Risk of Recurrence of Bipolar Disorder in Pregnant and Nonpregnant Women After Discontinuing Lithium Maintenance
Abstract
OBJECTIVE: Pregnancy poses major challenges for the treatment of bipolar disorder, and information to guide clinical care remains very sparse. The authors sought to determine the illness recurrence risk for women with bipolar disorder who discontinue lithium maintenance during pregnancy. METHOD: The authors retrospectively compared recurrence rates and survival functions for 101 women with DSM-IV bipolar disorder (68 type I, 33 type II) during pregnancy and postpartum (N=42) or during equivalent periods (weeks 1–40 and 41–64) for age-matched nonpregnant subjects (N=59) after either rapid (1–14 days) or gradual (15–30 days) discontinuation of lithium. Recurrence rates also were obtained for the year before discontinuing lithium. RESULTS: Rates of recurrence during the first 40 weeks after lithium discontinuation were similar for pregnant (52%) and nonpregnant women (58%) but had been much lower for both in the year before treatment was discontinued (21%). Among subjects who remained stable over the first 40 weeks after lithium discontinuation, postpartum recurrences were 2.9 times more frequent than recurrences in nonpregnant women during weeks 41–64 (70% versus 24%). Depressive or dysphoric-mixed episodes were more prevalent in pregnant than nonpregnant women (63% versus 38% of recurrences). Recurrence risk was greater after rapid than after gradual discontinuation, and for patients with more prior affective episodes, but was similar for diagnostic types I and II. CONCLUSIONS: Rates of recurrence during the first 40 weeks after lithium discontinuation were similar for pregnant and nonpregnant women but then sharply increased postpartum. Risk was much lower during preceding treatment and less with gradual discontinuation. Treatment planning for potentially pregnant women with bipolar disorder should consider the relative risks of fetal exposure to mood stabilizers versus the high recurrence risks after discontinuing lithium.
Bipolar disorder (types I and II) affects 1%–2% of the population and occurs commonly in women during childbearing years (1). Despite this relatively high prevalence, remarkably little is known about the risk of recurrence of bipolar illness during pregnancy, although major affective disorders, including psychotic forms, are quite common in pregnancy (2). The postpartum period is widely considered a high-risk period for recurrence of potentially severe and life-threatening recurrences of often-psychotic major affective illness, and thus it has received more systematic study (3–12). A traditional view is that pregnancy may protect against recurrence of major affective disorders or suicide. However, this impression is based on very limited data (13, 14), and several reports have suggested that pregnancy is not associated with altered recurrence risk in bipolar illness (15–17). Recurrences of mania and bipolar depression are not uncommon during pregnancy (18–21), and lithium has been used safely during pregnancy by many patients (22–25).
Management of pregnant women with bipolar disorder poses several clinical dilemmas. First, commonly employed antimanic agents (e.g., lithium, valproate, and carbamazepine) all carry some fetal teratogenic risk in early pregnancy and potential adverse effects during late pregnancy, labor, and delivery (26–33). Second, the impact of untreated psychiatric illness during pregnancy often appears to be discounted in decisions regarding maintaining or discontinuing a mood stabilizer. Finally, interruption, especially abruptly, of ongoing treatment with lithium—and perhaps other mood stabilizers—is associated with high risk of early relapse that can exceed rates predicted by the natural history of untreated manic-depressive illness (34–38) and may contribute to higher suicidal risk (39, 40). However, optimal clinical management of pregnant women with bipolar disorder only recently has begun to be examined critically. Treatment guidelines can be further refined as predictions of risk for bipolar disorder recurrence during pregnancy improve (25, 31, 33, 41–43). Specifically, it remains to be established whether pregnancy is associated with either a greater or lower risk of recurrence of mania or bipolar depression and whether pregnant and nonpregnant women respond differently to treatment discontinuation.
We now report on a retrospective assessment of recurrence risk in gravid and nongravid women with DSM-IV bipolar I or II disorder who elected to discontinue lithium maintenance treatment. This is the first study to compare 1) bipolar disorder recurrence risk after lithium discontinuation at different rates in a substantial number of pregnant and nonpregnant women, and 2) recurrence rates after discontinuing lithium in pregnancy with the recurrence rates of the same patients in the period preceding treatment discontinuation.
