewhat improved environment, away from the direct threat of violence.
The present findings indicate that individuals exposed to two different types of extreme trauma, natural disaster and violence, are not differentiated by severity, symptom profile, or course of PTSD. It is likely that these similarities are due to common features of both types of trauma, which include experiencing significant direct threats to life and witnessing mutilating injuries or grotesque death. However, these findings should not be construed to indicate that psychological sequelae of natural disasters are identical to those of human-perpetrated violence. For example, revenge fantasies, shame, and feelings of defilement may be more prominent after rape. Evaluation of associated features of PTSD will allow for better determination of possible differences in course of posttraumatic reactions to man-made versus natural trauma.
The mean PTSD Reaction Index scores of the individuals exposed to severe trauma (either earthquake or violence) and the intercorrelations with the depression and anxiety scale scores indicate that severely traumatized individuals are at high risk for severe, chronic posttraumatic stress and associated anxiety and depressive reactions. Further studies are needed to determine whether the high intercorrelations among these reactions are due to 1) their sharing a common etiology (exposure to trauma); 2) PTSD being etiologic in the subsequent development of depression and anxiety; 3) symptoms of each serving to exacerbate one another; 4) posttrauma adversities that exacerbate PTSD while promoting the onset and aggravation of depression and anxiety; or 5) measurements of these reactions not being wholly independent because of an overlap of symptoms among these categories.
The present research design obviated some methodological problems that have confounded research regarding the course of PTSD. Being prospective, it circumvented problems with memory failure inherent in retrospective studies. North et al. (27) reported that 1-year follow-up evaluations would have failed to detect about one-third of PTSD cases at baseline. The present design included subjects who were not seeking treatment and who were ethnically, culturally, and religiously homogeneous.
The present findings indicate that clinical evaluation of individuals exposed to earthquake or violence should include specific evaluation of posttraumatic stress, anxiety, and depressive reactions and that intervention strategies should address these coexisting symptoms. Early mental health intervention may serve to prevent the chronicity of these reactions among victims of extreme trauma.
 |
 |
 |
Received Jan. 7, 1999; revisions received June 16 and Sept. 30, 1999; accepted Oct. 18, 1999. From the Trauma Psychiatry Program, Department of Psychiatry and Biobehavioral Sciences, University of California at Los Angeles; and the Armenian Relief Society Clinics of Armenia, Gumri. Address reprint requests to Dr. Goenjian, 501 Via La Selva, Redondo Beach, CA 90277.
1 Goenjian A: A mental health relief programme in Armenia after the 1988 earthquake: implementation and clinical observations. Br J Psychiatry 1993; 163:230–239Crossref, Medline, Google Scholar
2 Goenjian AK, Najarian LM, Pynoos RS, Steinberg AM, Manoukian G, Tavosian A, Fairbanks LA: Posttraumatic stress disorder in elderly and younger adults after the 1988 earthquake in Armenia. Am J Psychiatry 1994; 151:895–901Link, Google Scholar
3. Goenjian AK, Najarian LM, Pynoos RS, Steinberg AM, Petrosian P, Setrakyan S, Fairbanks LA: Posttraumatic stress reactions after single and double trauma. Acta Psychiatr Scand 1994; 90:214–221Crossref, Medline, Google Scholar
4. MacFarlane AC: The longitudinal course of posttraumatic morbidity: the range of outcomes and their predictors. J Nerv Ment Dis 1988; 176:30–39Crossref, Medline, Google Scholar