METHOD
We examined the clinical course of DSM-IV bipolar I or II disorder in 42 pregnant and 59 nonpregnant women aged 16–50 years who discontinued lithium either rapidly (over 1–14 days) or gradually (15–30 days), as defined previously (35–37). The pregnant women discontinued treatment within 6 weeks of the date of conception. The subjects had an overall mean of 3.94 years (SD=3.40) of maintenance treatment. Subjects were obtained from the Perinatal and Reproductive Psychiatry Research Program at Massachusetts General Hospital in Boston and the Lucio Bini–Stanley Foundation Center for Mood Disorders Research in Cagliari, Sardinia. In addition, comparison data were obtained for the same women from the year before they discontinued lithium, as well as from another nine women who elected to continue lithium treatment throughout their pregnancy. Patients were advised of the relative risks of fetal exposure to psychotropic drugs and of recurrences of illness during maintenance treatment and after discontinuation of mood stabilizers, to the extent that these could be estimated (20, 26–33). In the nongravid comparison group, decisions regarding lithium discontinuation arose clinically, usually at the patient’s insistence after periods of relative euthymia (75% of cases) or in response to treatment-emergent adverse effects (25% of cases). All subjects provided informed consent for review and anonymous reporting of information pertaining to their clinical course. The study protocol was approved by the institutional review board at Massachusetts General and McLean Hospitals and by corresponding officials at the University of Cagliari Medical Center.
Demographic and clinical information was recorded systematically from semistructured interviews and review of clinical records. Recurrence was defined as a new episode of mania (or hypomania) or major depression that met DSM-IV criteria at any time during pregnancy or postpartum or within corresponding periods for nongravid women (weeks 1–40 and weeks 41–64, respectively), as well as during the year of maintenance treatment preceding lithium discontinuation.
Analyses included contingency tables (chi-square or Fisher’s exact p), analysis of variance (F), and Kaplan-Meier survival analysis (Mantel-Cox or Wilcoxon chi-square), determined with Statview-V programs for the Macintosh microcomputer (SAS Corp., Cary, N.C.). Data are means and standard deviations, survival-computed times (with standard errors), or proportions (with 95% confidence intervals [CI]), at stated degrees of freedom (df); statistical results yielding p>0.05 (two-tailed) were considered nonsignificant (n.s.). All clinical and analytical methods used have been detailed previously (37–39).
RESULTS
First, among women with bipolar illness who discontinued lithium maintenance treatment, comparisons were made between the 42 pregnant women followed throughout their pregnancy and for 24 weeks postpartum and the 59 nongravid women followed through equivalent periods (weeks 1–40 and 41–64). The pregnant and nonpregnant subjects were of similar age at illness onset (mean=22.72 years [SD=4.46] and mean=23.31 [SD=8.43], respectively) and at lithium discontinuation (mean=32.53 [SD=4.95] and mean=32.81 [SD=9.54]) (both F values ≤0.170, df=1, 99, n.s.). They also did not differ significantly in the proportion with bipolar I disorder (73.81% [N=31] and 62.71% [N=37]) or with respect to previous illness (proportion with four or more prior episodes: 64.29% [N=27] and 59.32% [N=35]; χ2=0.03–2.55, df=1, n.s.). However, a somewhat higher proportion of the pregnant women discontinued lithium rapidly (73.81% [N=31] versus 54.24% [N=32]; χ2=4.00, df=1, p=0.05).
Recurrence Risks After Lithium Discontinuation
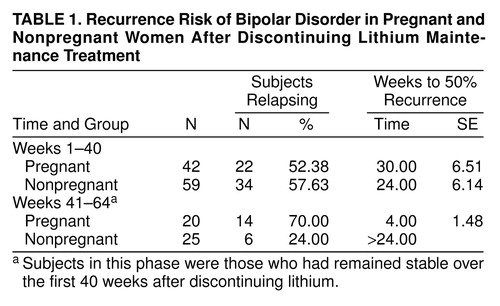
During the first 40 weeks after lithium discontinuation, there was little difference in recurrence rates between pregnant and nonpregnant women (52.38% [N=22 of 42] and 57.63% [N=34 of 59], respectively; χ2=0.273, df=1, n.s.) The overall recurrence rate was 55.45% (N=56 of 101). In contrast, among women who remained euthymic for 40 weeks after discontinuing lithium, significantly more pregnant subjects experienced a recurrence postpartum (70.00% [N=14 of 20]) than did the nonpregnant subjects during the corresponding time (24.00% [N=6 of 25]) (χ2=13.94, df=1, p=0.0002). None of the nine women with bipolar disorder who continued lithium treatment during pregnancy relapsed during weeks 1–40, but three (33.33%) experienced a recurrence soon after delivery (all within 2 weeks) despite continued maintenance treatment.
Over the entire 64-week period of risk after lithium discontinuation, recurrences were very common for both the pregnant/postpartum and the nonpregnant women (85.71% [N=36 of 42] and 67.80% [N=40 of 59], respectively). Among all subjects, the polarity of recurrent episodes was as follows: manic or hypomanic, 50.00%; depressive, 39.74%; and mixed-dysphoric, 10.26%. Among the pregnant subjects, the proportion of depressive or mixed episodes was similar during pregnancy and the postpartum period (63.64% and 62.50%, respectively; χ2=1.19, df=1, n.s.). However, depressive/mixed-dysphoric episodes were significantly more common among the pregnant/postpartum women than in nongravid subjects (63.16% versus 37.50% of episodes; χ2=5.13, df=1, p=0.02).
Survival Analyses
Kaplan-Meier survival functions over the initial 40 weeks after discontinuation of lithium maintenance treatment were compared for the pregnant and nonpregnant women (figure 1, table 1). The resulting computed time to 50% risk was 30.00 weeks (SE=6.51) in the pregnant women (43.92% remained stable throughout pregnancy without lithium) versus 24.00 weeks (SE=6.14) in nonpregnant women (of whom 42.37% remained stable for 40 weeks without lithium). These differences were not significant (χ2=0.057, df=1, n.s.; table 1). Secondary analyses based on matching for rapid discontinuation also did not reveal significant differences in recurrence risks between pregnant and nonpregnant women in the first 40 weeks after discontinuing treatment. Their respective computed times to 25% risk after rapid discontinuation were 10.00 weeks (SE=1.78) versus 8.00 weeks (SE=1.74) (χ2=2.54, df=1, n.s.). These findings suggest that pregnancy did not appreciably protect against risk associated with lithium discontinuation.
In contrast to the high rate of recurrences within 40 weeks after discontinuing lithium (55.45%), the recurrence rate among the same 101 women during the year before discontinuing was much lower (20.79% [N=21 of 101]). None of the nine pregnant women who elected to continue lithium treatment experienced a recurrence during their pregnancy. The survival function obtained from the pooled results of all 101 women during lithium maintenance, starting at 1 year before discontinuation, differed highly significantly from the survival function after discontinuation of lithium (time to 25% recurrence: >40 weeks during maintenance treatment versus 10.00 weeks [SE=2.62] after discontinuing lithium; χ2=36.20, df=1, p<0.0001). Serum lithium concentration during maintenance treatment averaged 0.620 meq/liter (SD=0.125).
Additional survival analyses were carried out among pregnant (N=20) and nonpregnant women (N=25) who remained stable throughout the first 40 weeks after stopping lithium (excluding two cases with episodes in both pregnancy and the puerperium). In contrast to the very similar early recurrence risk seen during weeks 1–40, recurrences of mania or depression in weeks 41–64 after discontinuing lithium were much greater in postpartum women. Computed time to 50% recurrence risk was only 4.00 weeks (SE=1.48) after pregnancy and indeterminate (>24 weeks) in women who had not been pregnant. Only 30.00% of 20 women without recurrence during pregnancy remained stable postpartum, but 76.00% of 25 nonpregnant comparison subjects remained stable through the additional 6 months of follow-up (by survival analysis, χ2=22.00, df=1, p<0.0001) (figure 1, table 1).
Rapidity of Lithium Discontinuation Effects
Because of the small number of pregnant patients who discontinued gradually, all subjects (gravid and nongravid) were pooled to evaluate the effect of lithium discontinuation rate. Only weeks 1–40 were considered because of the profound difference in risks in postpartum women versus nongravid women after 40 weeks. As shown in table 2, the resulting computed time to 25% recurrence risk was 2.50 times shorter after rapid than after gradual lithium discontinuation (χ2= 7.59, df=1, p=0.006). Moreover, six cases with uncertain discontinuation times yielded an intermediate computed time to 25% recurrence (12.00 weeks [SE=2.89]) between those with rapid and gradual discontinuation rates.