5. Green BL, Lindy JD, Grace MC, Glesser GC, Leonard AC, Korol M, Winget C: Buffalo Creek survivors in the second decade: stability of stress symptoms. Am J Orthopsychiatry 1990; 60:43–54Crossref, Medline, Google Scholar
6. Shore JH, Tatum EL, Vollmer WM: Psychiatric reactions to disaster: the Mount St Helens experience. Am J Psychiatry 1986; 143:590–595Link, Google Scholar
7. Duggan C, Gunn J: Medium-term course of disaster victims: a naturalistic follow-up. Br J Psychiatry 1995; 167:228–232Crossref, Medline, Google Scholar
8. Engdahl BE, Speed N, Eberly RA, Schwartz J: Comorbidity of psychiatric disorders and personality profiles of American WW II prisoners of war. J Nerv Ment Dis 1991; 179:181–187Crossref, Medline, Google Scholar
9. Engdahl B, Dikel TN, Eberly R, Blank A Jr: Posttraumatic stress disorder in a community group of former prisoners of war: a normative response to severe trauma. Am J Psychiatry 1997; 154:1576–1581Google Scholar
10. Goldstein G, van Kammen W, Shelly C, Miller DJ, van Kammen DP: Survivors of imprisonment in the Pacific theater during World War II. Am J Psychiatry 1987; 144:1210–1213Google Scholar
11. Kluznik JC, Speed N, vanValkenburg C, Magraw R: Forty-year follow-up of United States prisoners of war. Am J Psychiatry 1986; 143:1443–1446Google Scholar
12. Sutker PB, Allain AN Jr, Winstead DK: Psychopathology and psychiatric diagnoses of World War II Pacific theater prisoner of war survivors and combat veterans. Am J Psychiatry 1993; 150:240–245Link, Google Scholar
13. Solomon Z, Neria Y, Ohry A, Waysman M, Ginzburg K: PTSD among Israeli former prisoners of war and soldiers with combat stress reaction: a longitudinal study. Am J Psychiatry 1994; 151:554–559Link, Google Scholar
14. Boman B: The Vietnam veteran ten years on. Aust NZ J Psychiatry 1982; 16:107–127Crossref, Medline, Google Scholar
15. Helzer JE, Robins LN, McEvoy L: Posttraumatic stress disorder in the general population. N Engl J Med 1987; 317:1630–1634Google Scholar
16. Breslau N, Davis GC: Posttraumatic stress disorder: the etiologic specificity of wartime stressors. Am J Psychiatry 1987; 144:578–583Link, Google Scholar
17. Green BL, Lindy JD, Grace MC, Glesser GC: Multiple diagnosis in posttraumatic stress disorder: the role of war stressors. J Nerv Ment Dis 1989; 177:329–335Crossref, Medline, Google Scholar
18. Kulka RA, Schlenger WE, Fairbank JA, Hough RL, Jordan BK, Marmar CR, Weiss DS: Trauma and the Vietnam War Generation: Report of Findings From the National Vietnam Veterans Readjustment Study. New York, Brunner/Mazel, 1990Google Scholar
19. Breslau N, Kessler RC, Chilcoat HD, Schultz LR, Davis GC, Andreski P: Trauma and posttraumatic stress disorder in the community. Arch Gen Psychiatry 1998; 55:626–632Crossref, Medline, Google Scholar
20. Davidson JRT, Hughes D, Blazer D, George LK: Posttraumatic stress disorder in the community: an epidemiological study. Psychol Med 1991; 21:713–721Crossref, Medline, Google Scholar
21. Kessler RC, Sonnega A, Bromet E, Hughes M: Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry 1995; 52:1048–1060Google Scholar
22. Kilpatrick DG, Saunders BE, Veronen LJ, Best CL, Von JM: Criminal victimization: lifetime prevalence, reporting to police, and psychological impact. Crime and Delinquency 1987; 33:479–489Crossref, Google Scholar
23. Kilpatrick DG, Saunders BE, Amick-McMullan A, Best CL, Veronen LJ, Resnick HS: Victims and crime factors associated with the development of crime-related posttraumatic stress disorder. Behavior Therapy 1989; 20:199–214Crossref, Google Scholar
24. Breslau N, Davis GC, Adreski P, Peterson E: Traumatic events and posttraumatic stress disorder in an urban population of young adults. Arch Gen Psychiatry 1991; 48:216–222Crossref, Medline, Google Scholar
25. Foa EB: Trauma and women: course, predictors, and treatment. J Clin Psychiatry 1997; 5(suppl 9):25–28Google Scholar