Clinical Factors Associated With Recurrences
The 56 women (pregnant and nongravid) who relapsed during the first 40 weeks after lithium discontinuation were compared to the 45 women who did not. No significant differences were found between these groups in several measures. These included age at onset (F=1.39, df=1, 99, n.s.), years of illness (F=3.76, df=1, 99, n.s.), and proportion of diagnostic subtypes (χ2=0.31, df=1, n.s.). There were also no relationships of these factors to relapse risk at weeks 41–64 (not shown). However, at weeks 1–40, patients with a relatively high number of prior episodes (four or more) had a significantly higher risk than those with 1–3 episodes (66.13% [N=41 of 62] versus 38.46% [N=15 of 39]; χ2=7.42, df=1, p=0.006), with a nonsignificant difference in the same direction at weeks 41–64 (83.87% [N=52 of 62] versus 69.23% [N=27 of 39]; χ2=3.01, df=1, p=0.08).
DISCUSSION
Information remains limited about the risk of recurrence of mood disorders during pregnancy or about the effects on maternal or child health of continuing or interrupting treatment. A recent study reported that pregnant women with preceding recurrent major depression were at significant risk for recurrence after antidepressant discontinuation (44). However, information regarding risk for recurrence in bipolar women after discontinuation of lithium or other mood stabilizers is very limited, and the effects of treatment discontinuation and acute psychiatric illness on fetal development are virtually unknown (45). The present study is the first systematic effort to quantify recurrence risk after lithium discontinuation during pregnancy, as well as postpartum, with comparisons to risk during previous lithium maintenance treatment. The study design is far from ideal in that it lacks randomization and prospective or blind assessment and may be affected by subtle mismatching of pregnant and nonpregnant women or by cultural differences between study sites. On the other hand, prospective randomization of women to continue or discontinue maintenance treatment during and after pregnancy for experimental purposes would present severe ethical and clinical challenges.
An important finding of this study was that survival functions after lithium discontinuation were very similar in pregnant and nonpregnant women with bipolar disorder. Recurrence rates also were similar for bipolar I and II subtypes but were higher in patients with a history of four or more prior episodes of illness and for those who underwent rapid discontinuation of lithium. These findings are consistent with our previously replicated findings (34–38) with broader study groups of men and mainly nonpregnant women in which we reported that recurrence risk was sharply elevated within the first several months after lithium discontinuation and was much greater after abrupt or rapid discontinuation.
The similar recurrence risks in pregnant and nonpregnant women within the first 40 weeks after stopping lithium may suggest that pregnancy is relatively “risk neutral” or unlikely to exert important protective or risk-enhancing effects. Alternatively, it may well be that lithium discontinuation represents a dominant stressor during the first months after stopping treatment that overshadows any more subtle effects of pregnancy. It is also possible that women were somewhat protected from recurrences of mania or bipolar depression by pregnancy but that such an effect was countered by other factors that contributed to a higher risk than in nonpregnant women, which is perhaps suggested by their experiencing a higher proportion of depressive or mixed episodes after discontinuing lithium than nonpregnant comparison subjects. Although pregnant women did not differ from nonpregnant subjects in onset age, duration of illness, or number of prior episodes, a higher proportion of pregnant women had discontinued lithium rapidly, consistent with fear of potential teratogenic effects of lithium (30). However, matching on discontinuation rate did not reveal significantly lower risks over time (1–40 weeks) in pregnant versus nonpregnant women. Nevertheless, a potential for effects of uncontrolled variables on the present findings indicates that further studies of the effects of pregnancy on recurrence risk in treated and untreated women with bipolar disorder are required, if ethical and clinically sound study designs can be developed.
Recurrence rates were much higher postpartum than during the equivalent period for nonpregnant women (weeks 41–64). This finding is consistent with many previous reports that the postpartum period brings particularly great risk for women with major affective and psychotic disorders (3–11). Postpartum recurrence risk can be reduced in pregnant women with bipolar disorder by lithium prophylaxis in late pregnancy or after delivery (46–51). In the present small study group, however, the protection afforded by continuing lithium was not complete, since three of nine pregnant women who elected to continue taking lithium suffered a postpartum recurrence. None of these nine women relapsed while continuing lithium throughout pregnancy, whereas 21 of the 101 women who later discontinued lithium experienced a recurrence in the year before their pregnancy while still being treated with lithium, perhaps suggesting a protective effect of pregnancy. All nine women who continued lithium throughout pregnancy delivered infants without major malformations. Nevertheless, the safety and prophylactic effectiveness of lithium and other alternative treatments, including newer anticonvulsants and antipsychotics, require further investigation in women with bipolar disorder, particularly after the developmentally critical first trimester of pregnancy and into the postpartum period (52, 53).
Gradually discontinuing lithium limited recurrence risk during the first 40 weeks after discontinuation. This finding supports our previous findings in a broader study group of bipolar disorder patients, which indicated that slower discontinuation of lithium can reduce, and not merely delay, recurrence risk (35–38), and perhaps suicide risk as well (39, 40). Abrupt discontinuation of other maintenance medications, including antipsychotics and antidepressants, has also been associated with a high, early relapse risk (54, 55). Pending further study of the effects of treatment discontinuation in pregnancy, clinicians managing pregnant women receiving maintenance psychotropic medicines should consider the rate of drug discontinuation as an important risk variable. Although gradual discontinuation of lithium into the first trimester of pregnancy results in greater fetal exposure during organogenesis, this vulnerability may be offset by reducing risk for potentially serious or life-threatening psychiatric illness that may follow rapid discontinuation of lithium, particularly in women with a history of multiple episodes of affective illness (55).
Appropriate concerns regarding the teratogenic effects of lithium have led to treatment practices that require reconsideration. For example, mood-stabilizing treatment is often discontinued abruptly after diagnosis or anticipation of pregnancy to minimize potential teratogenic risks. This practice needs to be balanced against the high risk of recurrence found soon after discontinuing treatment and unknown effects of drug discontinuation on early fetal development. The impact of untreated psychiatric illness on pregnant women and their offspring is often discounted, perhaps owing to greater concern about fetal malformations. Nevertheless, acute affective or psychotic illness in pregnancy places a woman and her fetus at risk due to impulsive or self-injurious behavior, substance abuse, or inattention to prenatal care, as well as increased exposure to multiple psychotropic drugs at relatively high doses. Moreover, the impact of mania or depression, as well as of drug withdrawal, on fetal development is poorly defined (56). Stress in pregnant animals can lead to sustained dysfunction of the hypothalamic-pituitary-adrenal system in their offspring (56–58), but a clinical counterpart of such effects has not yet been proved. However, untreated affective illness during pregnancy has been associated with adverse neonatal outcomes, including premature delivery, low birth weight, and lower Apgar ratings of neonatal status (33).
The present findings do not, by themselves, provide an adequate basis for proposing guidelines for the clinical management of pregnant women with bipolar disorder. However, they add compelling evidence that the risks of stopping maintenance lithium treatment, especially abruptly, are similar in pregnant women and in broader clinical samples. Clinicians who manage women with bipolar disorders who are planning to conceive should consider the high risk of relapse associated with lithium discontinuation in the overall risk/benefit assessment.
Received Jan. 13, 1999; revision received May 17, 1999; accepted June 30, 1999. From the Perinatal and Reproductive Psychiatry Service, Massachusetts General Hospital, Harvard Medical School, Boston; the Bipolar and Psychotic Disorders Program, McLean Hospital, Belmont, Mass.; and the Lucio Bini Center and Department of Psychology, University of Cagliari, Cagliari, Italy. Address reprint requests to Dr. Viguera, Perinatal and Reproductive Psychiatry Service, WACC-812, Massachusetts General Hospital, Fruit Street, Boston, MA 02114. Supported in part by NIMH grants MH-01609 (Dr. Viguera) and MH-47370 (Dr. Baldessarini); grants from the National Alliance for Research on Schizophrenia and Depression (NARSAD) (Drs. Viguera and Nonacs); awards from the Stanley Foundation and NARSAD (Drs. Cohen and Tondo); and grants from the Bruce J. Anderson Foundation and the Mailman Center Private Donors Neuropsychopharmacology Research Fund (Dr. Baldessarini).
 |
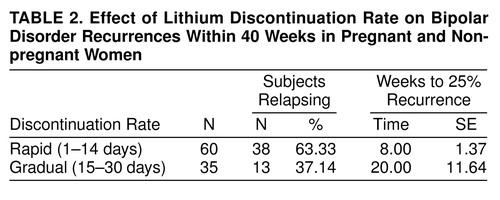 |
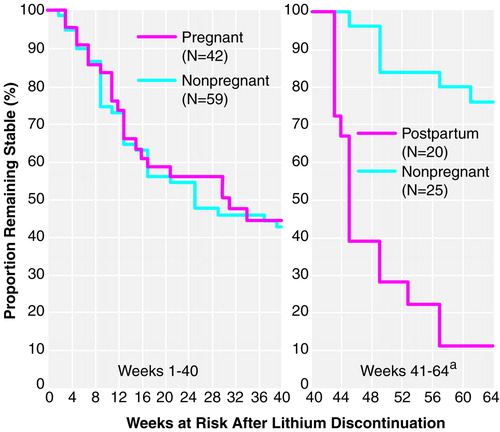
FIGURE 1. Kaplan-Meier Survival Analysis of Bipolar Disorder Recurrence Risk After Lithium Discontinuation During Pregnancy and Postpartum and During Equivalent Time Periods in Nonpregnant Women
aSubjects in this second analysis were those who had remained stable over the first 40 weeks after discontinuing lithium.
1. Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, Wittchen H-U, Kendler KS: Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity Survey. Arch Gen Psychiatry 1994; 51:8–19Crossref, Medline, Google Scholar
2. Steiner M: Perinatal mood disorders: position paper. Psychopharmacol Bull 1998; 34:301–306Medline, Google Scholar
3. Bratfos O, Haug JO: Puerperal mental disorders in manic-depressive females. Acta Psychiatr Scand 1966; 42:285–294Crossref, Medline, Google Scholar
4. Reich T, Winokur G: Postpartum psychoses in patients with manic depressive disease. J Nerv Ment Dis 1970; 151:60–68Crossref, Medline, Google Scholar
5. Brockington IF, Cernik KF, Schofield EM, Downing AR, Francis AF, Keelan C: Puerperal psychosis: phenomena and diagnosis. Arch Gen Psychiatry 1981; 38:829–833Crossref, Medline, Google Scholar
6. Paffenbarger RS: Epidemiological aspects of mental illness associated with childbirth, in Motherhood and Mental Illness. Edited by Brockington IF, Kumar R. New York, Grune & Stratton, 1982, pp 19–36Google Scholar
7. Davidson J, Robertson E: A follow-up study of post partum illness, 1946–1978. Acta Psychiatr Scand 1985; 71:451–457Crossref, Medline, Google Scholar
8. Meltzer ES, Kumar R: Puerperal mental illness, clinical features and classification: a study of 142 mother-and-baby admissions. Br J Psychiatry 1985; 147:647–654Crossref, Medline, Google Scholar
9. Kendell RE, Chalmers JC, Platz C: Epidemiology of puerperal psychoses. Br J Psychiatry 1987; 150:662–673Crossref, Medline, Google Scholar
10. Dean C, Williams RJ, Brockington IF: Is puerperal psychosis the same as bipolar manic-depressive disorder? a family study. Psychol Med 1989; 19:637–647Crossref, Medline, Google Scholar
11. Klompenhouwer JL, van Hulst AM: Classification of postpartum psychosis: a study of 250 mother and baby admissions in the Netherlands. Acta Psychiatr Scand 1991; 84:255–261Crossref, Medline, Google Scholar
12. Leibenluft E: Women with bipolar illness: clinical and research issues. Am J Psychiatry 1996; 153:163–173Link, Google Scholar
13. Zajieck E: Psychiatric problems during pregnancy, in Pregnancy: A Psychological and Social Study. Edited by Wolkind S, Zajicek E. London, Academic Press, 1981, pp 57–73Google Scholar
14. Marzuk PM, Tardiff K, Leon AC, Hirsch CS, Portera L, Hartwell N, Iqbal MI: Lower risk of suicide during pregnancy. Am J Psychiatry 1997; 154:122–123Link, Google Scholar
15. McNeil TF, Kaij L, Malmquist-Larsson A: Women with nonorganic psychosis: mental disturbance during pregnancy. Acta Psychiatr Scand 1984; 70:127–139Crossref, Medline, Google Scholar
16. Leir L, Kastrup M, Rafaelsen O: Psychiatric illness in relation to pregnancy and childbirth: diagnostic profiles, psychosocial and perinatal aspects. Nord Psykiatr Tidsskr 1989; 43:535–542Crossref, Google Scholar
17. Llewellyn AM, Stowe ZN, Nemeroff CB: Depression during pregnancy and the puerperium. J Clin Psychiatry 1997; 58(suppl 15):26–32Google Scholar
18. McNeil TF: A prospective study of postpartum psychoses in a high-risk group, 1: clinical characteristics of the current postpartum episodes. Acta Psychiatr Scand 1986; 74:205–216Crossref, Medline, Google Scholar
19. Krener P, Simmons MK, Hansen RL, Treat JN: Effect of pregnancy on psychosis: life circumstances and psychiatric symptoms. Int J Psychiatry Med 1989; 19:65–84Crossref, Medline, Google Scholar
20. Finnerty M, Levin Z, Miller LJ: Acute manic episodes in pregnancy. Am J Psychiatry 1996; 153:261–263Link, Google Scholar
21. Viguera AC, Nonacs R, Cohen LS: Risks of discontinuing maintenance treatment in pregnant women with bipolar disorder, in 1997 Annual Meeting New Research Program and Abstracts. Washington, DC, American Psychiatric Association, 1997, pp 97–98Google Scholar