26. Resnick HS, Kilpatrick DG, Dansky BS, Saunders BE, Best CL: Prevalence of civilian trauma and posttraumatic stress disorder in a representative national sample of women. J Consult Clin Psychol 1993; 61:984–991Crossref, Medline, Google Scholar
27. North CS, Smith EM, Spitznagel EL: One-year follow-up of survivors of a mass shooting. Am J Psychiatry 1997; 154:1696–1702Google Scholar
28. Mollica RF, Wyshak G, Lavelle J: The psychosocial impact of war trauma and torture on Southeast Asian refugees. Am J Psychiatry 1987; 144:1567–1572Google Scholar
29. Kinzey JD, Boehnlein JK, Leung PK, Moore LJ, Riley C, Smith D: The prevalence of posttraumatic stress disorder and its clinical significance among Southeast Asian refugees. Am J Psychiatry 1990; 147:913–917Link, Google Scholar
30. Ramsay R, Gorst-Unsworth C, Turner S: Psychiatric morbidity in survivors of organized state violence including torture. Br J Psychiatry 1993; 162:55–59Crossref, Medline, Google Scholar
31. Carlson EB, Rosser-Hogan R: Trauma experiences, posttraumatic stress, dissociation, and depression in Cambodian refugees. Am J Psychiatry 1991; 148:1548–1551Google Scholar
32. Mollica RF, Donelan K, Tor S, Lavelle J, Elias C, Frankel M, Blendon RJ: The effect of trauma and confinement on functional health and mental health status of Cambodians living in Thailand-Cambodia border camps. JAMA 1993; 270:581–586Crossref, Medline, Google Scholar
33. Weine SM, Vojvoda D, Becker DF, McGlashan TH, Hodzic E, Laub D, Hyman L, Sawyer M, Lazrove S: PTSD symptoms in Bosnian refugees 1 year after resettlement in the United States. Am J Psychiatry 1998; 155:562–564Link, Google Scholar
34. Breslau N, Davis GC, Peterson GL, Schultz L: Psychiatric sequelae of posttraumatic stress disorder in women. Arch Gen Psychiatry 1997; 54:81–87Crossref, Medline, Google Scholar
35. Engdahl B, Dikel TN, Eberly R, Blank A Jr: Comorbidity and course of psychiatric disorders in a community sample of former prisoners of war. Am J Psychiatry 1998; 155:1740–1745Google Scholar
36. Frederick C: Effects of natural vs human-induced violence upon victims, in Evaluation and Change: Services for Survivors. Edited by Kivens L. Minneapolis, Minneapolis Medical Research Foundation, 1980, pp 71–75Google Scholar
37. Madakasira S, O’Brien KF: Acute posttraumatic disorder in victims of a natural disaster. J Nerv Ment Dis 1987; 175:286–290Crossref, Medline, Google Scholar
38. Frederick CJ: Psychic trauma in victims of crime and terrorism, in Cataclysms, Crises, and Catastrophes: Psychology in Action. Edited by VandenBos GR, Bryant BK. Washington, DC, American Psychological Association, 1987, pp 55–108Google Scholar
39. Hamilton M: A rating scale for depression. J Neurol Neurosurg Psychiatry 1960; 23:56–62Crossref, Medline, Google Scholar
40. Hamilton M: The assessment of anxiety states by rating. Br J Med Psychol 1959; 32:50–55Crossref, Medline, Google Scholar
41. Hamilton M: Diagnosis and ratings of anxiety, in Studies of Anxiety. Br J Psychiatry (special publication) 1969; 3:76–79Google Scholar
42. Jordan BK, Marmar CR, Fairbank JA, Schlenger WE, Weiss DS, Hough RL, Kulka RA: Problems in families of male Vietnam veterans with posttraumatic stress disorder. J Consult Clin Psychol 1992; 60:916–926Crossref, Medline, Google Scholar
43. Carroll EM, Rueger DB, Foy DW, Donahoe CP Jr: Vietnam combat veterans with posttraumatic stress disorder: analysis of marital and cohabitating adjustment. J Abnorm Psychol 1985; 94:329–337Crossref, Medline, Google Scholar
44. Shalev AY, Freedman S, Peri T, Brandes D, Sahar T, Orr SP, Pitman RK: Prospective study of posttraumatic stress disorder and depression following trauma. Am J Psychiatry 1998; 155:630–637Link, Google Scholar
45. Goenjian AK, Pynoos RS, Steinberg AM, Najarian LM, Asarnow JR, Karayan I, Ghurabi M, Fairbanks LA: Psychiatric comorbidity in children after the 1988 earthquake in Armenia. J Am Acad Child Adoles Psychiatry 1995; 34:1174–1184Google Scholar