22. Jacobson SJ, Jones K, Johnson K, Ceolin L, Kaur P, Sahn D, Donnenfeld AE, Rieder M, Santelli R, Smythe J: Prospective multicentre study of pregnancy outcome after lithium exposure during first trimester. Lancet 1992; 339:530–533Crossref, Medline, Google Scholar
23. Llewellyn A, Stowe ZN, Strader JR Jr: The use of lithium and management of women with bipolar disorder during pregnancy and lactation. J Clin Psychiatry 1998; 59(suppl 6):57–64Google Scholar
24. Schou M: Treating recurrent affective disorders during and after pregnancy: what can be taken safely? Drug Saf 1998; 18:143–152Google Scholar
25. Yonkers KA, Little BB, March D: Lithium during pregnancy. CNS Drugs 1998; 9:261–269Crossref, Medline, Google Scholar
26. Koch K, Hartman A, Jager-Roman E, Rating D, Helge H: Major malformations of children of epileptic parents—due to epilepsy or its therapy? in Epilepsy, Pregnancy and the Child. Edited by Janz D, Bossi L, Dam M, Helge H, Richens A, Schmidt D. New York, Raven Press, 1982, pp 313–316Google Scholar
27. Robert E, Guibaud P: Maternal valproic acid and congenital neural tube defects (letter). Lancet 1982; 2:937Crossref, Medline, Google Scholar
28. Rosa FW: Spina bifida in infants of women treated with carbamazepine during pregnancy. N Engl J Med 1991; 324:674–677Crossref, Medline, Google Scholar
29. Omtzigt JG, Los FJ, Grobbee DE, Pijpers L, Jahoda MG, Brandenburg H, Stewart PA, Gaillard HL, Sachs ES, Wladimiroff JW, Lindhout D: The risk of spina bifida aperta after first-trimester exposure to valproate in a prenatal cohort. Neurology 1992; 42(suppl 5):119–125Google Scholar
30. Cohen LS, Friedman JM, Jefferson JW, Johnson EM, Weiner ML: A reevaluation of risk of in utero exposure to lithium. JAMA 1994; 271:146–150Crossref, Medline, Google Scholar
31. Altshuler LL, Cohen L, Szuba MP, Burt VK, Gitlin M, Mintz J: Pharmacologic management of psychiatric illness during pregnancy: dilemmas and guidelines. Am J Psychiatry 1996; 153:592–606Link, Google Scholar
32. Briggs GG, Freeman RK, Yaffe S: Drugs in Pregnancy and Lactation. Baltimore, Williams & Wilkins, 1997Google Scholar
33. Cohen LS, Rosenbaum JF: Psychotropic drug use during pregnancy: weighing the risks. J Clin Psychiatry 1998; 59(suppl 2):18–28Google Scholar
34. Suppes T, Baldessarini RJ, Faedda GL, Tohen M: Risk of recurrence following discontinuation of lithium treatment in bipolar disorder. Arch Gen Psychiatry 1991; 48:1082–1088Google Scholar
35. Faedda GL, Tondo L, Baldessarini RJ, Suppes T, Tohen M: Outcome after rapid vs gradual discontinuation of lithium treatment in bipolar disorders. Arch Gen Psychiatry 1993; 50:448–455Crossref, Medline, Google Scholar
36. Baldessarini RJ, Tondo L, Faedda GL, Suppes TR, Floris G, Rudas N: Effects of the rate of discontinuing lithium maintenance treatment in bipolar disorders. J Clin Psychiatry 1996; 57:441–448Crossref, Medline, Google Scholar
37. Baldessarini RJ, Tondo L, Floris G, Rudas N: Reduced morbidity after gradual discontinuation of lithium treatment for bipolar I and II disorders: a replication study. Am J Psychiatry 1997; 154:551–553Link, Google Scholar
38. Baldessarini RJ, Tondo L: Effects of lithium treatment in bipolar disorders and posttreatment-discontinuation recurrence risk. Clin Drug Investigation 1998; 15:337–351Crossref, Medline, Google Scholar
39. Tondo L, Baldessarini RJ, Hennen J, Floris G, Silvetti F, Tohen M, Rudas N: Lithium treatment and risk of suicidal behavior in bipolar disorder patients. J Clin Psychiatry 1998; 59:405–414Crossref, Medline, Google Scholar
40. Baldessarini RJ, Tondo L, Hennen J: Effects of lithium treatment and its discontinuation on suicidal behavior in bipolar manic-depressive disorders. J Clin Psychiatry 1999; 60(suppl 2):77–84Google Scholar
41. van Gent EM, Verhoeven WMA: Bipolar illness, lithium prophylaxis, and pregnancy. Pharmacopsychiatry 1992; 25:187–191Crossref, Medline, Google Scholar
42. Blehar MC: Gender differences in risk factors for mood and anxiety disorders: implications for clinical treatment research. Psychopharmacol Bull 1995; 31:687–691Medline, Google Scholar
43. Altshuler LL, Hendrick V, Cohen LS: Course of mood and anxiety disorders during pregnancy and the postpartum period. J Clin Psychiatry 1998; 59(suppl 2):29–33Google Scholar
44. Cohen LS, Robertson LM, Goldstein J, Sichel DA, Grush LR, Weinstock LS: Impact of pregnancy on risk of relapse of MDD, in 1997 Annual Meeting Syllabus and Proceedings Summary. Washington, DC, American Psychiatric Association, 1997, p 23–24Google Scholar
45. Hultman CM, Sparén P, Takei N, Murray RM, Cnattingius S: Prenatal and perinatal risk factors for schizophrenia, affective psychosis, and reactive psychosis of early onset: case-control study. Br Med J 1999; 318:421–426Crossref, Medline, Google Scholar
46. Targum SD, Davenport YB, Webster MJ: Postpartum mania in bipolar manic-depressive patients withdrawn from lithium carbonate. J Nerv Ment Dis 1979; 167:572–574Crossref, Medline, Google Scholar
47. Abou-Saleh MT, Coppen A: Puerperal affective disorders and response to lithium (letter). Br J Psychiatry 1983; 142:539Crossref, Medline, Google Scholar
48. Stewart DE: Prophylactic lithium in postpartum affective psychosis. J Nerv Ment Dis 1988; 176:485–489Crossref, Medline, Google Scholar
49. Stewart DE, Klompenhouwer JL, Kendell RE, van Hulst AM: Prophylactic lithium in puerperal psychosis: the experience of three centres. Br J Psychiatry 1991; 158:393–397Crossref, Medline, Google Scholar
50. Austin MPV: Puerperal affective psychoses: is there a case for lithium prophylaxis? Br J Psychiatry 1992; 161:692–694Google Scholar
51. Cohen LS, Sichel DA, Robertson LM, Heckscher E, Rosenbaum JF: Postpartum prophylaxis for women with bipolar disorder. Am J Psychiatry 1995; 152:1641–1645Google Scholar
52. Markovitz PJ, Calabrese JR: Use of anticonvulsants for manic depression in pregnancy (letter). Psychosomatics 1990; 31:118Crossref, Medline, Google Scholar
53. Wisner KL: Prevention of postpartum episodes in bipolar women, in 1998 Annual Meeting Syllabus and Proceedings Summary. Washington, DC, American Psychiatric Association, 1998, p 4Google Scholar
54. Viguera AC, Baldessarini RJ, Hegarty JD, van Kammen DP, Tohen M: Clinical risk following abrupt and gradual withdrawal of maintenance neuroleptic treatment. Arch Gen Psychiatry 1997; 54:49–55Crossref, Medline, Google Scholar
55. Viguera AC, Baldessarini RJ, Friedberg J: Discontinuing antidepressant treatment in major depression. Harv Rev Psychiatry 1998; 5:293–306Crossref, Medline, Google Scholar
56. Geddes J: Prenatal and perinatal risk factors for early onset schizophrenia, affective psychosis, and reactive psychosis. BMJ 1999; 318:426Crossref, Medline, Google Scholar
57. Plotsky PM, Meaney MJ: Early, postnatal experience alters hypothalamic corticotropin-releasing factor (CRF) mRNA, median eminence CRF content and stress-induced CRF release in adult rats. Brain Res Mol Brain Res 1993; 18:195–200Crossref, Medline, Google Scholar
58. Ladd CO, Owens MJ, Nemeroff CB: Persistent changes in corticotropin-releasing factor neuronal systems induced by maternal deprivation. Endocrinology 1996; 137:1212–1218Google Scholar



